Provider Section
Total Page:16
File Type:pdf, Size:1020Kb
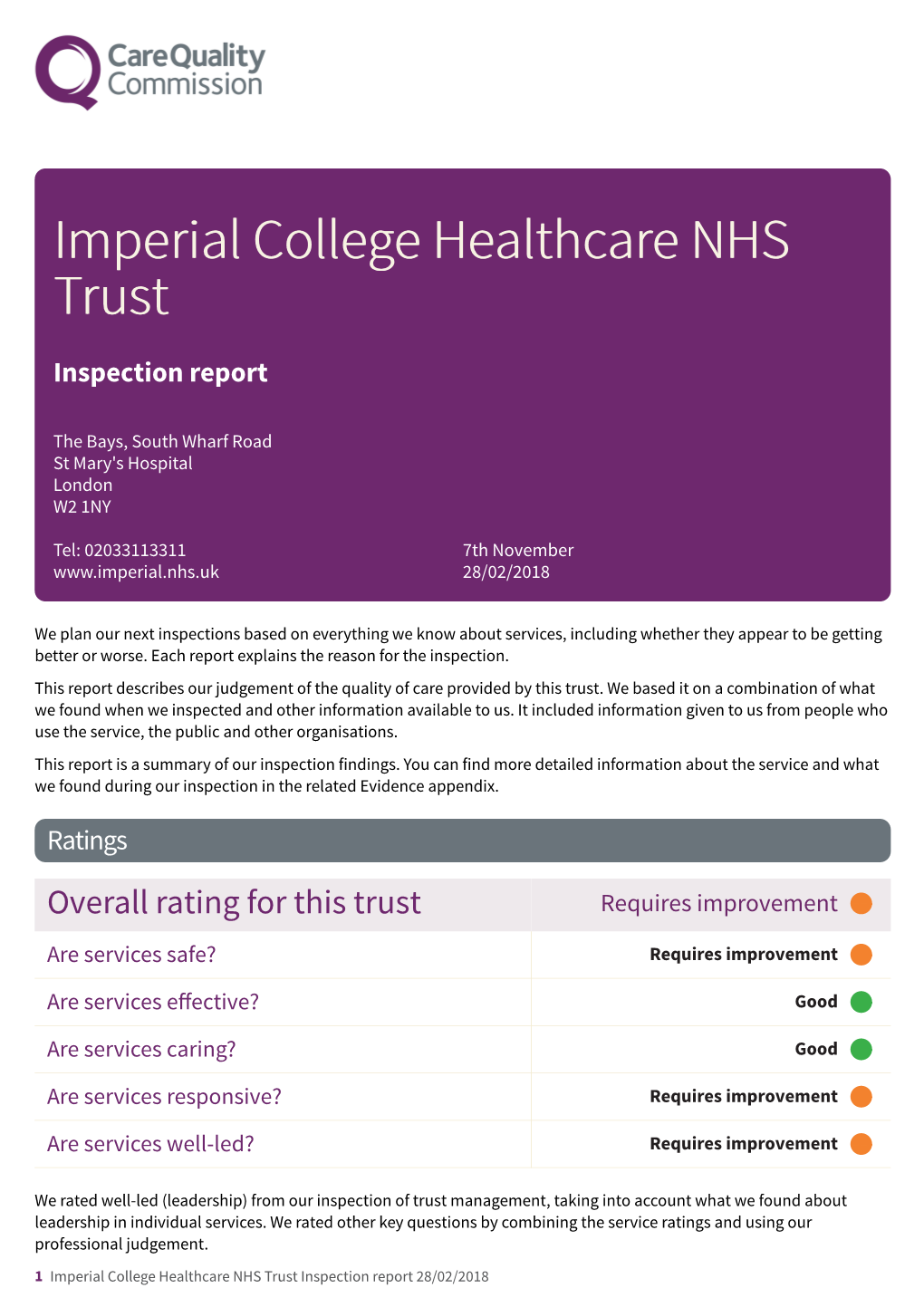
Load more
Recommended publications
-

Disorders of Thrombosis and Hemostasis in Pregnancy
Disorders of Thrombosis and Hemostasis in Pregnancy Hannah Cohen • Patrick O'Brien Editors Disorders of Thrombosis and Hemostasis in Pregnancy A Guide to Management Second Edition Editors Hannah Cohen Patrick O'Brien Department of Haematology Institute for Women’s Health University College London Hospitals University College London Hospitals NHS Foundation Trust NHS Foundation Trust London London UK UK ISBN 978-3-319-15119-9 ISBN 978-3-319-15120-5 (eBook) DOI 10.1007/978-3-319-15120-5 Library of Congress Control Number: 2015936083 Springer Cham Heidelberg New York Dordrecht London © Springer-Verlag London 2015 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specifi c statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The publisher, the authors and the editors are safe to assume that the advice and information in this book are believed to be true and accurate at the date of publication. Neither the publisher nor the authors or the editors give a warranty, express or implied, with respect to the material contained herein or for any errors or omissions that may have been made. -
How to Make a Comment Or Complaint
How to make a comment or complaint An easy-read guide for people with learning disabilities and their carers Making a comment We would like you to tell us what you think of our hospitals and the support you receive Please tell us if we can do better If you have had a good experience, we would like you to tell us about it This is how you can give us your comments: ●● Speak to someone from our patient advice and liaison service (PALS) ●● Use one of the hand-held computers on the ward or department you are visiting If you are not happy with the care or treatment you receive The Trust hopes to offer good support to all patients Sometimes things go wrong If you are not happy with the support you have received, you should tell us as soon as possible This booklet will tell you: ●● How to complain ●● The steps you will need to take ●● Who can give you support Step 1: how to make an informal complaint If you are not happy you should speak to the hospital staff caring for you Often things can be put right this way If you want to discuss the problem with someone else in the hospital, you can contact PALS, the patient advice and liaison service PALS can speak to the ward or department and try to put things right Using PALS, the patient advice and liaison service Every hospital has a patient advice and liaison team (PALS). They can help you with: ●● Any questions you have about your visit ●● Helping with to put right any problems during your visit ●● Speaking to the ward or department on your behalf We have patient advice and liaison services (PALS) -
An Introduction to Physiotherapy at Charing Cross Hospital
Musculoskeletal physiotherapy An introduction to physiotherapy Information for patients, relatives and carers What should I bring to my first appointment? Your physiotherapist will need to examine the affected area so please bring a pair of shorts and/or a vest top with you to wear, if appropriate. Please also bring a list of your current medication. If you are fasting please let us know and we will adapt your exercises accordingly. What will happen at my first appointment? Please arrive on time and check in at the kiosk in the physiotherapy department or at the reception desk. If you arrive late for your appointment we may not be able to see you as the clinic usually runs on time. Your appointment will last 30 to 60 minutes. Imperial College Healthcare NHS Trust is an academic health science centre. We may offer you an appointment with a student who works under the supervision of a senior member of staff. If you do not wish to participate in this training please let us know. It will not affect your treatment or care in any way. What if I cannot keep my appointment? If you cannot attend an appointment please let us know at least 24 hours in advance if possible by calling 020 3311 0333 between 08.00 and 17.00, Monday to Friday. The appointment can then be offered to another patient on the waiting list. If you reschedule more than one appointment you may be discharged back to the care of your GP. If you do not attend your appointment you may be discharged from our service in accordance with Trust policy. -

38149 OHE Pop TEXT 2/6/05 09:53 Page 1
38149 OHE Pop NEW COVER 2/6/05 09:53 Page 1 IMPROVING POPULATION HEALTH IN INDUSTRIALISED NATIONS HEALTH IMPROVING POPULATION SUSSEX IMPROVING POPULATION HEALTH IN INDUSTRIALISED NATIONS Based on papers delivered at the OHE Conference, London, 6 December 1999 Edited by Jon Sussex 38149 OHE Pop NEW COVER 2/6/05 09:53 Page 2 38149 OHE Pop TEXT 2/6/05 09:53 Page 1 IMPROVING POPULATION HEALTH IN INDUSTRIALISED NATIONS Based on papers delivered at the OHE Conference, London, 6 December 1999: ‘The Causes of Improved Population Health in Industrialised Nations: How will the 21st century differ from the 20th?’ Edited by Jon Sussex Office of Health Economics 12 Whitehall London SW1A 2DY www.ohe.org 38149 OHE Pop TEXT 2/6/05 09:53 Page 2 © September 2000. Office of Health Economics. Price £10.00 ISBN 1 899040 66 8 Printed by BSC Print Ltd, London. Office of Health Economics The Office of Health Economics (OHE) was founded in 1962. Its terms of reference are to: ● commission and undertake research on the economics of health and health care; ● collect and analyse health and health care data from the UK and other countries; ● disseminate the results of this work and stimulate discussion of them and their policy implications. The OHE is supported by an annual grant from the Association of the British Pharmaceutical Industry and by sales of its publications, and welcomes financial support from other bodies interested in its work. 2 38149 OHE Pop TEXT 2/6/05 09:53 Page 3 OFFICE OF HEALTH ECONOMICS Terms of Reference The Office of Health Economics (OHE) was founded in 1962. -

Imperialmatters31.Pdf
Imperial Matters 31 QX 6/2/08 08:26 Page 37 head ISSUE 31 WINTER 2007–08_THE UK’S NEW KIND OF HEALTHCARE CENTRE_LOOKING BACK AT A YEAR OF CELEBRATIONS_AN EVENING OF ROCK AND DUST_PLUS ALL THE NEWS FROM THE COLLEGE AND ALUMNI GROUPS IMPERIALmatters Alumni magazine of Imperial College London including the former Charing Cross and Westminster Medical School, Royal Postgraduate Medical School, St Mary’s Hospital Medical School and Wye College. ISSUE 31 WINTER 2007–08 in this issue ... 12 15 16 17 18 26 27 REGULAR FEATURES ALUMNI NEWS 1 editorial by Sir Richard Sykes 22 networks and groups 2 letters 26 Imperial’s international ambassadors 28 alumni focus NEWS 30 media mentions 3 Imperial news 31 books 4 faculty news 32 in memoriam 33 honours FEATURES 12 wrapping up our Centenary year_looking back at a year of celebrations 15 Centenary celebrations reunite alumni_at the Alumni Reunion 2007 16 dust rocks!_alumnus and Queen guitarist Brian May explains zodiacal dust 17 a rare vintage_the possibilities of Manchester Merlot and Sheffield Shiraz 18 a giant step for UK healthcare_a look at the UK’s first Academic Health Science Centre 20 Africa: health matters?_leading academics gather to discuss African healthcare 21 good advice_shaping the College’s future success in fundraising EXCLUSIVE ONLINE FEATURES new Department of Life Sciences_to encourage collaboration across the spectrum of life sciences happy 10th birthday medicine_celebrating 10 years since the Faculty’s formation schistosomiasis control initiative_awarded the Queen’s Anniversary Prize celebrating strong links with Asia_at the Asia Convocation IMPERIALmatters PRODUCED BY THE OFFICE OF ALUMNI AND DEVELOPMENT AND IMPERIAL COLLEGE COMMUNICATIONS EDITOR ZOË PERKINS MANAGING EDITOR SASKIA DANIEL EDITORIAL CONTRIBUTORS LIZ GREGSON, ABIGAIL SMITH, LAURA GALLAGHER, DANIELLE REEVES, COLIN SMITH AND NAOMI WESTON DESIGN JEFF EDEN PRINT PROLITHO LTD DISTRIBUTION PHAROS INTERNATIONAL IMPERIAL MATTERS IS PUBLISHED TWICE A YEAR. -

Grants • Arts • Volunteering • Fundraising Imperial Health Charity Newsletter Spring 2018
IMPERIAL HEALTH CHARITY NEWSLETTER SPRING 2018 GRANTS • ARTS • VOLUNTEERING • FUNDRAISING PAGES 6&7 - We did it! The More Smiles Appeal for the children’s intensive care unit at St Mary’s Hospital reaches its £2 million target INNOVATION INSPIRATION INTERVIEW Elderly care ward Resident artist Meet the eye transformed with joins the team to experts with a support from get creative with new vision for charity grant young patients patient care PAGE 2 PAGE 9 PAGE 10 CHARING CROSS • HAMMERSMITH • QUEEN CHARLOTTE’S & CHELSEA • ST MARY’S • WESTERN EYE Welcome to Focus Imperial Health Charity Chief Executive Ian Lush meets Senior Ward Sister Mojisola Hassan at the opening of the Welcome to the Spring refurbished Thistlethwayte ward at St Mary’s Hospital 2018 edition of Focus, the quarterly newsletter from Imperial Health Charity. I am delighted to announce that we have exceeded the £2 million target of our More Smiles Appeal! The money we have raised will go towards the expansion and refurbishment of the children’s intensive care unit at St Mary’s Hospital. The unit treats some of the country’s sickest children, providing a lifeline where other hospitals are simply not equipped to offer such complex care. We launched the appeal - in partnership with COSMIC charity - back in 2015 and it has taken an incredible amount of hard work and dedication to reach our ambitious target. There is not enough space here to recognise the many people who have helped us along the way. But to everyone who has made a donation or raised money - thank you. -

Report 29: the Impact of the COVID-19 Epidemic on All-Cause Attendances to Emergency Departments in Two Large London Hospitals: an Observational Study
1 July 2020 Imperial College COVID-19 response team Report 29: The impact of the COVID-19 epidemic on all-cause attendances to emergency departments in two large London hospitals: an observational study Michaela A C Vollmer, Sreejith Radhakrishnan, Mara D Kont, Seth Flaxman, Sam Bhatt, Ceire Costelloe, Kate Honeyford, Paul Aylin, Graham Cooke, Julian Redhead, Alison Sanders, Peter J White, Neil Ferguson, Katharina Hauck, Shevanthi Nayagam, Pablo N Perez-Guzman WHO Collaborating Centre for Infectious Disease Modelling MRC Centre for Global Infectious Disease Analysis Abdul Latif Jameel Institute for Disease and Emergency Analytics (J-IDEA) Division of Digestive Diseases, Department of Metabolism Digestion and Reproduction Imperial College London Imperial College Healthcare NHS Trust Imperial College London Department of Primary Care and Public Health Global Digital Health Unit Correspondence: [email protected] SUGGESTED CITATION Michaela A C Vollmer, Sreejith Radhakrishnan, Mara D Kont et al. The impact of the COVID-19 epidemic on all- cause attendances to emergency departments in two large London hospitals: an observational study. Imperial College London (30-05-2020), doi: https://doi.org/10.25561/80295. This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. DOI: https://doi.org/10.25561/80295 Page 1 of 22 1 July 2020 Imperial College COVID-19 response team Summary The health care system in England has been highly affected by the surge in demand due to patients afflicted by COVID-19. Yet the impact of the pandemic on the care seeking behaviour of patients and thus on Emergency department (ED) services is unknown, especially for non-COVID-19 related emergencies. -

Issue 175 • 21 March 2007
reporter www.imperial.ac.uk Issue 175 • 21 March 2007 Supporting a healthy outcome A key step forward for UK’s first Academic Health Science Centre centre pages early years grows darling pays a call up! Secretary of State for 44 new places for Trade and Industry visits Imperial children Imperial PAGE 3 PAGE 5 Sponsor Ben Support the Student in brief Opportunities Fund One for all and all for one! Imperial as One, the College’s black and minority ethnic race equality advisory group, was estab- lished in 2005 with the aim of promoting good race relations and supporting good practice throughout London Marathon the organisation. All staff are welcome to join. If you are interested in being involved or wish to Running for Opportunity receive further details, register your interest at [email protected]. Or why not have a taste of a paradise island by going along to their Ben Ryall is Imperial College’s first ever themed ‘Splash’ party this Friday 23 March? A London Marathon runner. He will be running buffet and entertainment will be provided. Contact Sunday 22 April to raise money for the Student Opportunities Fund. The Fund Clive Mendes on 020 7585 7809 to order your enables students from all over the world to tickets. receive a scholarship to support them for the duration of their course at Imperial. Established in 2003, the Student Opportunities Fund has awarded 60 scholarships. Visit Ben’s website to keep track of his weekly blog and training diary, see photos of Ben’s training, and keep him Research grant on the up on his toes by sending him good luck messages. -

Ealing Winter Resilience Health and Adult Social Care Scrutiny Panel 25 November 2015
EALING WINTER RESILIENCE HEALTH AND ADULT SOCIAL CARE SCRUTINY PANEL 25 NOVEMBER 2015 INTRODUCTION This report details the Ealing Winter Resilience plans and performance to date across the key providers of the local health and social care system. The key organisations contributing to this report are Ealing CCG, London Ambulance Service, London North West Hospitals NHS Trust, Imperial College Healthcare NHS Trust, and Ealing Adult Social Care. The plans are facilitated and co-ordinated through the Ealing System Resilience Group (SRG), also known as the Ealing Urgent Care Board which meets on a monthly basis. The report covers the capacity required to ensure the safe delivery of effective, high quality accessible integrated services. The paper also highlights the public and patient winter campaign to ensure the use of right service at the right time. The following summarises SRG resilience plan, demonstrating how Ealing CCG and Council are working with partners to deliver consistent 4 hour performance in 15/16. This document builds on identified SRG actions and takes account of the 8 High Impact Interventions (‘what good looks like’) from NHSE. 1 KEY SCHEMES The following summarises the key additional resources invested from system resilience funding and Better Care Fund to enable safe and efficient management during winter. These schemes are based on the winter debrief form 2014/15 and lessons learnt. Organisation Scheme £ 1 LNWHT Discharge Co-ordinators – 7day working - To facilitate £219,016 discharges on all the wards particularly for -

Imperial College Healthcare NHS Trust: Annual Report and Accounts 2018/19
Annual report 2018/19 Contents Welcome Welcome 3 I’m delighted to introduce the annual report for Performance report 5 Imperial College Healthcare NHS Trust for 2018/19 – the first to be published during my tenure as Overview 6 chair. I took up my new role in April 2019 and About the Trust 9 the achievements and challenges set out in these pages illustrate perfectly why I feel such pride Trust in numbers 12 and enthusiasm for the task ahead as we embrace Performance analysis corporate objectives 14 the best in patient care. Sustainability report 26 Imperial College Healthcare incorporates five hospitals and a growing portfolio of community-based and Performance against five domains of quality 28 digital services. We offer one of the broadest ranges Research discoveries 37 of acute and specialist care in the country to over one million patients a year. Working closely with partners Accountability report 39 across the healthcare system, we draw patients from Corporate governance report 40 across the UK and from around the world, as well as Paula Vennells CBE being privileged to serve those who live locally in Chair Statement of the chief executive officer’s some of north west London’s most diverse boroughs. responsibilities as the accountable officer of the Trust 45 Like the rest of the NHS and all developed healthcare systems, we are grappling with how best to respond Statement of directors’ responsibilities sustainably to growing needs. At the same time, we in respect of the accounts 45 are excited and inspired by the expanding possibilities Annual governance statement 48 of 21st century healthcare, which has the potential to improve patient care and outcomes – beyond what Care Quality Commission Regulatory Framework 50 we can imagine today. -

Trial of Isotretinoin and Calcitriol Monitored by CA 125 in Patients with Ovarian Cancer
Britsh Joumal of Cancer (1996) 74, 1479-1481 © 1996 Stockton Press All rights reserved 0007-0920/96 $12.00 Trial of isotretinoin and calcitriol monitored by CA 125 in patients with ovarian cancer GJS Rustin', TG Quinnell', J Johnson', H Clarke2, AE Nelstrop' and W Bollag3 'Department of Medical Oncology, Mount Vernon Centre for Cancer Treatment, Mount Vernon Hospital, Northwood, Middlesex HA6 2RN, UK; 2Department of Medical Oncology, Charing Cross Hospital, London W6 8RF, UK; 3Pharmaceutical Research, F Hoffmann-La Roche Ltd., CH-4002, Basle, Switzerland. Summary Twenty-two asymptomatic women with rising CA 125 levels after chemotherapy for ovarian cancer were entered into a trial of isotretinoin combined with calcitriol. Tumours were evaluated according to precise criteria based on serial CA 125 levels and by comparing regression slopes of CA 125 before and during therapy. There was no evidence based on CA 125 of any responses or significant change in tumour growth rate. Keywords: calcitriol; isotretinoin; CA 125; ovarian cancer Retinoids have been shown in vitro and in animal disease, defined as a CA 125 level that had risen to more than experiments to have inhibitory activity against a wide range 100 U ml-'; a Karnofsky performance status of at least 60; of solid tumours. The single-agent activity in man has been an ability to take oral medication; a serum creatinine less disappointing apart from in acute promyelocytic leukaemia than 1.5 x upper limit of normal; LFTs and bilirubin less (Smith et al., 1992). However, combination therapy with than 2 x upper limit of normal; serum calcium within normal interferon has shown considerable activity against cervical range; and no serious concomitant physical or psychiatric carcinoma (Lippman et al., 1992). -

Use of Non-Invasive Optical Analysis in Neurosurgery – a Pilot Study
Joint Research Compliance Office Use of non-invasive optical analysis in Neurosurgery – A pilot study Study Protocol 30/12/2019, Version 2.0 MAIN SPONSOR: Imperial College London FUNDERS: BrAin Tumour ReseArch STUDY COORDINATION CENTRE: Charing Cross Hospital – ImperiAl College NHS Trust IRAS Project ID: 258210 REC reference: Chief Investigator: Mr Kevin O’Neill, Dan Elson Co-investigators: Mr Giulio Anichini – Study coordinator, also responsible for patients’ recruitment, intra- operative data acquisition, data analysis, writing and submission of the research. Mr Neekhil Patel – Responsible for patients’ recruitment, intra-operative data acquisition, and data analysis Mr David Peterson - Responsible for patients’ recruitment and intra-operative data acquisition IRAS Project ID: 258210 Version 2.0, 30/12/2019 1 Joint Research Compliance Office Professor Dan Elson, Dr Iani Gayo, Dr Ioannis Gkouzionis, Dr Maria Leiloglou, Dr Vadzim Chalau, Dr Elizabeth Noble – Responsible for data processing and analysis Mr Babar Vaqas – Responsible for data analysis, writing and submission review Statistician: members of ICL / Hamlyn Center – to be defined Study Coordination Centre For general queries, supply of study documentation, and collection of data, please contact: Study Coordinator: Mr Giulio Anichini Address: Charing Cross Hospital, 3rd Floor South Corridor, Fulham Palace Rd, Hammersmith, London W6 8RF Registration: GMC 7422941 Tel: 020 3311 7678 E-mail: [email protected], [email protected] CLINICAL QUERIES Clinical queries should be directed to Mr Giulio Anichini, who will direct the query to the appropriate person IRAS Project ID: 258210 Version 2.0, 30/12/2019 2 Joint Research Compliance Office SPONSOR Imperial College of London is the main research Sponsor for this study.