Commemorative Program
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Texas First Lady Anita Perry
Texas First Lady Anita Perry For the past nine years, Texas First Lady Anita Perry has worked to promote a number of issues to benefit Texans from all walks of life, for Texans young and old and in all parts of the state. Active in the historic preservation of Texas’ cultural landmarks and communities, the First Lady plays a dynamic role in the Texas Historical Commission’s (THC) annual Main Street program, and travels the state educating Texans on the importance of restoration and preservation in revitalizing communities. In July 2008, the THC designated a new recognition to honor communities that demonstrate a high level of creativity and ingenuity. Named the First Lady’s Texas Treasures Award, Mrs. Perry serves as honorary chair of this endeavor to bring attention to small towns that work hard to preserve their authentic Texas sense of place. Along with Texas Governor Rick Perry, Mrs. Perry is committed to enhancing Texas’ expansion into international markets and promoting Texas as a prime location for business and trade. In that capacity, and as a dedicated representative of Texas tourism and economic development, the First Lady has led missions of Texas delegates to Japan, Germany and Spain. Mrs. Perry was recently honored by the Texas Travel Industry Association with the Silver Spur Award for her support of Texas travel. Promoting Texas tourism generates billions of dollars each year for the state’s economy. Following the devastating fire at the Governor’s Mansion in June 2008, the First Lady founded the Texas Governor’s Mansion Restoration Fund. Restoration of the 154-year-old Texas treasure will come from a public/private partnership and Mrs. -

Executive Order 13978 of January 18, 2021
6809 Federal Register Presidential Documents Vol. 86, No. 13 Friday, January 22, 2021 Title 3— Executive Order 13978 of January 18, 2021 The President Building the National Garden of American Heroes By the authority vested in me as President by the Constitution and the laws of the United States of America, it is hereby ordered as follows: Section 1. Background. In Executive Order 13934 of July 3, 2020 (Building and Rebuilding Monuments to American Heroes), I made it the policy of the United States to establish a statuary park named the National Garden of American Heroes (National Garden). To begin the process of building this new monument to our country’s greatness, I established the Interagency Task Force for Building and Rebuilding Monuments to American Heroes (Task Force) and directed its members to plan for construction of the National Garden. The Task Force has advised me it has completed the first phase of its work and is prepared to move forward. This order revises Executive Order 13934 and provides additional direction for the Task Force. Sec. 2. Purpose. The chronicles of our history show that America is a land of heroes. As I announced during my address at Mount Rushmore, the gates of a beautiful new garden will soon open to the public where the legends of America’s past will be remembered. The National Garden will be built to reflect the awesome splendor of our country’s timeless exceptionalism. It will be a place where citizens, young and old, can renew their vision of greatness and take up the challenge that I gave every American in my first address to Congress, to ‘‘[b]elieve in yourselves, believe in your future, and believe, once more, in America.’’ Across this Nation, belief in the greatness and goodness of America has come under attack in recent months and years by a dangerous anti-American extremism that seeks to dismantle our country’s history, institutions, and very identity. -

=, �- �- 190 3000 WEKZ-FM 180 15000 KBRK-FM Brookings, S
§ KSEL-FM Lubbock, Tex. 740 100000 § WKBl-FM a 550 740 § KDNC-FM Spokane,wash. 330 26500 WATP-FM �=, �- �- 190 3000 WEKZ-FM 180 15000 KBRK-FM Brookings, S. 0. 175 3000 § CKAT �::hoeda�fim. 5860 WPTN-FM Cookeville, Tenn. 210 3000 93.9 WJJM-FM Lewisburg, Tenn. 115 3000 WA TO-FM Oak Ridge, Tenn. 45 2500 WDBL-FM Springfield, Tenn. 215 3000 § KPOL-FM Los Angeles,Calif. 550 100000 KOLK-FM Del Rio, Tex. 68 3000 . 484 20000 §KLIS Palestine, Tex. 300 3000 F � �:st�M �f!\"t°:di� F�. 170 45000 t WXBB Warrenton, Va. 810 300 § WMTM-FM Moultrie, Ga. 165 28500 t WISS-FM Berlin, Wis. 155 3000 § WWEL Chicago, Ill. 170 6000 t WERL-FM Eagle River, Wis. 202 3000 § WFMW-FM Madisonville, Ky. 295 27000 WP RE-FM Prairie Du Chien, Wis. -46 3000 WCOU-FM Lewiston, Me. 250 13700 § CFRW-FM 6500 KWPM-FM West Plains Mo. 390 39000 § CKPR-FM r.:; ��ea�Oni. 48000 § *WNYC-FM New :tor\f.t Y. 220 5300 § CKMF-FM Montreal, Que. 41400 WCHN-FM Norwich, . Y. 250 3200 WBAG-FM BurlingtOn, N. C. 300 10000 94.5 § KSPI-FM Stillwater, Okla. 300 4000 Rapid City, 360 6000 Birmingham, 980 100000 KKLS-FM Corpus S. D. KSIX-FM Christi, Te,.;. 840 100000 WAPI-FM Ala. 620 100000 § KBUY-FM Ft. Worth, Tex. 430 100000 §KOOL-FM PhoeniK, ATiz. 310 50000 § KWLW San Angelo,Tex. 145 34000 F § KFIG Fresno, Calif. 90 7100 480 3500 KLIL Ukiah,Calif. 330 54000 WMEV-FM Ottawa,Marion, Ont.Va. 95000 Daytona § CFMO-FM § WNDB-FM Beach, Fla. -

Administration of George W. Bush, 2002 / Jan. 4
Administration of George W. Bush, 2002 / Jan. 4 Letter to Congressional Leaders Transmitting a Report on the National Emergency With Respect to the Taliban January 3, 2002 Dear Mr. Speaker: (Dear Mr. President:) Taliban that was declared in Executive As required by section 401(c) of the Na- Order 13129 of July 4, 1999. tional Emergencies Act, 50 U.S.C. 1641(c), Sincerely, and section 204(c) of the International GEORGE W. BUSH Emergency Economic Powers Act (IEEPA), 50 U.S.C. 1703(c), I transmit NOTE: Identical letters were sent to J. Den- herewith a 6-month periodic report on the nis Hastert, Speaker of the House of Rep- national emergency with respect to the resentatives, and Richard B. Cheney, Presi- dent of the Senate. Remarks on the Unveiling of the President’s Portrait in Austin, Texas January 4, 2002 Thank you. Thank you, Laura. You need I appreciate, Scott, your taking time to try to know, I listen to her every day. [Laugh- to figure me out. It’s a real pleasure for ter] Whatever success we’ve had is because me to work with you. I know it’s a chal- she’s constantly telling me what to do. lenge from your part, but it looks like you [Laughter] I’m proud of Laura, and I can’t did me justice, and I thank you. And it’s tell you what a great job she has done also good to see your brother, Stuart. The for America—you know that, yourself. But Gentlings are a part of the really fantastic she brings such a steadiness and a calm artistic community we have here in Texas. -

NINR History Book
NINR NATIONAL INSTITUTE OF NURSING RESEARCH PHILIP L. CANTELON, PhD NINR: Bringing Science To Life National Institute of Nursing Research (NINR) with Philip L. Cantelon National Institute of Nursing Research National Institutes of Health Publication date: September 2010 NIH Publication No. 10-7502 Library of Congress Control Number 2010929886 ISBN 978-0-9728874-8-9 Printed and bound in the United States of America TABLE OF CONTENTS Preface The National Institute of Nursing Research at NIH: Celebrating Twenty-five Years of Nursing Science .........................................v Acknowledgments ..................................................................................................ix Chapter One Origins of the National Institute of Nursing Research .................................1 Chapter Two Launching Nursing Science at NIH ..............................................................39 Chapter Three From Center to Institute: Nursing Research Comes of Age .....................65 Chapter Four From Nursing Research to Nursing Science ............................................. 113 Chapter Five Speaking the Language of Science ............................................................... 163 Epilogue The Transformation of Nursing Science ..................................................... 209 Appendices A. Oral History Interviews .......................................................................... 237 B. Photo Credits ........................................................................................... 239 -

View (E15309) Daenis Camiré, Jason Erb, Henrik Kehlet, Timothy Brennan, Ian Gilron
JMIR Research Protocols Ongoing Trials, Grant Proposals, Formative Research, Methods, Early Results Volume 9 (2020), Issue 1 ISSN: 1929-0748 Contents Protocols Factors Associated With Trial Completion and Adherence in App-Based N-of-1 Trials: Protocol for a Randomized Trial Evaluating Study Duration, Notification Level, and Meaningful Engagement in the Brain Boost Study (e16362) Jason Bobe, Jacqueline Buros, Eddye Golden, Matthew Johnson, Michael Jones, Bethany Percha, Ryan Viglizzo, Noah Zimmerman. 5 Caring Near and Far by Connecting Community-Based Clients and Family Member/Friend Caregivers Using Passive Remote Monitoring: Protocol for a Pragmatic Randomized Controlled Trial (e15027) Lorie Donelle, Sandra Regan, Michael Kerr, Merrick Zwarenstein, Michael Bauer, Grace Warner, Wanrudee Isaranuwatchai, Aleksandra Zecevic, Elizabeth Borycki, Dorothy Forbes, Lori Weeks, Bev Leipert, Emily Read. 14 Using Augmented Reality to Motivate Oral Hygiene Practice in Children: Protocol for the Development of a Serious Game (e10987) Susy Amantini, Alexandre Montilha, Bianca Antonelli, Kim Leite, Daniela Rios, Thiago Cruvinel, Natalino Lourenço Neto, Thais Oliveira, Maria Machado. 23 Relationship Education and HIV Prevention for Young Male Couples Administered Online via Videoconference: Protocol for a National Randomized Controlled Trial of 2GETHER (e15883) Michael Newcomb, Elissa Sarno, Emily Bettin, James Carey, Jody Ciolino, Ricky Hill, Christopher Garcia, Kathryn Macapagal, Brian Mustanski, Gregory Swann, Sarah Whitton. 33 Behavioral, Nutritional, -
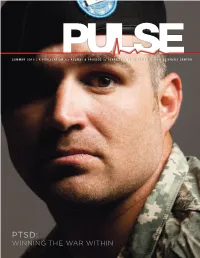
Winning the War Within Table of Contents
SUMMER 2012 | A PUBLICATION for ALUMNI & FRIENDS of TEXAS TECH UNIVERSITY HEALTH SCIENCES CENTER An End… A Beginning PTSD: Winning thE war Within TABLE of CONTENTS WINNING THE BATTLE WITHIN Today, “Fake Jake” is no more. Jake Bundy finally put him to rest after years of struggling 20 with post-traumatic stress disorder and is now ready for a career in occupational therapy. To help veterans like Bundy, the Paul L. Foster School of Medicine has signed on to the Joining Forces Initiative, coming to the aid of America’s military families. AT THE CROSSROADS OF ACADEMIA AND INDUSTRY 12 The Pine Street corridor has been transformed from a pawn shopper’s paradise to a health care harbor, but there’s more to this revitalization than meets the eye. Through the partnership between TTUHSC and the Abilene community, there is an opportunity to advance education, research and the region’s economy. MISSION ACCOMPLISHED 28 When Paul P. Brooke Jr., Ph.D., FACHE, became dean of the departments School of Allied Health Sciences, he approached the job with the past in mind. “I used to say I came out [to TTUHSC] to see 2 | President’s message what would happen if I put all of the things that I had learned in my military experiences into practice. In all due modesty, it 3 | ROUNDS Grand seems to have worked out pretty well.” 12 | DISCOVERIES Research and Scholarly Activities 31 | ROUNDS Alumni FRIDAY NIGHT LIFE 32 The play that Natalie Steadman, M.A.T., (SOAHS ’92) had 35 | ALUMNI PROFILES prepared for her entire career was over in less than five minutes, but it is one she will likely never forget. -

VITAE FALL 2016 Heidi E. Ajrami Division of Arts, Humanities, And
VITAE FALL 2016 Heidi E. Ajrami Division of Arts, Humanities, and Social Sciences English Dept. Phone: 361-573-3291 ext. 3370 The Victoria College Fax: 361-582-2577 2200 E. Red River St. [email protected] Victoria, TX 77901 EDUCATION Post-Graduate Certificate in TESOL, May 2007 Shenandoah University, Winchester, VA Master of Arts in English, May 1998 University of Nebraska at Omaha, Omaha, NE Bachelor of Arts in English, June 1989 (summa cum laude) Mercer University, Atlanta, GA COLLEGE TEACHING EXPERIENCE Spring 2003-present Victoria College, Professor of English, Division of Arts, Humanities, and Social Sciences Fall 1999-Fall 2002 Victoria College, Associate Professor of English, Humanities and Fine Arts Fall 1998-Spring 1999 Clarkson College, Adjunct Instructor, English, Humanities, Business, and Orientation PROFESSIONAL DEVELOPMENT SEAL Academy Spring 2016-Spring 2017 Syllabi Templates workshop Fall 2016 Windows Shortcuts workshop Fall 2016 Adobe workshop Fall 2015 Video Accessibility Basics workshop Fall 2015 FERPA training Fall 2015 PROFESSIONAL PRESENTATIONS AND MEMBERSHIPS Specifications Grading and Self-Regulated Learning Convocation Fall 2016 Specifications Grading and Self-Regulated Learning CAPE worshop Fall 2016 TCCTA membership Fall 2015-present COMMUNITY ACTIVITIES Relay for Life – annually since 2013 Foster family for Dorothy O’Connor Pet Adoption – Fall 2016 Christ’s Kitchen – Fall 2016 VITAE Jennifer Anderson English Department Office Tel: (361) 582-2577 The Victoria College Fax: (361) 582-2578 2200 E. Red River St. Victoria, TX 77901 [email protected] EDUCATION Master of English (Composition and Rhetoric), May 2003, Texas A&M University, Corpus Christi, TX. Bachelor of Humanities (English,) December 2001, University of Houston – Victoria, Victoria, TX. -

Inside This Issue
News ● Serving DX’ers since 1933 ● Volume 78, No. 19 ● February 14, 2011 ● (ISSN 0737-1639) Inside this issue . 2 … AM Switch 6 … Domestic DX Digest East 11 … DX Test Information 3 … Domestic DX Digest West 10 … International DX Digest 11 … Space Weather Forecast DX Tests Full details on our February DX DX News Publishing Schedule, Vol. 78 Tests may be found on page 11. Deadline Masthead 25 Apr. 1 Apr. 11 DX Test Schedule (All Times ELT) 20 Feb. 11 Feb. 21 26 Apr. 22 May 2 Sat 12 Feb KHMO-1070 0200-0205 21 Feb. 18 Feb. 28 27 May 27 June 6 0300-0305 22 Feb. 25 Mar. 7 28 July 1 July 11 Sat 12 Feb WLIQ-1530 0400-0500 23 Mar. 4 Mar. 14 29 Aug. 5 Aug. 15 Sat 19 Feb WLRB-1510 0200-0300 24 Mar. 18 Mar. 28 30 Sept. 9 Sept. 19 From the Publisher: ¡Snow más! There’s been The DX Time Machine a lot of snow across much of North America the 75 years ago – From the February 12, 1936 DX last couple weeks. So, if you’re stuck indoors, News – The DX test from CMBX Havana didn’t there’s not much else to do but to tune around work out, because the station announced during for all the stations running emergency coverage, the test that it had changed frequency to 1394 or whose antenna patterns are out of whack, kHz; member Bill Stone was working on an leading to unique DX opportunities. Send your “Across Canada DX Party” of DX tests from catches to DX News so we can all enjoy them! stations in every province, all on March 1. -
Welcome to the Texas Women's HALL of FAME 2014 PROGRAM
GCW_HOF_program_042514.indd 1 4/28/14 9:20 AM TEXAS Women’s hall of fAME Welcome to The Texas Women’s HALL OF FAME 2014 PROGRAM Welcome Carmen Pagan, Governor’s Commission for Women Chair Invocation Reverend Coby Shorter Presentation The Anita Thigpen Perry School of Nursing at Texas Tech University Keynote Address Governor Rick Perry Induction 2014 Texas Women’s Hall of Fame Honorees Closing 3 Texas Governor‘s Commission for Women GCW_HOF_program_042514.indd 2-3 4/28/14 9:20 AM TEXAS Women’s hall of fAME TEXAS Women’s hall of fAME The Texas Women’s HALL OF FAME AWARDS The Governor’s Commission for Women established the Texas Women’s Hall of Fame in 1984 to honor the remarkable achievements of Texas women while sharing their stories of great determination and innovation. The biennial awards highlight Texas women who have made significant contributions, often despite great odds. Nominations are submitted from across the state and reviewed by a panel of judges. Past honorees include first ladies, Olympic athletes and astronauts. The Texas Women’s HALL OF FAME 2014 Inductees The History of Our HALL OF FAME EXHIBIT In 2003, the Governor’s Commission for Women established a permanent exhibit for the Texas Women’s Hall of Fame on the campus of Texas Woman’s University in Denton, Texas. The exhibit features the biographies, photographs and video interviews of more than 100 notable women who have been chosen to represent the very best from our state. The exhibit is free of charge, and it is open to the public Monday through Friday from 8:00 a.m. -

Board Minutes
TEXAS TECH UNIVERSITY SYSTEM Lubbock, Texas Minutes Board of Regents February 25-26, 2010 Thursday, February 25, 2010.—The members of the Board of Regents of the Texas Tech University System convened at 8:30 am on Thursday, February 25, 2010, in Room 2241, Pharmacy Academic Center, 1310 Coulter Avenue, Amarillo, Texas, with the following in attendance: ATTENDANCE.— Regents present were Larry K. Anders, Chairman; L. Frederick “Rick” Francis; John Huffaker; Mickey L. Long; Kyle Miller, Student Regent; Nancy R. Neal; John Field Scovell; Daniel T. Serna; and Jerry Turner, Vice Chairman. Also participating at the opening of the meeting were Mr. Kent Hance, Chancellor, TTUS; Dr. Guy Bailey, President, TTU; Mr. Elmo Cavin, Interim President and Executive Vice President for Finance and Administration, TTUHSC; Dr. Joseph Rallo, President, ASU; Mr. Ben Lock, Executive Assistant to the Chancellor and Secretary of the Board of Regents, TTUS; Mr. Pat Campbell, Vice Chancellor and General Counsel, TTUS; Mr. Jim Brunjes, Vice Chancellor and Chief Financial Officer, TTUS; Dr. John Opperman, Vice Chancellor for Policy and Planning, TTUS; Dr. Kelly Overley, Vice Chancellor for Institutional Advancement, TTUS; Mr. Jodey Arrington, Chief of Staff, Chancellor’s Office, TTUS; Dr. Bob Smith, Provost and Senior Vice President for Academic Affairs, TTU; Dr. James Limbaugh, Interim Academic and Student Affairs Provost and Vice President, ASU; Dr. Rial Rolfe, Vice President for Academic Services, TTUHSC; Dr. Michael Shonrock, Senior Vice President for Student Affairs and Enrollment Management, TTU; and Mrs. Christina Martinez, Assistant Secretary to the Board of Regents, TTUS. I. CALL TO ORDER; CONVENE INTO OPEN SESSION OF THE BOARD.— Chairman Anders announced a quorum present and called the meeting to order. -

Licensing and Management System
Approved by OMB (Office of Management and Budget) 3060-0010 September 2019 (REFERENCE COPY - Not for submission) Commercial Broadcast Stations Biennial Ownership Report (FCC Form 323) File Number: 0000101820 Submit Date: 2020-01-29 FRN: 0017937822 Purpose: Commercial Broadcast Stations Biennial Ownership Report Status: Received Status Date: 01/29/2020 Filing Status: Active Section I - General Information 1. Respondent FRN Entity Name 0019985258 Oaktree Fund GP AIF, LLC Street City (and Country if non U. State ("NA" if non-U.S. Zip Address S. address) address) Code Phone Email c/o Oaktree Los Angeles CA 90071 +1 (213) tdavidson@akingump. Capital 830-6300 com Management, L.P. 333 South Grand Avenue, 28th Floor 2. Contact Name Organization Representative Tom Davidson Akin Gump Strauss Hauer & Feld LLP Street City (and Country if non U.S. Zip Address address) State Code Phone Email 2001 K St. Washington DC 20006 +1 (202) 887- tdavidson@akingump. NW 4011 com Not Applicable 3. Application Filing Fee 4. Nature of (a) Provide the following information about the Respondent: Respondent Relationship to stations/permits Entity required to file a Form 323 because it holds an attributable interest in one or more Licensees Nature of Respondent Limited liability company (b) Provide the following information about this report: Purpose Biennial "As of" date 10/01/2019 When filing a biennial ownership report or validating and resubmitting a prior biennial ownership report, this date must be Oct. 1 of the year in which this report is filed. 5. Licensee(s) and Station(s) Respondent is filing this report to cover the following Licensee(s) and station(s): Licensee/Permittee Name FRN Townsquare Media Licensee of Utica/Rome, Inc.