Article & Appendix
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genetic Diversity of Dengue Virus in Clinical Specimens from Bangkok
Tropical Medicine and Infectious Disease Article Genetic Diversity of Dengue Virus in Clinical Specimens from Bangkok, Thailand, during 2018–2020: Co-Circulation of All Four Serotypes with Multiple Genotypes and/or Clades Kanaporn Poltep 1,2,3 , Juthamas Phadungsombat 2,4 , Emi E. Nakayama 2,4 , Nathamon Kosoltanapiwat 1 , Borimas Hanboonkunupakarn 5, Witthawat Wiriyarat 3, Tatsuo Shioda 2,4,* and Pornsawan Leaungwutiwong 1,* 1 Department of Microbiology and Immunology, Faculty of Tropical Medicine, Mahidol University, Bangkok 10400, Thailand; [email protected] (K.P.); [email protected] (N.K.) 2 Mahidol-Osaka Center for Infectious Diseases (MOCID), Faculty of Tropical Medicine, Mahidol University, Bangkok 10400, Thailand; [email protected] (J.P.); [email protected] (E.E.N.) 3 The Monitoring and Surveillance Center for Zoonotic Diseases in Wildlife and Exotic Animals, Faculty of Veterinary Science, Mahidol University, Nakhon Pathom 73170, Thailand; [email protected] 4 Department of Viral Infections, Research Institute for Microbial Diseases (RIMD), Osaka University, Osaka 565-0871, Japan 5 Department of Clinical Tropical Medicine, Faculty of Tropical Medicine, Mahidol University, Bangkok 10400, Thailand; [email protected] * Correspondence: [email protected] (T.S.); [email protected] (P.L.) Citation: Poltep, K.; Phadungsombat, Abstract: Dengue is an arboviral disease highly endemic in Bangkok, Thailand. To characterize J.; Nakayama, E.E.; Kosoltanapiwat, the current genetic diversity of dengue virus (DENV), we recruited patients with suspected DENV N.; Hanboonkunupakarn, B.; infection at the Hospital for Tropical Diseases, Bangkok, during 2018–2020. We determined complete Wiriyarat, W.; Shioda, T.; nucleotide sequences of the DENV envelope region for 111 of 276 participant serum samples. -

2020 Taxonomic Update for Phylum Negarnaviricota (Riboviria: Orthornavirae), Including the Large Orders Bunyavirales and Mononegavirales
Archives of Virology https://doi.org/10.1007/s00705-020-04731-2 VIROLOGY DIVISION NEWS 2020 taxonomic update for phylum Negarnaviricota (Riboviria: Orthornavirae), including the large orders Bunyavirales and Mononegavirales Jens H. Kuhn1 · Scott Adkins2 · Daniela Alioto3 · Sergey V. Alkhovsky4 · Gaya K. Amarasinghe5 · Simon J. Anthony6,7 · Tatjana Avšič‑Županc8 · María A. Ayllón9,10 · Justin Bahl11 · Anne Balkema‑Buschmann12 · Matthew J. Ballinger13 · Tomáš Bartonička14 · Christopher Basler15 · Sina Bavari16 · Martin Beer17 · Dennis A. Bente18 · Éric Bergeron19 · Brian H. Bird20 · Carol Blair21 · Kim R. Blasdell22 · Steven B. Bradfute23 · Rachel Breyta24 · Thomas Briese25 · Paul A. Brown26 · Ursula J. Buchholz27 · Michael J. Buchmeier28 · Alexander Bukreyev18,29 · Felicity Burt30 · Nihal Buzkan31 · Charles H. Calisher32 · Mengji Cao33,34 · Inmaculada Casas35 · John Chamberlain36 · Kartik Chandran37 · Rémi N. Charrel38 · Biao Chen39 · Michela Chiumenti40 · Il‑Ryong Choi41 · J. Christopher S. Clegg42 · Ian Crozier43 · John V. da Graça44 · Elena Dal Bó45 · Alberto M. R. Dávila46 · Juan Carlos de la Torre47 · Xavier de Lamballerie38 · Rik L. de Swart48 · Patrick L. Di Bello49 · Nicholas Di Paola50 · Francesco Di Serio40 · Ralf G. Dietzgen51 · Michele Digiaro52 · Valerian V. Dolja53 · Olga Dolnik54 · Michael A. Drebot55 · Jan Felix Drexler56 · Ralf Dürrwald57 · Lucie Dufkova58 · William G. Dundon59 · W. Paul Duprex60 · John M. Dye50 · Andrew J. Easton61 · Hideki Ebihara62 · Toufc Elbeaino63 · Koray Ergünay64 · Jorlan Fernandes195 · Anthony R. Fooks65 · Pierre B. H. Formenty66 · Leonie F. Forth17 · Ron A. M. Fouchier48 · Juliana Freitas‑Astúa67 · Selma Gago‑Zachert68,69 · George Fú Gāo70 · María Laura García71 · Adolfo García‑Sastre72 · Aura R. Garrison50 · Aiah Gbakima73 · Tracey Goldstein74 · Jean‑Paul J. Gonzalez75,76 · Anthony Grifths77 · Martin H. Groschup12 · Stephan Günther78 · Alexandro Guterres195 · Roy A. -

Hantavirus Disease Were HPS Is More Common in Late Spring and Early Summer in Seropositive in One Study in the U.K
Hantavirus Importance Hantaviruses are a large group of viruses that circulate asymptomatically in Disease rodents, insectivores and bats, but sometimes cause illnesses in humans. Some of these agents can occur in laboratory rodents or pet rats. Clinical cases in humans vary in Hantavirus Fever, severity: some hantaviruses tend to cause mild disease, typically with complete recovery; others frequently cause serious illnesses with case fatality rates of 30% or Hemorrhagic Fever with Renal higher. Hantavirus infections in people are fairly common in parts of Asia, Europe and Syndrome (HFRS), Nephropathia South America, but they seem to be less frequent in North America. Hantaviruses may Epidemica (NE), Hantavirus occasionally infect animals other than their usual hosts; however, there is currently no Pulmonary Syndrome (HPS), evidence that they cause any illnesses in these animals, with the possible exception of Hantavirus Cardiopulmonary nonhuman primates. Syndrome, Hemorrhagic Nephrosonephritis, Epidemic Etiology Hemorrhagic Fever, Korean Hantaviruses are members of the genus Orthohantavirus in the family Hantaviridae Hemorrhagic Fever and order Bunyavirales. As of 2017, 41 species of hantaviruses had officially accepted names, but there is ongoing debate about which viruses should be considered discrete species, and additional viruses have been discovered but not yet classified. Different Last Updated: September 2018 viruses tend to be associated with the two major clinical syndromes in humans, hemorrhagic fever with renal syndrome (HFRS) and hantavirus pulmonary (or cardiopulmonary) syndrome (HPS). However, this distinction is not absolute: viruses that are usually associated with HFRS have been infrequently linked to HPS and vice versa. A mild form of HFRS in Europe is commonly called nephropathia epidemica. -

Taxonomy of the Order Bunyavirales: Update 2019
Archives of Virology (2019) 164:1949–1965 https://doi.org/10.1007/s00705-019-04253-6 VIROLOGY DIVISION NEWS Taxonomy of the order Bunyavirales: update 2019 Abulikemu Abudurexiti1 · Scott Adkins2 · Daniela Alioto3 · Sergey V. Alkhovsky4 · Tatjana Avšič‑Županc5 · Matthew J. Ballinger6 · Dennis A. Bente7 · Martin Beer8 · Éric Bergeron9 · Carol D. Blair10 · Thomas Briese11 · Michael J. Buchmeier12 · Felicity J. Burt13 · Charles H. Calisher10 · Chénchén Cháng14 · Rémi N. Charrel15 · Il Ryong Choi16 · J. Christopher S. Clegg17 · Juan Carlos de la Torre18 · Xavier de Lamballerie15 · Fēi Dèng19 · Francesco Di Serio20 · Michele Digiaro21 · Michael A. Drebot22 · Xiaˇoméi Duàn14 · Hideki Ebihara23 · Toufc Elbeaino21 · Koray Ergünay24 · Charles F. Fulhorst7 · Aura R. Garrison25 · George Fú Gāo26 · Jean‑Paul J. Gonzalez27 · Martin H. Groschup28 · Stephan Günther29 · Anne‑Lise Haenni30 · Roy A. Hall31 · Jussi Hepojoki32,33 · Roger Hewson34 · Zhìhóng Hú19 · Holly R. Hughes35 · Miranda Gilda Jonson36 · Sandra Junglen37,38 · Boris Klempa39 · Jonas Klingström40 · Chūn Kòu14 · Lies Laenen41,42 · Amy J. Lambert35 · Stanley A. Langevin43 · Dan Liu44 · Igor S. Lukashevich45 · Tāo Luò1 · Chuánwèi Lüˇ 19 · Piet Maes41 · William Marciel de Souza46 · Marco Marklewitz37,38 · Giovanni P. Martelli47 · Keita Matsuno48,49 · Nicole Mielke‑Ehret50 · Maria Minutolo3 · Ali Mirazimi51 · Abulimiti Moming14 · Hans‑Peter Mühlbach50 · Rayapati Naidu52 · Beatriz Navarro20 · Márcio Roberto Teixeira Nunes53 · Gustavo Palacios25 · Anna Papa54 · Alex Pauvolid‑Corrêa55 · Janusz T. Pawęska56,57 · Jié Qiáo19 · Sheli R. Radoshitzky25 · Renato O. Resende58 · Víctor Romanowski59 · Amadou Alpha Sall60 · Maria S. Salvato61 · Takahide Sasaya62 · Shū Shěn19 · Xiǎohóng Shí63 · Yukio Shirako64 · Peter Simmonds65 · Manuela Sironi66 · Jin‑Won Song67 · Jessica R. Spengler9 · Mark D. Stenglein68 · Zhèngyuán Sū19 · Sùróng Sūn14 · Shuāng Táng19 · Massimo Turina69 · Bó Wáng19 · Chéng Wáng1 · Huálín Wáng19 · Jūn Wáng19 · Tàiyún Wèi70 · Anna E. -

Domestically Acquired Seoul Virus Causing Hemophagocytic Lymphohistiocytosis—Washington, DC, 2018
applyparastyle “fig//caption/p[1]” parastyle “FigCapt” Open Forum Infectious Diseases BRIEF REPORT Domestically Acquired Seoul SEOV infection in humans has a mortality rate of <1%. In the SEOV outbreak among 183 rat owners in the United States Virus Causing Hemophagocytic and Canada in 2017, 24 (13.1%) had Seoul virus antibodies, 3 Lymphohistiocytosis—Washington, (12.5%) were hospitalized, and no deaths occurred [4]. DC, 2018 Hemophagocytic lymphohistiocytosis (HLH) is a rare im- mune disorder in which overactivity of white blood cells leads 1, 2 3 2 Bhagyashree Shastri, Aaron Kofman, Andrew Hennenfent, John D. Klena, to hemophagocytosis and can result in death. HLH may be Stuart Nicol,2 James C. Graziano,2 Maria Morales-Betoulle,2 Deborah Cannon,2 Agueda Maradiaga,3 Anthony Tran,4 and Sheena K. Ramdeen1 primary due to genetic causes or secondary due to cancers, 1Department of Infectious Diseases, Medstar Washington Hospital Center, Washington, autoimmune disorders, or infections. Although a variety of in- 2 DC, USA, Viral Special Pathogens Branch, Division of High-Consequence Pathogens and fections have been shown to cause HLH, studies have raised the Pathology, Centers for Disease Control and Prevention, Atlanta, Georgia, USA, 3Center for Policy, Planning and Evaluation, DC Department of Health, Washington, DC, USA, and 4Public possibility of HLH linked to HFRS, mostly due to PUUV- in- Health Laboratory, DC Department of Forensic Sciences, Washington, DC, USA duced HFRS (Puumala virus) [5, 6]. Although it has been shown that wild Norway rats on the east Seoul orthohantavirus (SEOV) infections, uncommonly re- coast of the United States can carry SEOV, it has never been ported in the United States, often result in mild illness. -

A Look Into Bunyavirales Genomes: Functions of Non-Structural (NS) Proteins
viruses Review A Look into Bunyavirales Genomes: Functions of Non-Structural (NS) Proteins Shanna S. Leventhal, Drew Wilson, Heinz Feldmann and David W. Hawman * Laboratory of Virology, Rocky Mountain Laboratories, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, MT 59840, USA; [email protected] (S.S.L.); [email protected] (D.W.); [email protected] (H.F.) * Correspondence: [email protected]; Tel.: +1-406-802-6120 Abstract: In 2016, the Bunyavirales order was established by the International Committee on Taxon- omy of Viruses (ICTV) to incorporate the increasing number of related viruses across 13 viral families. While diverse, four of the families (Peribunyaviridae, Nairoviridae, Hantaviridae, and Phenuiviridae) contain known human pathogens and share a similar tri-segmented, negative-sense RNA genomic organization. In addition to the nucleoprotein and envelope glycoproteins encoded by the small and medium segments, respectively, many of the viruses in these families also encode for non-structural (NS) NSs and NSm proteins. The NSs of Phenuiviridae is the most extensively studied as a host interferon antagonist, functioning through a variety of mechanisms seen throughout the other three families. In addition, functions impacting cellular apoptosis, chromatin organization, and transcrip- tional activities, to name a few, are possessed by NSs across the families. Peribunyaviridae, Nairoviridae, and Phenuiviridae also encode an NSm, although less extensively studied than NSs, that has roles in antagonizing immune responses, promoting viral assembly and infectivity, and even maintenance of infection in host mosquito vectors. Overall, the similar and divergent roles of NS proteins of these Citation: Leventhal, S.S.; Wilson, D.; human pathogenic Bunyavirales are of particular interest in understanding disease progression, viral Feldmann, H.; Hawman, D.W. -

Yellow Head Virus: Transmission and Genome Analyses
The University of Southern Mississippi The Aquila Digital Community Dissertations Fall 12-2008 Yellow Head Virus: Transmission and Genome Analyses Hongwei Ma University of Southern Mississippi Follow this and additional works at: https://aquila.usm.edu/dissertations Part of the Aquaculture and Fisheries Commons, Biology Commons, and the Marine Biology Commons Recommended Citation Ma, Hongwei, "Yellow Head Virus: Transmission and Genome Analyses" (2008). Dissertations. 1149. https://aquila.usm.edu/dissertations/1149 This Dissertation is brought to you for free and open access by The Aquila Digital Community. It has been accepted for inclusion in Dissertations by an authorized administrator of The Aquila Digital Community. For more information, please contact [email protected]. The University of Southern Mississippi YELLOW HEAD VIRUS: TRANSMISSION AND GENOME ANALYSES by Hongwei Ma Abstract of a Dissertation Submitted to the Graduate Studies Office of The University of Southern Mississippi in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy December 2008 COPYRIGHT BY HONGWEI MA 2008 The University of Southern Mississippi YELLOW HEAD VIRUS: TRANSMISSION AND GENOME ANALYSES by Hongwei Ma A Dissertation Submitted to the Graduate Studies Office of The University of Southern Mississippi in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy Approved: December 2008 ABSTRACT YELLOW HEAD VIRUS: TRANSMISSION AND GENOME ANALYSES by I Iongwei Ma December 2008 Yellow head virus (YHV) is an important pathogen to shrimp aquaculture. Among 13 species of naturally YHV-negative crustaceans in the Mississippi coastal area, the daggerblade grass shrimp, Palaemonetes pugio, and the blue crab, Callinectes sapidus, were tested for potential reservoir and carrier hosts of YHV using PCR and real time PCR. -

Taxonomy of the Order Bunyavirales: Second Update 2018
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Arch Virol Manuscript Author . Author manuscript; Manuscript Author available in PMC 2020 March 01. Published in final edited form as: Arch Virol. 2019 March ; 164(3): 927–941. doi:10.1007/s00705-018-04127-3. TAXONOMY OF THE ORDER BUNYAVIRALES: SECOND UPDATE 2018 A full list of authors and affiliations appears at the end of the article. Abstract In October 2018, the order Bunyavirales was amended by inclusion of the family Arenaviridae, abolishment of three families, creation of three new families, 19 new genera, and 14 new species, and renaming of three genera and 22 species. This article presents the updated taxonomy of the order Bunyavirales as now accepted by the International Committee on Taxonomy of Viruses (ICTV). Keywords Arenaviridae; arenavirid; arenavirus; bunyavirad; Bunyavirales; bunyavirid; Bunyaviridae; bunyavirus; emaravirus; Feraviridae; feravirid, feravirus; fimovirid; Fimoviridae; fimovirus; goukovirus; hantavirid; Hantaviridae; hantavirus; hartmanivirus; herbevirus; ICTV; International Committee on Taxonomy of Viruses; jonvirid; Jonviridae; jonvirus; mammarenavirus; nairovirid; Nairoviridae; nairovirus; orthobunyavirus; orthoferavirus; orthohantavirus; orthojonvirus; orthonairovirus; orthophasmavirus; orthotospovirus; peribunyavirid; Peribunyaviridae; peribunyavirus; phasmavirid; phasivirus; Phasmaviridae; phasmavirus; phenuivirid; Phenuiviridae; phenuivirus; phlebovirus; reptarenavirus; tenuivirus; tospovirid; Tospoviridae; tospovirus; virus classification; virus nomenclature; virus taxonomy INTRODUCTION The virus order Bunyavirales was established in 2017 to accommodate related viruses with segmented, linear, single-stranded, negative-sense or ambisense RNA genomes classified into 9 families [2]. Here we present the changes that were proposed via an official ICTV taxonomic proposal (TaxoProp 2017.012M.A.v1.Bunyavirales_rev) at http:// www.ictvonline.org/ in 2017 and were accepted by the ICTV Executive Committee (EC) in [email protected]. -
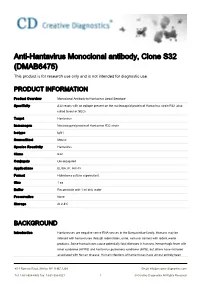
Anti-Hantavirus Monoclonal Antibody, Clone S32 (DMAB6475) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-Hantavirus Monoclonal antibody, Clone S32 (DMAB6475) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Monoclonal Antibody to Hantavirus Seoul Serotype Specificity S32 reacts with an epitope present on the nucleocapsid protein of Hantavirus strain R22 (also called Seoul or SEO) Target Hantavirus Immunogen Nucleocapsid protein of Hantavirus R22 strain Isotype IgG1 Source/Host Mouse Species Reactivity Hantavirus Clone S32 Conjugate Unconjugated Applications ELISA, IF, IHC-Fr Format Hybridoma culture supernatant Size 1 ea Buffer Reconstitute with 1 ml dist. water Preservative None Storage At 2-8℃ BACKGROUND Introduction Hantaviruses are negative sense RNA viruses in the Bunyaviridae family. Humans may be infected with hantaviruses through rodent bites, urine, saliva or contact with rodent waste products. Some hantaviruses cause potentially fatal diseases in humans, hemorrhagic fever with renal syndrome (HFRS) and hantavirus pulmonary syndrome (HPS), but others have not been associated with human disease. Human infections of hantaviruses have almost entirely been 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved linked to human contact with rodent excrement, but recent human-to-human transmission has been reported with the Andes virus in South America. The name hantavirus is derived from the Hantan River area in South Korea, which provided the founding member of the group: Hantaan virus (HTNV), isolated in the late 1970s by Ho-Wang Lee and colleagues. HTNV is one of several hantaviruses that cause HFRS, formerly known as Korean hemorrhagic fever. -

Arenaviridae Astroviridae Filoviridae Flaviviridae Hantaviridae
Hantaviridae 0.7 Filoviridae 0.6 Picornaviridae 0.3 Wenling red spikefish hantavirus Rhinovirus C Ahab virus * Possum enterovirus * Aronnax virus * * Wenling minipizza batfish hantavirus Wenling filefish filovirus Norway rat hunnivirus * Wenling yellow goosefish hantavirus Starbuck virus * * Porcine teschovirus European mole nova virus Human Marburg marburgvirus Mosavirus Asturias virus * * * Tortoise picornavirus Egyptian fruit bat Marburg marburgvirus Banded bullfrog picornavirus * Spanish mole uluguru virus Human Sudan ebolavirus * Black spectacled toad picornavirus * Kilimanjaro virus * * * Crab-eating macaque reston ebolavirus Equine rhinitis A virus Imjin virus * Foot and mouth disease virus Dode virus * Angolan free-tailed bat bombali ebolavirus * * Human cosavirus E Seoul orthohantavirus Little free-tailed bat bombali ebolavirus * African bat icavirus A Tigray hantavirus Human Zaire ebolavirus * Saffold virus * Human choclo virus *Little collared fruit bat ebolavirus Peleg virus * Eastern red scorpionfish picornavirus * Reed vole hantavirus Human bundibugyo ebolavirus * * Isla vista hantavirus * Seal picornavirus Human Tai forest ebolavirus Chicken orivirus Paramyxoviridae 0.4 * Duck picornavirus Hepadnaviridae 0.4 Bildad virus Ned virus Tiger rockfish hepatitis B virus Western African lungfish picornavirus * Pacific spadenose shark paramyxovirus * European eel hepatitis B virus Bluegill picornavirus Nemo virus * Carp picornavirus * African cichlid hepatitis B virus Triplecross lizardfish paramyxovirus * * Fathead minnow picornavirus -

Commission Directive (Eu)
L 279/54 EN Offi cial Jour nal of the European Union 31.10.2019 COMMISSION DIRECTIVE (EU) 2019/1833 of 24 October 2019 amending Annexes I, III, V and VI to Directive 2000/54/EC of the European Parliament and of the Council as regards purely technical adjustments THE EUROPEAN COMMISSION, Having regard to the Treaty on the Functioning of the European Union, Having regard to Directive 2000/54/EC of the European Parliament and of the Council of 18 September 2000 on the protection of workers from risks related to exposure to biological agents at work (1), and in particular Article 19 thereof, Whereas: (1) Principle 10 of the European Pillar of Social Rights (2), proclaimed at Gothenburg on 17 November 2017, provides that every worker has the right to a healthy, safe and well-adapted working environment. The workers’ right to a high level of protection of their health and safety at work and to a working environment that is adapted to their professional needs and that enables them to prolong their participation in the labour market includes protection from exposure to biological agents at work. (2) The implementation of the directives related to the health and safety of workers at work, including Directive 2000/54/EC, was the subject of an ex-post evaluation, referred to as a REFIT evaluation. The evaluation looked at the directives’ relevance, at research and at new scientific knowledge in the various fields concerned. The REFIT evaluation, referred to in the Commission Staff Working Document (3), concludes, among other things, that the classified list of biological agents in Annex III to Directive 2000/54/EC needs to be amended in light of scientific and technical progress and that consistency with other relevant directives should be enhanced. -

SPECIAL REPORT Our Hantaan Virus Became A
SPECIAL REPORT J Bacteriol Virol. Vol 49. No 2. June 2019; 49(2): 45-52 https://doi.org/10.4167/jbv.2019.49.2.45 JBV eISSN 2093-0249 Our Hantaan Virus Became a New Family, Hantaviridae in the Classification of Order Bunyavirales. It will Remain as a History of Virology Ho Wang Lee1,2* and Jin Won Song2 1The National Academy of Sciences, Republic of Korea 2Department of Microbiology, College of Medicine, Korea University, Seoul, Korea In February 2019, the order Bunyavirales, previously family Bunyaviridae, was Corresponding amended by new order of 10 families including Hantaviridae family, and now Ho Wang Lee, M.D., Ph.D. accepted by the International Committee on Taxonomy of Viruses (ICTV). Department of Microbiology, College of Hantaviridae is now a family of the order Bunyavirales, and the prototype virus Medicine, Korea University, Inchon-ro 73, species is Hantaan orthohantavirus. The family Hantaviridae is divided into four Seongbuk-gu, Seoul 02841, Korea subfamilies including Mammantavirinae, Repantavirinae, Actantavirinae and Phone : +82-2-2286-1336 Agantavirinae. The subfamily Mammantavirinae is divided into four genera Fax : +82-2-923-3645 including Orthohantavirus, Loanvirus, Mobatvirus and Thottimvirus. The four Hantavirus species have been found in Korea including three Orthohantaviruses (Hantaan orthohantavirus, Seoul orthohantavirus and Jeju orthohantavirus) and one Thottimvirus (Imjin thottimvirus). Received : May 30, 2019 Revised : June 14, 2019 Key Words: order Bunyavirales, family Hantaviridae, genus Orthohantavirus, genus Accepted : June 17, 2019 Thottimvirus, Hantaan orthohantanvirus, Seoul orthohantanvirus and Jeju orthohantanvirus, Imjin thottimvirus 한탄강의 기적: 한탄바이러스와 서울바이러스 발견 호랑이는 죽어서 가죽을 남기고 사람은 죽어서 이름을 남긴다(虎虎虎虎 人虎虎人)라는 말을 나는 어려서부터 많이 들으면서 자라났다.