Chromosomal Instability and Copy Number Alterations in Barrett's
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Learning from Cadherin Structures and Sequences: Affinity Determinants and Protein Architecture
Learning from cadherin structures and sequences: affinity determinants and protein architecture Klára Fels ıvályi Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Graduate School of Arts and Sciences COLUMBIA UNIVERSITY 2014 © 2014 Klara Felsovalyi All rights reserved ABSTRACT Learning from cadherin structures and sequences: affinity determinants and protein architecture Klara Felsovalyi Cadherins are a family of cell-surface proteins mediating adhesion that are important in development and maintenance of tissues. The family is defined by the repeating cadherin domain (EC) in their extracellular region, but they are diverse in terms of protein size, architecture and cellular function. The best-understood subfamily is the type I classical cadherins, which are found in vertebrates and have five EC domains. Among the five different type I classical cadherins, the binding interactions are highly specific in their homo- and heterophilic binding affinities, though their sequences are very similar. As previously shown, E- and N-cadherins, two prototypic members of the subfamily, differ in their homophilic K D by about an order of magnitude, while their heterophilic affinity is intermediate. To examine the source of the binding affinity differences among type I cadherins, we used crystal structures, analytical ultracentrifugation (AUC), surface plasmon resonance (SPR), and electron paramagnetic resonance (EPR) studies. Phylogenetic analysis and binding affinity behavior show that the type I cadherins can be further divided into two subgroups, with E- and N-cadherin representing each. In addition to the affinity differences in their wild-type binding through the strand-swapped interface, a second interface also shows an affinity difference between E- and N-cadherin. -

Aneuploidy: Using Genetic Instability to Preserve a Haploid Genome?
Health Science Campus FINAL APPROVAL OF DISSERTATION Doctor of Philosophy in Biomedical Science (Cancer Biology) Aneuploidy: Using genetic instability to preserve a haploid genome? Submitted by: Ramona Ramdath In partial fulfillment of the requirements for the degree of Doctor of Philosophy in Biomedical Science Examination Committee Signature/Date Major Advisor: David Allison, M.D., Ph.D. Academic James Trempe, Ph.D. Advisory Committee: David Giovanucci, Ph.D. Randall Ruch, Ph.D. Ronald Mellgren, Ph.D. Senior Associate Dean College of Graduate Studies Michael S. Bisesi, Ph.D. Date of Defense: April 10, 2009 Aneuploidy: Using genetic instability to preserve a haploid genome? Ramona Ramdath University of Toledo, Health Science Campus 2009 Dedication I dedicate this dissertation to my grandfather who died of lung cancer two years ago, but who always instilled in us the value and importance of education. And to my mom and sister, both of whom have been pillars of support and stimulating conversations. To my sister, Rehanna, especially- I hope this inspires you to achieve all that you want to in life, academically and otherwise. ii Acknowledgements As we go through these academic journeys, there are so many along the way that make an impact not only on our work, but on our lives as well, and I would like to say a heartfelt thank you to all of those people: My Committee members- Dr. James Trempe, Dr. David Giovanucchi, Dr. Ronald Mellgren and Dr. Randall Ruch for their guidance, suggestions, support and confidence in me. My major advisor- Dr. David Allison, for his constructive criticism and positive reinforcement. -

Genome-Wide Transcriptional Sequencing Identifies Novel Mutations in Metabolic Genes in Human Hepatocellular Carcinoma DAOUD M
CANCER GENOMICS & PROTEOMICS 11 : 1-12 (2014) Genome-wide Transcriptional Sequencing Identifies Novel Mutations in Metabolic Genes in Human Hepatocellular Carcinoma DAOUD M. MEERZAMAN 1,2 , CHUNHUA YAN 1, QING-RONG CHEN 1, MICHAEL N. EDMONSON 1, CARL F. SCHAEFER 1, ROBERT J. CLIFFORD 2, BARBARA K. DUNN 3, LI DONG 2, RICHARD P. FINNEY 1, CONSTANCE M. CULTRARO 2, YING HU1, ZHIHUI YANG 2, CU V. NGUYEN 1, JENNY M. KELLEY 2, SHUANG CAI 2, HONGEN ZHANG 2, JINGHUI ZHANG 1,4 , REBECCA WILSON 2, LAUREN MESSMER 2, YOUNG-HWA CHUNG 5, JEONG A. KIM 5, NEUNG HWA PARK 6, MYUNG-SOO LYU 6, IL HAN SONG 7, GEORGE KOMATSOULIS 1 and KENNETH H. BUETOW 1,2 1Center for Bioinformatics and Information Technology, National Cancer Institute, Rockville, MD, U.S.A.; 2Laboratory of Population Genetics, National Cancer Institute, National Cancer Institute, Bethesda, MD, U.S.A.; 3Basic Prevention Science Research Group, Division of Cancer Prevention, National Cancer Institute, Bethesda, MD, U.S.A; 4Department of Biotechnology/Computational Biology, St. Jude Children’s Research Hospital, Memphis, TN, U.S.A.; 5Department of Internal Medicine, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea; 6Department of Internal Medicine, University of Ulsan College of Medicine, Ulsan University Hospital, Ulsan, Korea; 7Department of Internal Medicine, College of Medicine, Dankook University, Cheon-An, Korea Abstract . We report on next-generation transcriptome Worldwide, liver cancer is the fifth most common cancer and sequencing results of three human hepatocellular carcinoma the third most common cause of cancer-related mortality (1). tumor/tumor-adjacent pairs. -

Chromosomal Instability and Copy Number Alterations in Barrett's Esophagus and Esophageal Adenocarcinoma Thomas G
Human Cancer Biology Chromosomal Instability and Copy Number Alterations in Barrett's Esophagus and Esophageal Adenocarcinoma Thomas G. Paulson,1,2 Carlo C. Maley,4,5 Xiaohong Li,2 Hongzhe Li,6 Carissa A. Sanchez,1,2 Dennis L. Chao,3 Robert D. Odze,7 Thomas L. Vaughan,2,8 Patricia L. Blount,1,2,10 and Brian J. Reid1,2,9,10 Abstract Purpose: Chromosomal instability, as assessed by many techniques, including DNA content aneuploidy, loss of heterozygosity, and comparative genomic hybridization, has consistently been reported to be common in cancer and rare in normal tissues. Recently, a panel of chromosome instability biomarkers, including loss of heterozygos- ity and DNA content, has been reported to identify patients at high and low risk of pro- gression from Barrett's esophagus (BE) to esophageal adenocarcinoma (EA), but required multiple platforms for implementation. Although chromosomal instability in- volving amplifications and deletions of chromosome regions have been observed in nearly all cancers, copy number alterations (CNA) in premalignant tissues have not been well characterized or evaluated in cohort studies as biomarkers of cancer risk. Experimental Design: We examined CNAs in 98 patients having either BE or EA using Bacterial Artificial Chromosome (BAC) array comparative genomic hybridization to char- acterize CNAs at different stages of progression ranging from early BE to advanced EA. Results: CNAs were rare in early stages (less than high-grade dysplasia) but were pro- gressively more frequent and larger in later stages (high-grade dysplasia and EA), in- cluding high-level amplifications. The number of CNAs correlated highly with DNA content aneuploidy. -

WO 2013/095793 Al 27 June 2013 (27.06.2013) W P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2013/095793 Al 27 June 2013 (27.06.2013) W P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C12Q 1/68 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/US2012/063579 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, 5 November 20 12 (05 .11.20 12) KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, (25) Filing Language: English NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, (26) Publication Language: English RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, (30) Priority Data: ZM, ZW. 61/579,530 22 December 201 1 (22. 12.201 1) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: AVEO PHARMACEUTICALS, INC. kind of regional protection available): ARIPO (BW, GH, [US/US]; 75 Sidney Street, Fourth Floor, Cambridge, MA GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, 02139 (US). -

Notate Human RPE-Specific Gene Expression
UvA-DARE (Digital Academic Repository) Function and pathology of the human retinal pigment epithelium Booij, J.C. Publication date 2010 Link to publication Citation for published version (APA): Booij, J. C. (2010). Function and pathology of the human retinal pigment epithelium. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:25 Sep 2021 A new strategy to identify and an- notate human RPE-specific gene expression 3 Judith C Booij, Jacoline B ten Brink, Sigrid MA Swagemakers, Annemieke JMH Verkerk, Anke HW Essing, Peter J van der Spek, Arthur AB Bergen. PlosOne 2010, 5(3) e9341 Chapter 3 Abstract Background: The aim of the study was to identify and functionally annotate cell type-spe- cific gene expression in the human retinal pigment epithelium (RPE), a key tissue involved in age-related macular degeneration and retinitis pigmentosa. -

Protocadherin in Colorectal Tumours
Hindawi Publishing Corporation Gastroenterology Research and Practice Volume 2015, Article ID 317093, 9 pages http://dx.doi.org/10.1155/2015/317093 Research Article Epigenetic-Mediated Downregulation of -Protocadherin in Colorectal Tumours Bujko Mateusz,1 Kober Paulina,1 Statkiewicz MaBgorzata,2 Mikula Michal,2 Ligaj Marcin,3 Zwierzchowski Lech,4 Ostrowski Jerzy,2 and Siedlecki Janusz Aleksander1 1 Department of Molecular and Translational Oncology, Maria Sklodowska-Curie Memorial Cancer Center and Institute of Oncology, 5W.K.Roentgena,02-781Warsaw,Poland 2Department of Genetics, Maria Sklodowska-Curie Memorial Cancer Center and Institute of Oncology, 5W.K.Roentgena,02-781Warsaw,Poland 3Department of Pathology, Maria Sklodowska-Curie Memorial Cancer Center and Institute of Oncology, 5 W.K. Roentgena, 02-781 Warsaw, Poland 4Department of Molecular Biology, Institute of Genetics and Animal Breeding, 36A Postępu 36A, Jastrzębiec, 05-552 Magdalenka, Poland Correspondence should be addressed to Bujko Mateusz; [email protected] Received 16 November 2014; Accepted 25 March 2015 Academic Editor: Robert Odze Copyright © 2015 Bujko Mateusz et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Carcinogenesis involves altered cellular interaction and tissue morphology that partly arise from aberrant expression of cadherins. Mucin-like protocadherin is implicated in intercellular adhesion and its expression was found decreased in colorectal cancer (CRC). This study has compared MUPCDH (CDHR5) expression in three key types of colorectal tissue samples, for normal mucosa, adenoma, and carcinoma. A gradual decrease of mRNA levels and protein expression was observed in progressive stages of colorectal carcinogenesis which are consistent with reports of increasing MUPCDH 5 promoter region DNA methylation. -

Chromosomal Instability and Copy Number Alterations in Barrett's Esophagus and Esophageal Adenocarcinoma Thomas G
Human Cancer Biology Chromosomal Instability and Copy Number Alterations in Barrett's Esophagus and Esophageal Adenocarcinoma Thomas G. Paulson,1,2 Carlo C. Maley,4,5 Xiaohong Li,2 Hongzhe Li,6 Carissa A. Sanchez,1,2 Dennis L. Chao,3 Robert D. Odze,7 Thomas L. Vaughan,2,8 Patricia L. Blount,1,2,10 and Brian J. Reid1,2,9,10 Abstract Purpose: Chromosomal instability, as assessed by many techniques, including DNA content aneuploidy, loss of heterozygosity, and comparative genomic hybridization, has consistently been reported to be common in cancer and rare in normal tissues. Recently, a panel of chromosome instability biomarkers, including loss of heterozygos- ity and DNA content, has been reported to identify patients at high and low risk of pro- gression from Barrett's esophagus (BE) to esophageal adenocarcinoma (EA), but required multiple platforms for implementation. Although chromosomal instability in- volving amplifications and deletions of chromosome regions have been observed in nearly all cancers, copy number alterations (CNA) in premalignant tissues have not been well characterized or evaluated in cohort studies as biomarkers of cancer risk. Experimental Design: We examined CNAs in 98 patients having either BE or EA using Bacterial Artificial Chromosome (BAC) array comparative genomic hybridization to char- acterize CNAs at different stages of progression ranging from early BE to advanced EA. Results: CNAs were rare in early stages (less than high-grade dysplasia) but were pro- gressively more frequent and larger in later stages (high-grade dysplasia and EA), in- cluding high-level amplifications. The number of CNAs correlated highly with DNA content aneuploidy. -
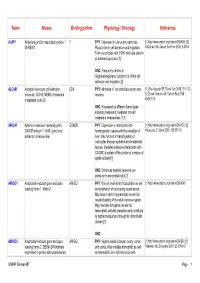
Name Aliases Binding Partner Physiology / Oncology References
Name Aliases Binding partner Physiology / Oncology References AJAP1 Adherens junction associated protein 1, ? PHY : Expressed in uterus and pancreas. [1] http://www.uniprot.org/uniprot/Q9UKB5. [2] SHREW1 Plays a role in cell adhesion and migration. McDonald JM, Cancer Biol Ther 2006, 5:300-4 Forms a complex with CDH1 and beta-catenin at adherens junctions [1] ONC : Frequently deleted in oligodendrogliomas, functions to inhibit cell adhesion and migration [2] ALCAM Activated leukocyte cell adhesion CD6 PHY : Adhesion of activated leukocytes and [1] Ofori-Acquah SF, Transl Res 2008, 151:122- molecule, CD166, MEMD (melanoma neurons 8. [2] van Kilsdonk JW, Cancer Res 2008, metastasis clone D) 68:3671-9 ONC : Expressed by different tumor types including melanoma; mediates cancer/ melanoma invasiveness [1,2] AMICA1 Adhesion molecule interacting with CXADR PHY : Expression is restricted to the [1] http://www.uniprot.org/uniprot/Q86YT9. [2] CXADR antigen 1, JAML (junctional hematopoietic tissues with the exception of Moog-Lutz C, Blood 2003, 102:3371-8 adhesion molecule-like) liver. May function in transmigration of leukocytes through epithelial and endothelial tissues. Mediates adhesive interactions with CXADR, a protein of the junctional complex of epithelial cells [1] ONC : Enhances myeloid leukemia cell adhesion to endothelial cells [2] AMIGO1 Amphoterin-induced gene and open AMIGO PHY : May be involved in fasciculation as well [1] http://www.uniprot.org/uniprot/Q86WK6 reading frame 1, Alivin-2 as myelination of developing neural axons. May have a role in regeneration as well as neural plasticity in the adult nervous system. May mediate homophilic as well as heterophilic cell-cell interaction and contribute to signal transduction through its intracellular domain [1] ONC : - AMIGO2 Amphoterin-induced gene and open AMIGO PHY : Highest levels in breast, ovary, cervix, [1] http://www.uniprot.org/uniprot/Q86SJ2. -
Supplementary Information
Supplementary Information Table S1. Regions of CNV data excluded from CNV analysis due to poor density of probe coverage. Region Centromere Telomere Chr. p q p q 1 p11.1, p11.2, q11, q12, q21.1 p36.33, p36.32, p36.31, q44 p12, p13.1 p36.23, p36.22, p36.21 2 p11.1, p11.2 q11.1 p25.3 q37.3 3 p11.1 q11.1, q11.2 none excluded q29 4 p11 q11 p16.1, p16.2, p16.3 q35.2, q35.1 5 p12 q11.1 p15.33 q35.3, q35.2, q35.1 6 p11.1 q11.1 p25.3, p35.2 q27 7 p11.1 q11.1, q11.21 p22.3 q36.3 8 p11.1 q11.1 p23.3, p23.2, p23.1 q24.3 9 p11.1, p11.2 q11, q12, q13 p24.3 q34.3, q34.2, q34.13, q34.12, q34.11 10 p11.1 q11.1, q11.21, q11.22 none excluded q26.3 11 p11.11, p11.12 q11 p15.5 q25 12 p11.1, p11.21 q11 p13.33, p13.32 q24.33, q24.32, q24.31 13 no probes q11 no probes q34 14 no probes q11.1, q11.2 no probes q32.33 15 no probes q11.1, q11.2, q12, no probes q26.3 q13.1, q13.2, q13.3 16 p11.1, p11.2 q11.1, q11.2 p13.3 q24.3, q24.2, q24.1 17 none excluded none excluded p13.3 q25.3 18 p11.1, p11.21 q11.1 none excluded q23 19 p11 q11 p13.3 q13.43 20 p11.1, p11.21 q11.1, q11.21 none excluded q13.33 21 no probes q11.1, q11.2 no probes q22.3 22 no probes q11.1, q11.21, q11.22 no probes q13.33, q13.32 Table S2. -

A New Strategy to Identify and Annotate Human RPE-Specific Gene Expression
A New Strategy to Identify and Annotate Human RPE-Specific Gene Expression Judith C. Booij1, Jacoline B. ten Brink1, Sigrid M. A. Swagemakers2,3, Annemieke J. M. H. Verkerk2, Anke H. W. Essing1, Peter J. van der Spek2, Arthur A. B. Bergen1,4,5* 1 Department of Clinical and Molecular Ophthalmogenetics, Netherlands Institute for Neuroscience, Royal Netherlands Academy of Arts and Sciences, Amsterdam, The Netherlands, 2 Department of Bioinformatics and Genetics, Erasmus Medical Center, Rotterdam, The Netherlands, 3 Cancer Genomics Centre, Erasmus Medical Center, Rotterdam, The Netherlands, 4 Clinical Genetics Academic Medical Centre Amsterdam, University of Amsterdam, The Netherlands, 5 Department of Ophthalmology, Academic Medical Centre Amsterdam, University of Amsterdam, The Netherlands Abstract Background: To identify and functionally annotate cell type-specific gene expression in the human retinal pigment epithelium (RPE), a key tissue involved in age-related macular degeneration and retinitis pigmentosa. Methodology: RPE, photoreceptor and choroidal cells were isolated from selected freshly frozen healthy human donor eyes using laser microdissection. RNA isolation, amplification and hybridization to 44 k microarrays was carried out according to Agilent specifications. Bioinformatics was carried out using Rosetta Resolver, David and Ingenuity software. Principal Findings: Our previous 22 k analysis of the RPE transcriptome showed that the RPE has high levels of protein synthesis, strong energy demands, is exposed to high levels of oxidative stress and a variable degree of inflammation. We currently use a complementary new strategy aimed at the identification and functional annotation of RPE-specific expressed transcripts. This strategy takes advantage of the multilayered cellular structure of the retina and overcomes a number of limitations of previous studies. -

Mouse Cdhr5 Knockout Project (CRISPR/Cas9)
https://www.alphaknockout.com Mouse Cdhr5 Knockout Project (CRISPR/Cas9) Objective: To create a Cdhr5 knockout Mouse model (C57BL/6J) by CRISPR/Cas-mediated genome engineering. Strategy summary: The Cdhr5 gene (NCBI Reference Sequence: NM_001114322 ; Ensembl: ENSMUSG00000025497 ) is located on Mouse chromosome 7. 15 exons are identified, with the ATG start codon in exon 1 and the TAG stop codon in exon 15 (Transcript: ENSMUST00000167263). Exon 1~15 will be selected as target site. Cas9 and gRNA will be co-injected into fertilized eggs for KO Mouse production. The pups will be genotyped by PCR followed by sequencing analysis. Note: Exon 1 starts from about 0.04% of the coding region. Exon 1~15 covers 100.0% of the coding region. The size of effective KO region: ~7564 bp. The KO region does not have any other known gene. Page 1 of 9 https://www.alphaknockout.com Overview of the Targeting Strategy Wildtype allele 5' gRNA region gRNA region 3' 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Legends Exon of mouse Cdhr5 Knockout region Page 2 of 9 https://www.alphaknockout.com Overview of the Dot Plot (up) Window size: 15 bp Forward Reverse Complement Sequence 12 Note: The 2000 bp section upstream of start codon is aligned with itself to determine if there are tandem repeats. Tandem repeats are found in the dot plot matrix. The gRNA site is selected outside of these tandem repeats. Overview of the Dot Plot (down) Window size: 15 bp Forward Reverse Complement Sequence 12 Note: The 2000 bp section downstream of stop codon is aligned with itself to determine if there are tandem repeats.