Chromosomal Instability and Copy Number Alterations in Barrett's Esophagus and Esophageal Adenocarcinoma Thomas G
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tyrosine Kinase Oncogenes in Normal Hematopoiesis and Hematological Disease
Oncogene (2002) 21, 3314 ± 3333 ã 2002 Nature Publishing Group All rights reserved 0950 ± 9232/02 $25.00 www.nature.com/onc Tyrosine kinase oncogenes in normal hematopoiesis and hematological disease Blanca Scheijen1,2 and James D Grin*,1,2 1Department of Adult Oncology, Dana-Farber Cancer Institute, 44 Binney Street, Boston, Massachusetts, MA 02115, USA; 2Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Boston, Massachusetts, USA Tyrosine kinase oncogenes are formed as a result of Adaptors do not contain intrinsic catalytic activity but mutations that induce constitutive kinase activity. Many consist of independent functioning interaction modules of these tyrosine kinase oncogenes that are derived from like SH2-domain (mediates binding to phosphotyrosine genes, such as c-Abl, c-Fes, Flt3, c-Fms, c-Kit and residues), SH3-domain (interacts with polyproline-rich PDGFRb, that are normally involved in the regulation of PXXP stretch) or pleckstrin homology (PH) domain hematopoiesis or hematopoietic cell function. Despite (binds to inositol lipids). dierences in structure, normal function, and subcellular The ®rst tyrosine kinase oncogene associated with location, many of the tyrosine kinase oncogenes signal human hematologic disease, Bcr ± Abl, was identi®ed through the same pathways, and typically enhance almost twenty years ago, and there is now evidence for proliferation and prolong viability. They represent involvement of multiple tyrosine kinase oncogenes in excellent potential drug targets, and it is likely that acute and chronic leukemias, lymphomas, and myelo- additional mutations will be identi®ed in other kinases, mas. In each case, the tyrosine kinase activity of the their immediate downstream targets, or in proteins oncogene is constitutively activated by mutations that regulating their function. -

Anti-GRAP Antibody (ARG63124)
Product datasheet [email protected] ARG63124 Package: 100 μg anti-GRAP antibody Store at: -20°C Summary Product Description Goat Polyclonal antibody recognizes GRAP Tested Reactivity Hu Predict Reactivity Ms, Rat, Cow Tested Application WB Host Goat Clonality Polyclonal Isotype IgG Target Name GRAP Antigen Species Human Immunogen C-GFFPRSYVQPVHL Conjugation Un-conjugated Alternate Names GRB2-related adapter protein Application Instructions Application table Application Dilution WB 0.3 - 1 µg/ml Application Note WB: Recommend incubate at RT for 1h. * The dilutions indicate recommended starting dilutions and the optimal dilutions or concentrations should be determined by the scientist. Calculated Mw 25 kDa Properties Form Liquid Purification Purified from goat serum by ammonium sulphate precipitation followed by antigen affinity chromatography using the immunizing peptide. Buffer Tris saline (pH 7.3), 0.02% Sodium azide and 0.5% BSA Preservative 0.02% Sodium azide Stabilizer 0.5% BSA Concentration 0.5 mg/ml Storage instruction For continuous use, store undiluted antibody at 2-8°C for up to a week. For long-term storage, aliquot and store at -20°C or below. Storage in frost free freezers is not recommended. Avoid repeated freeze/thaw cycles. Suggest spin the vial prior to opening. The antibody solution should be gently mixed before use. www.arigobio.com 1/2 Note For laboratory research only, not for drug, diagnostic or other use. Bioinformation Database links GeneID: 10750 Human Swiss-port # Q13588 Human Background This gene encodes a member of the GRB2/Sem5/Drk family and functions as a cytoplasmic signaling protein which contains an SH2 domain flanked by two SH3 domains. -

Biological Databases What Is a Database ?
BIOLOGICAL DATABASES WHAT IS A DATABASE ? A structured collection of data held in computer storage; esp. one that incorporates software to make it accessible in a variety of ways; any large collection of information. A collection of data structured searchable (index) -> table of contents updated periodically (release) -> new edition cross-referenced (hyperlinks ) -> links with other db Includes also associated tools (software) necessary for access, updating, information insertion, information deletion…. A database consists of basic units called records or entries. Each record consists of fields, which hold pre-defined data related to the record. For example, a protein database would have protein sequences as records and protein properties as fields (e.g., name of protein, length, amino-acid sequence, …) 2 DATABASES ON THE INTERNET Biological databases often have web interfaces, which allow users to send queries to the databases. Some databases can be accessed by different web servers, each offering a different interface. request query web page result User Web server Database server 3 WHY BIOLOGICAL DATABASES ? Exponential growth in biological data. Data (genomic sequences, 3D structures, 2D gel analysis, MS analysis, Microarrays….) are no longer published in a conventional manner, but directly submitted to databases. Essential tools for biological research. The only way to publish massive amounts of data without using all the paper in the world. 4 NUCLEOTIDES 5 COMPLETE GENOMES Until 2018: Eukaryotes 5262 Prokaryotes 131446 Viruses 14027 6 SOME STATISTICS More than 1000 different ‘biological’ databases Variable size: <100Kb to >20Gb DNA: > 20 Gb Protein: 1 Gb 3D structure: 5 Gb Other: smaller Update frequency: daily to annually to seldom to forget about it . -

Learning from Cadherin Structures and Sequences: Affinity Determinants and Protein Architecture
Learning from cadherin structures and sequences: affinity determinants and protein architecture Klára Fels ıvályi Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Graduate School of Arts and Sciences COLUMBIA UNIVERSITY 2014 © 2014 Klara Felsovalyi All rights reserved ABSTRACT Learning from cadherin structures and sequences: affinity determinants and protein architecture Klara Felsovalyi Cadherins are a family of cell-surface proteins mediating adhesion that are important in development and maintenance of tissues. The family is defined by the repeating cadherin domain (EC) in their extracellular region, but they are diverse in terms of protein size, architecture and cellular function. The best-understood subfamily is the type I classical cadherins, which are found in vertebrates and have five EC domains. Among the five different type I classical cadherins, the binding interactions are highly specific in their homo- and heterophilic binding affinities, though their sequences are very similar. As previously shown, E- and N-cadherins, two prototypic members of the subfamily, differ in their homophilic K D by about an order of magnitude, while their heterophilic affinity is intermediate. To examine the source of the binding affinity differences among type I cadherins, we used crystal structures, analytical ultracentrifugation (AUC), surface plasmon resonance (SPR), and electron paramagnetic resonance (EPR) studies. Phylogenetic analysis and binding affinity behavior show that the type I cadherins can be further divided into two subgroups, with E- and N-cadherin representing each. In addition to the affinity differences in their wild-type binding through the strand-swapped interface, a second interface also shows an affinity difference between E- and N-cadherin. -

Aneuploidy: Using Genetic Instability to Preserve a Haploid Genome?
Health Science Campus FINAL APPROVAL OF DISSERTATION Doctor of Philosophy in Biomedical Science (Cancer Biology) Aneuploidy: Using genetic instability to preserve a haploid genome? Submitted by: Ramona Ramdath In partial fulfillment of the requirements for the degree of Doctor of Philosophy in Biomedical Science Examination Committee Signature/Date Major Advisor: David Allison, M.D., Ph.D. Academic James Trempe, Ph.D. Advisory Committee: David Giovanucci, Ph.D. Randall Ruch, Ph.D. Ronald Mellgren, Ph.D. Senior Associate Dean College of Graduate Studies Michael S. Bisesi, Ph.D. Date of Defense: April 10, 2009 Aneuploidy: Using genetic instability to preserve a haploid genome? Ramona Ramdath University of Toledo, Health Science Campus 2009 Dedication I dedicate this dissertation to my grandfather who died of lung cancer two years ago, but who always instilled in us the value and importance of education. And to my mom and sister, both of whom have been pillars of support and stimulating conversations. To my sister, Rehanna, especially- I hope this inspires you to achieve all that you want to in life, academically and otherwise. ii Acknowledgements As we go through these academic journeys, there are so many along the way that make an impact not only on our work, but on our lives as well, and I would like to say a heartfelt thank you to all of those people: My Committee members- Dr. James Trempe, Dr. David Giovanucchi, Dr. Ronald Mellgren and Dr. Randall Ruch for their guidance, suggestions, support and confidence in me. My major advisor- Dr. David Allison, for his constructive criticism and positive reinforcement. -

Genome-Wide Transcriptional Sequencing Identifies Novel Mutations in Metabolic Genes in Human Hepatocellular Carcinoma DAOUD M
CANCER GENOMICS & PROTEOMICS 11 : 1-12 (2014) Genome-wide Transcriptional Sequencing Identifies Novel Mutations in Metabolic Genes in Human Hepatocellular Carcinoma DAOUD M. MEERZAMAN 1,2 , CHUNHUA YAN 1, QING-RONG CHEN 1, MICHAEL N. EDMONSON 1, CARL F. SCHAEFER 1, ROBERT J. CLIFFORD 2, BARBARA K. DUNN 3, LI DONG 2, RICHARD P. FINNEY 1, CONSTANCE M. CULTRARO 2, YING HU1, ZHIHUI YANG 2, CU V. NGUYEN 1, JENNY M. KELLEY 2, SHUANG CAI 2, HONGEN ZHANG 2, JINGHUI ZHANG 1,4 , REBECCA WILSON 2, LAUREN MESSMER 2, YOUNG-HWA CHUNG 5, JEONG A. KIM 5, NEUNG HWA PARK 6, MYUNG-SOO LYU 6, IL HAN SONG 7, GEORGE KOMATSOULIS 1 and KENNETH H. BUETOW 1,2 1Center for Bioinformatics and Information Technology, National Cancer Institute, Rockville, MD, U.S.A.; 2Laboratory of Population Genetics, National Cancer Institute, National Cancer Institute, Bethesda, MD, U.S.A.; 3Basic Prevention Science Research Group, Division of Cancer Prevention, National Cancer Institute, Bethesda, MD, U.S.A; 4Department of Biotechnology/Computational Biology, St. Jude Children’s Research Hospital, Memphis, TN, U.S.A.; 5Department of Internal Medicine, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea; 6Department of Internal Medicine, University of Ulsan College of Medicine, Ulsan University Hospital, Ulsan, Korea; 7Department of Internal Medicine, College of Medicine, Dankook University, Cheon-An, Korea Abstract . We report on next-generation transcriptome Worldwide, liver cancer is the fifth most common cancer and sequencing results of three human hepatocellular carcinoma the third most common cause of cancer-related mortality (1). tumor/tumor-adjacent pairs. -

NLRP3 and ASC Differentially Affect the Lung Transcriptome During Pneumococcal Pneumonia
UvA-DARE (Digital Academic Repository) Cell-specific pattern recognition receptor signaling in antibacterial defense van Lieshout, M.H.P. Publication date 2015 Document Version Final published version Link to publication Citation for published version (APA): van Lieshout, M. H. P. (2015). Cell-specific pattern recognition receptor signaling in antibacterial defense. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:30 Sep 2021 Chapter 7 NLRP3 and ASC differentially affect the lung transcriptome during pneumococcal pneumonia American Journal of Respiratory Cell and Molecular Biology 2014 Apr;50(4):699-712 DOI: 10.1165/rcmb.2013-0015OC Miriam H.P. van Lieshout 1,2 Brendon P. Scicluna 1,2 Sandrine Florquin 3 Tom van der Poll 1,2,4 Academic Medical Center, University of Amsterdam, Amsterdam, the Netherlands: 1Center of Infection and Immunity Amsterdam 2Center of Experimental and Molecular Medicine 3Department of Pathology 4Division of Infectious Diseases Chapter 7 Abstract Streptococcus (S.) pneumoniae is the most frequently isolated causative pathogen of community-acquired pneumonia, a leading cause of mortality worldwide. -

GRAP (NM 006613) Human Tagged ORF Clone Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for RG208908 GRAP (NM_006613) Human Tagged ORF Clone Product data: Product Type: Expression Plasmids Product Name: GRAP (NM_006613) Human Tagged ORF Clone Tag: TurboGFP Symbol: GRAP Synonyms: DFNB114 Vector: pCMV6-AC-GFP (PS100010) E. coli Selection: Ampicillin (100 ug/mL) Cell Selection: Neomycin ORF Nucleotide >RG208908 representing NM_006613 Sequence: Red=Cloning site Blue=ORF Green=Tags(s) TTTTGTAATACGACTCACTATAGGGCGGCCGGGAATTCGTCGACTGGATCCGGTACCGAGGAGATCTGCC GCCGCGATCGCC ATGGAGTCCGTGGCCCTGTACAGCTTTCAGGCTACAGAGAGCGACGAGCTGGCCTTCAACAAGGGAGACA CACTCAAGATCCTGAACATGGAGGATGACCAGAACTGGTACAAGGCCGAGCTCCGGGGTGTCGAGGGATT TATTCCCAAGAACTACATCCGCGTCAAGCCCCATCCGTGGTACTCGGGCAGGATTTCCCGGCAGCTGGCC GAAGAGATTCTGATGAAGCGGAACCATCTGGGAGCCTTCCTGATCCGGGAGAGTGAGAGCTCCCCAGGGG AGTTCTCTGTGTCTGTGAACTATGGAGACCAGGTGCAGCACTTCAAGGTGCTGCGTGAGGCCTCGGGGAA GTACTTCCTGTGGGAGGAGAAGTTCAACTCCCTCAACGAGCTGGTCGACTTCTACCGCACCACCACCATC GCCAAGAAGCGGCAGATCTTCCTGCGCGACGAGGAGCCCTTGCTCAAGTCACCTGGGGCCTGCTTTGCCC AGGCCCAGTTTGACTTCTCAGCCCAGGACCCCTCGCAGCTCAGCTTCCGCCGTGGCGACATCATTGAGGT CCTGGAGCGCCCAGACCCCCACTGGTGGCGGGGCCGGTCCTGCGGGCGCGTTGGCTTCTTCCCACGGAGT TACGTGCAGCCCGTGCACCTG ACGCGTACGCGGCCGCTCGAG - GFP Tag - GTTTAA Protein Sequence: >RG208908 representing NM_006613 Red=Cloning site Green=Tags(s) MESVALYSFQATESDELAFNKGDTLKILNMEDDQNWYKAELRGVEGFIPKNYIRVKPHPWYSGRISRQLA EEILMKRNHLGAFLIRESESSPGEFSVSVNYGDQVQHFKVLREASGKYFLWEEKFNSLNELVDFYRTTTI -
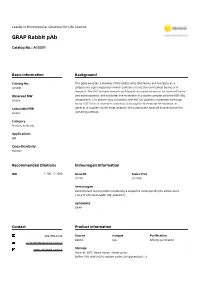
GRAP Rabbit Pab
Leader in Biomolecular Solutions for Life Science GRAP Rabbit pAb Catalog No.: A15391 Basic Information Background Catalog No. This gene encodes a member of the GRB2/Sem5/Drk family and functions as a A15391 cytoplasmic signaling protein which contains an SH2 domain flanked by two SH3 domains. The SH2 domain interacts with ligand-activated receptors for stem cell factor Observed MW and erythropoietin, and facilitates the formation of a stable complex with the BCR-ABL 36kDa oncoprotein. This protein also associates with the Ras guanine nucleotide exchange factor SOS1 (son of sevenless homolog 1) through its N-terminal SH3 domain. In Calculated MW general, it couples signals from receptor and cytoplasmic tyrosine kinases to the Ras 25kDa signaling pathway. Category Primary antibody Applications WB Cross-Reactivity Human Recommended Dilutions Immunogen Information WB 1:200 - 1:2000 Gene ID Swiss Prot 10750 Q13588 Immunogen Recombinant fusion protein containing a sequence corresponding to amino acids 128-217 of human GRAP (NP_006604.1). Synonyms GRAP Contact Product Information 400-999-6126 Source Isotype Purification Rabbit IgG Affinity purification [email protected] www.abclonal.com.cn Storage Store at -20℃. Avoid freeze / thaw cycles. Buffer: PBS with 0.02% sodium azide,50% glycerol,pH7.3. Validation Data Western blot analysis of extracts of various cell lines, using GRAP antibody (A15391) at 1:1000 dilution. Secondary antibody: HRP Goat Anti-Rabbit IgG (H+L) (AS014) at 1:10000 dilution. Lysates/proteins: 25ug per lane. Blocking buffer: 3% nonfat dry milk in TBST. Detection: ECL Basic Kit (RM00020). Exposure time: 5s. Antibody | Protein | ELISA Kits | Enzyme | NGS | Service For research use only. -

Regulation of Ras Exchange Factors and Cellular Localization of Ras Activation by Lipid Messengers Int Cells
REVIEW ARTICLE published: 04 September 2013 doi: 10.3389/fimmu.2013.00239 Regulation of Ras exchange factors and cellular localization of Ras activation by lipid messengers inT cells Jesse E. Jun1, Ignacio Rubio2 and Jeroen P.Roose 1* 1 Department of Anatomy, University of California San Francisco, San Francisco, CA, USA 2 Institute for Molecular Cell Biology, Center for Sepsis Control and Care (CSCC), University Hospital, Friedrich-Schiller-University, Jena, Germany Edited by: The Ras-MAPK signaling pathway is highly conserved throughout evolution and is acti- Karsten Sauer, The Scripps Research vated downstream of a wide range of receptor stimuli. Ras guanine nucleotide exchange Institute, USA factors (RasGEFs) catalyze GTP loading of Ras and play a pivotal role in regulating receptor- Reviewed by: Kjetil Taskén, University of Oslo, ligand induced Ras activity. In T cells, three families of functionally important RasGEFs are Norway expressed: RasGRF,RasGRP,and Son of Sevenless (SOS)-family GEFs. Early on it was rec- Balbino Alarcon, Consejo Superior de ognized that Ras activation is critical for T cell development and that the RasGEFs play an Investigaciones Cientificas, Spain important role herein. More recent work has revealed that nuances in Ras activation appear *Correspondence: to significantly impactT cell development and selection.These nuances include distinct bio- Jeroen P.Roose, Department of Anatomy, University of California San chemical patterns of analog versus digital Ras activation, differences in cellular localization Francisco, 513 Parnassus Avenue, of Ras activation, and intricate interplays between the RasGEFs during distinctT cell devel- Room HSW-1326, San Francisco, CA opmental stages as revealed by various new mouse models. -

And Y-Linked Ampliconic Genes in Human Populations
HIGHLIGHTED ARTICLE | INVESTIGATION Dynamic Copy Number Evolution of X- and Y-Linked Ampliconic Genes in Human Populations Elise A. Lucotte,1 Laurits Skov, Jacob Malte Jensen, Moisès Coll Macià, Kasper Munch, and Mikkel H. Schierup Bioinformatic Research Center, Aarhus University, 8000, Denmark ORCID ID: 0000-0001-8442-2654 (E.A.L.) ABSTRACT Ampliconic genes are multicopy, with the majority found on sex chromosomes and enriched for testis-expressed genes. While ampliconic genes have been associated with the emergence of hybrid incompatibilities, we know little about their copy number distribution and their turnover in human populations. Here, we explore the evolution of human X- and Y-linked ampliconic genes by investigating copy number variation (CNV) and coding variation between populations using the Simons Genome Diversity Project. We develop a method to assess CNVs using the read depth on modified X and Y chromosome targets containing only one repetition of each ampliconic gene. Our results reveal extensive standing variation in copy number both within and between human populations for several ampliconic genes. For the Y chromosome, we can infer multiple independent amplifications and losses of these gene copies even within closely related Y haplogroups, that diversified , 50,000 years ago. Moreover, X- and Y-linked ampliconic genes seem to have a faster amplification dynamic than autosomal multicopy genes. Looking at expression data from another study, we also find that X- and Y-linked ampliconic genes with extensive CNV are significantly more expressed than genes with no CNV during meiotic sex chromosome inactivation (for both X and Y) and postmeiotic sex chromosome repression (for the Y chromosome only). -

Gads Is a Novel SH2 and SH3 Domain-Containing Adaptor Protein That Binds to Tyrosine-Phosphorylated Shc
Oncogene (1998) 17, 3073 ± 3082 ã 1998 Stockton Press All rights reserved 0950 ± 9232/98 $12.00 http://www.stockton-press.co.uk/onc Gads is a novel SH2 and SH3 domain-containing adaptor protein that binds to tyrosine-phosphorylated Shc Stanley K Liu and C Jane McGlade Department of Medical Biophysics, Ontario Cancer Institute, AMGEN Institute, University of Toronto, 620 University Avenue, Suite 706, Toronto, Ontario, Canada, M5G 2C1 Shc proteins are important substrates of receptor and human tumor cells with known tyrosine kinase gene cytoplasmic tyrosine kinases that couple activated alterations (Pelicci et al., 1995). Following tyrosine- receptors to downstream signaling enzymes. Phosphor- phosphorylation, Shc associates with the SH2 and ylation of Shc tyrosine residues 239 and 317 leads to SH3 domain-containing adaptor protein, Grb2 (Low- recruitment of the Grb2-Sos complex, thus linking Shc enstein et al., 1992; Rozakis-Adcock et al., 1992). This phosphorylation to Ras activation. We have used interaction is mediated by the phosphorylated tyrosine phosphorylated peptides corresponding to the regions residues 239 and 317 of Shc which are both found spanning tyrosine 239/240 and 317 of Shc in an within a sequence conforming to a high anity expression library screen to identify additional down- binding site for the Grb2 SH2 domain (Salcini et stream targets of Shc. Here we report the identi®cation al., 1994; van der Geer et al., 1996; Gotoh et al., of Gads, a novel adaptor protein most similar to Grb2 1996; Harmer and DeFranco, 1997). The Grb2 SH3 and Grap that contains amino and carboxy terminal domains mediate its stable association with the Ras SH3 domains ¯anking a central SH2 domain and a 120 guanine nucleotide exchange factor, Sos, and mem- amino acid unique region.