Dihydroergotamine, Ergotamine, Methysergide and Sumatriptan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Medication Guide
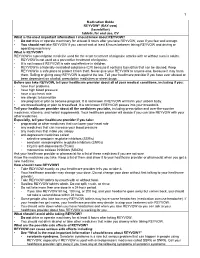
1 Medication Guide REYVOW® (RAY-vow) (lasmiditan) tablets, for oral use, CV What is the most important information I should know about REYVOW? • Do not drive or operate machinery for at least 8 hours after you take REYVOW, even if you feel well enough. • You should not take REYVOW if you cannot wait at least 8 hours between taking REYVOW and driving or operating machinery. What is REYVOW? REYVOW is a prescription medicine used for the acute treatment of migraine attacks with or without aura in adults. • REYVOW is not used as a preventive treatment of migraine. • It is not known if REYVOW is safe and effective in children. • REYVOW is a federally controlled substance (CV) because it contains lasmiditan that can be abused. Keep REYVOW in a safe place to protect it from theft. Never give your REYVOW to anyone else, because it may harm them. Selling or giving away REYVOW is against the law. Tell your healthcare provider if you have ever abused or been dependent on alcohol, prescription medicines or street drugs. Before you take REYVOW, tell your healthcare provider about all of your medical conditions, including if you: • have liver problems • have high blood pressure • have a low heart rate • are allergic to lasmiditan • are pregnant or plan to become pregnant. It is not known if REYVOW will harm your unborn baby. • are breastfeeding or plan to breastfeed. It is not known if REYVOW passes into your breastmilk. Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. -

Anti-Migraine Agents Reference Number: OH.PHAR.PPA.34 Effective Date: 01.01.21 Last Review Date: 11.20 Line of Business: Medicaid
Clinical Policy: Anti-Migraine Agents Reference Number: OH.PHAR.PPA.34 Effective Date: 01.01.21 Last Review Date: 11.20 Line of Business: Medicaid See Important Reminder at the end of this policy for important regulatory and legal information. Description • When using a preferred agent where applicable, the number of tablets/doses allowed per month will be restricted based on the manufacturer’s package insert and/or Buckeye Health plans quantity limits. CNS AGENTS: ANTI-MIGRAINE AGENTS – ACUTE MIGRANE TREATMENT NO PA REQUIRED “PREFERRED” STEP THERAPY REQUIRED PA REQUIRED “NON-PREFERRED” “PREFERRED” NARATRIPTAN (GENERIC OF AMERGE®) NURTEC™ ODT (rimegepant) ALMOTRIPTAN (generic of Axert®) RIZATRIPTAN TABLETS (GENERIC OF CAFERGOT® (ergotamine w/caffeine) MAXALT®) ELETRIPTAN (generic of Relpax®) RIZATRIPTAN ODT (GENERIC OF ERGOMAR® (ergotamine) MAXALT-MLT®) FROVA® (frovatriptan) SUMATRIPTAN TABLETS, NASAL SPRAY, MIGERGOT® (ergotamine w/caffeine) INJECTION (GENERIC OF MIGRANAL® (dihydroergotamine) IMITREX®) ONZETRA™ XSAIL™ (sumatriptan) REYVOW™ (lasmiditan) SUMAVEL DOSEPRO® (sumatriptan) TOSYMRA® (sumatriptan) TREXIMET® (sumatriptan/naproxen) UBRELVY™ (ubrogepant)* ZOLMITRIPTAN (generic of Zomig®) ZOLMITRIPTAN ODT (generic of Zomig ZMT®) ZOMIG® NASAL SPRAY (zolmitriptan) CNS AGENTS: ANTI-MIGRAINE AGENTS – CLUSTER HEADACHE TREATMENT NO PA REQUIRED “PREFERRED” PA REQUIRED “NON-PREFERRED” VERAPAMIL (Generic of Calan®) EMGALITY™ (galcanezumab) VERAPAMIL SR/ER (Generic of Calan SR®, Isoptin SR®, Verelan®) CNS AGENTS: ANTI-MIGRAINE AGENTS – PROPHYLAXIS TREATMENT NO PA REQUIRED “PREFERRED” STEP THERAPY REQUIRED PA REQUIRED “NON-PREFERRED” (Trials of at least 3 controller “PREFERRED” medications) Cardiovascular Agents: Beta-blockers AIMOVIG™ (erenumab-aooe) † EMGALITY™ (galcanezumab) CNS Agents: Anticonvulsants AJOVY™ (fremanezumab-vfrm) * CNS Agents: Serotonin-norepinephrine reuptake inhibitors CNS Agents: Tricyclic antidepressants †Initial Dose is limited to 70mg once monthly; may request dose increase if 70mg fails to provide adequate relief over two consecutive months. -

What Are the Acute Treatments for Migraine and How Are They Used?
2. Acute Treatment CQ II-2-1 What are the acute treatments for migraine and how are they used? Recommendation The mainstay of acute treatment for migraine is pharmacotherapy. The drugs used include (1) acetaminophen, (2) non-steroidal anti-inflammatory drugs (NSAIDs), (3) ergotamines, (4) triptans and (5) antiemetics. Stratified treatment according to the severity of migraine is recommended: use NSAIDs such as aspirin and naproxen for mild to moderate headache, and use triptans for moderate to severe headache, or even mild to moderate headache when NSAIDs were ineffective in the past. It is necessary to give guidance and cautions to patients having acute attacks, and explain the methods of using medications (timing, dose, frequency of use) and medication use during pregnancy and breast-feeding. Grade A Background and Objective The objective of acute treatment is to resolve the migraine attack completely and rapidly and restore the patient’s normal functions. An ideal treatment should have the following characteristics: (1) resolves pain and associated symptoms rapidly; (2) is consistently effective; (3) no recurrence; (4) no need for additional use of medication; (5) no adverse effects; (6) can be administered by the patients themselves; and (7) low cost. Literature was searched to identify acute treatments that satisfy the above conditions. Comments and Evidence The acute treatment drugs for migraine generally include (1) acetaminophens, (2) non-steroidal anti-inflammatory drugs (NSAIDs), (3) ergotamines, (4) triptans, and (5) antiemetics. For severe migraines including status migrainosus and migraine attacks refractory to treatment, (6) anesthetics, and (7) corticosteroids (dexamethasone) are used (Tables 1 and 2).1)-9) There are two approaches to the selection and sequencing of these medications: “step care” and “stratified care”. -

Pharmacokinetics, Pharmacodynamics and Drug
pharmaceutics Review Pharmacokinetics, Pharmacodynamics and Drug–Drug Interactions of New Anti-Migraine Drugs—Lasmiditan, Gepants, and Calcitonin-Gene-Related Peptide (CGRP) Receptor Monoclonal Antibodies Danuta Szkutnik-Fiedler Department of Clinical Pharmacy and Biopharmacy, Pozna´nUniversity of Medical Sciences, Sw.´ Marii Magdaleny 14 St., 61-861 Pozna´n,Poland; [email protected] Received: 28 October 2020; Accepted: 30 November 2020; Published: 3 December 2020 Abstract: In the last few years, there have been significant advances in migraine management and prevention. Lasmiditan, ubrogepant, rimegepant and monoclonal antibodies (erenumab, fremanezumab, galcanezumab, and eptinezumab) are new drugs that were launched on the US pharmaceutical market; some of them also in Europe. This publication reviews the available worldwide references on the safety of these anti-migraine drugs with a focus on the possible drug–drug (DDI) or drug–food interactions. As is known, bioavailability of a drug and, hence, its pharmacological efficacy depend on its pharmacokinetics and pharmacodynamics, which may be altered by drug interactions. This paper discusses the interactions of gepants and lasmiditan with, i.a., serotonergic drugs, CYP3A4 inhibitors, and inducers or breast cancer resistant protein (BCRP) and P-glycoprotein (P-gp) inhibitors. In the case of monoclonal antibodies, the issue of pharmacodynamic interactions related to the modulation of the immune system functions was addressed. It also focuses on the effect of monoclonal antibodies on expression of class Fc gamma receptors (FcγR). Keywords: migraine; lasmiditan; gepants; monoclonal antibodies; drug–drug interactions 1. Introduction Migraine is a chronic neurological disorder characterized by a repetitive, usually unilateral, pulsating headache with attacks typically lasting from 4 to 72 h. -

The Serotonergic System in Migraine Andrea Rigamonti Domenico D’Amico Licia Grazzi Susanna Usai Gennaro Bussone
J Headache Pain (2001) 2:S43–S46 © Springer-Verlag 2001 MIGRAINE AND PATHOPHYSIOLOGY Massimo Leone The serotonergic system in migraine Andrea Rigamonti Domenico D’Amico Licia Grazzi Susanna Usai Gennaro Bussone Abstract Serotonin (5-HT) and induce migraine attacks. Moreover serotonin receptors play an impor- different pharmacological preventive tant role in migraine pathophysiolo- therapies (pizotifen, cyproheptadine gy. Changes in platelet 5-HT content and methysergide) are antagonist of are not casually related, but they the same receptor class. On the other may reflect similar changes at a neu- side the activation of 5-HT1B-1D ronal level. Seven different classes receptors (triptans and ergotamines) of serotoninergic receptors are induce a vasocostriction, a block of known, nevertheless only 5-HT2B-2C neurogenic inflammation and pain M. Leone • A. Rigamonti • D. D’Amico and 5HT1B-1D are related to migraine transmission. L. Grazzi • S. Usai • G. Bussone (౧) syndrome. Pharmacological evi- C. Besta National Neurological Institute, Via Celoria 11, I-20133 Milan, Italy dences suggest that migraine is due Key words Serotonin • Migraine • e-mail: [email protected] to an hypersensitivity of 5-HT2B-2C Triptans • m-Chlorophenylpiperazine • Tel.: +39-02-2394264 receptors. m-Chlorophenylpiperazine Pathogenesis Fax: +39-02-70638067 (mCPP), a 5-HT2B-2C agonist, may The 5-HT receptor family is distinguished from all other 5- Introduction 1 HT receptors by the absence of introns in the genes; in addi- tion all are inhibitors of adenylate cyclase [1]. Serotonin (5-HT) and serotonin receptors play an important The 5-HT1A receptor has a high selective affinity for 8- role in migraine pathophysiology. -

Novel Formulations for Treatment of Migraine
(19) TZZ _T (11) EP 2 756 756 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 23.07.2014 Bulletin 2014/30 A01N 43/42 (2006.01) A61K 31/44 (2006.01) (21) Application number: 14165112.5 (22) Date of filing: 24.04.2009 (84) Designated Contracting States: • Turanin, John AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Emeryville, CA California 94608 (US) HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL • Hawley, Roger PT RO SE SI SK TR Emeryville, CA California 94608 (US) • Schuster, Jeffrey, A. (30) Priority: 28.04.2008 US 48463 Bolinas, CA California 94924 (US) (62) Document number(s) of the earlier application(s) in (74) Representative: Duxbury, Stephen et al accordance with Art. 76 EPC: Arnold & Siedsma 09739139.5 / 2 273 880 Pettenkoferstrasse 37 80336 München (DE) (71) Applicant: Zogenix, Inc. Emeryville CA 94608 (US) Remarks: This application was filed on 17-04-2014 as a (72) Inventors: divisional application to the application mentioned • Farr, Stephen J. under INID code 62. Orinda, CA California 94563 (US) (54) Novel formulations for treatment of migraine (57) Systems and methods are described for treating Systems that are self contained, portable, prefilled, and un-met medical needs in migraine and related conditions simple to self administer at the onset of a migraine attack such as cluster headache. Included are treatments that are disclosed, and preferably include a needle-free in- are both rapid onset and long acting, which include sus- jector and a high viscosity formulation, to eliminate such tained release formulations, and combination products, issues as fear of self administration with needles, and Also included are treatments for multiple symptoms of needle stick and cross contamination. -

Current and Prospective Pharmacological Targets in Relation to Antimigraine Action
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Erasmus University Digital Repository Naunyn-Schmiedeberg’s Arch Pharmacol (2008) 378:371–394 DOI 10.1007/s00210-008-0322-7 REVIEW Current and prospective pharmacological targets in relation to antimigraine action Suneet Mehrotra & Saurabh Gupta & Kayi Y. Chan & Carlos M. Villalón & David Centurión & Pramod R. Saxena & Antoinette MaassenVanDenBrink Received: 8 January 2008 /Accepted: 6 June 2008 /Published online: 15 July 2008 # The Author(s) 2008 Abstract Migraine is a recurrent incapacitating neuro- (CGRP1 and CGRP2), adenosine (A1,A2,andA3), glutamate vascular disorder characterized by unilateral and throbbing (NMDA, AMPA, kainate, and metabotropic), dopamine, headaches associated with photophobia, phonophobia, endothelin, and female hormone (estrogen and progesterone) nausea, and vomiting. Current specific drugs used in the receptors. In addition, we have considered some other acute treatment of migraine interact with vascular receptors, targets, including gamma-aminobutyric acid, angiotensin, a fact that has raised concerns about their cardiovascular bradykinin, histamine, and ionotropic receptors, in relation to safety. In the past, α-adrenoceptor agonists (ergotamine, antimigraine therapy. Finally, the cardiovascular safety of dihydroergotamine, isometheptene) were used. The last two current and prospective antimigraine therapies is touched decades have witnessed the advent of 5-HT1B/1D receptor upon. agonists (sumatriptan and second-generation triptans), which have a well-established efficacy in the acute Keywords 5-HT. Antimigraine drugs . CGRP. treatment of migraine. Moreover, current prophylactic Noradrenaline . Migraine . Receptors treatments of migraine include 5-HT2 receptor antagonists, Ca2+ channel blockers, and β-adrenoceptor antagonists. Despite the progress in migraine research and in view of its Introduction complex etiology, this disease still remains underdiagnosed, and available therapies are underused. -

Triptans Step Therapy/Quantity Limit Criteria
Triptans Step Therapy/Quantity Limit Criteria Program may be implemented with the following options 1) step therapy 2) quantity limits or 3) step therapy with quantity limits For Blue Cross and Blue Shield of Illinois Option 1 (step therapy only) will apply. Brand Generic Dosage Form Amerge® naratriptan tablets Axert® almotriptan tablets Frova® frovatriptan tablets Imitrex® sumatriptan injection*, nasal spray, tablets* Maxalt® rizatriptan tablets Maxalt-MLT® rizatriptan tablets Relpax® eletriptan tablets Treximet™ sumatriptan and naproxen tablets Zomig® zolmitriptan tablets, nasal spray Zomig-ZMT® zolmitriptan tablets * generic available and included as target agent in quantity limit edit FDA APPROVED INDICATIONS1-7 The following information is taken from individual drug prescribing information and is provided here as background information only. Not all FDA-approved indications may be considered medically necessary. All criteria are found in the section “Prior Authorization Criteria for Approval.” Amerge® Tablets1, Axert® Tablets2, Frova® Tablets3,Imitrex® injection4, Imitrex Nasal Spray5, Imitrex Tablets6, Maxalt® Tablets7, Maxalt-MLT® Tablets7, Relpax® Tablets8, Treximet™ Tablets9, Zomig® Tablets10, Zomig-ZMT® Tablets10, and Zomig® Nasal Spray11 Amerge (naratriptan), Axert (almotriptan), Frova (frovatriptan), Imitrex (sumatriptan), Maxalt (rizatriptan), Maxalt-MLT (rizatriptan orally disintegrating), Relpax (eletriptan), Treximet (sumatriptan/naproxen), Zomig (zolmitriptan), and Zomig-ZMT (zolmitriptan orally disintegrating) tablets, and Imitrex (sumatriptan) and Zomig (zolmitriptan) nasal spray are all indicated for the acute treatment of migraine attacks with or without aura in adults. They are not intended for the prophylactic therapy of migraine or for use in the management of hemiplegic or basilar migraine. Safety and effectiveness of all of these products have not been established for cluster headache, which is present in an older, predominantly male population. -

(DMT), Harmine, Harmaline and Tetrahydroharmine: Clinical and Forensic Impact
pharmaceuticals Review Toxicokinetics and Toxicodynamics of Ayahuasca Alkaloids N,N-Dimethyltryptamine (DMT), Harmine, Harmaline and Tetrahydroharmine: Clinical and Forensic Impact Andreia Machado Brito-da-Costa 1 , Diana Dias-da-Silva 1,2,* , Nelson G. M. Gomes 1,3 , Ricardo Jorge Dinis-Oliveira 1,2,4,* and Áurea Madureira-Carvalho 1,3 1 Department of Sciences, IINFACTS-Institute of Research and Advanced Training in Health Sciences and Technologies, University Institute of Health Sciences (IUCS), CESPU, CRL, 4585-116 Gandra, Portugal; [email protected] (A.M.B.-d.-C.); ngomes@ff.up.pt (N.G.M.G.); [email protected] (Á.M.-C.) 2 UCIBIO-REQUIMTE, Laboratory of Toxicology, Department of Biological Sciences, Faculty of Pharmacy, University of Porto, 4050-313 Porto, Portugal 3 LAQV-REQUIMTE, Laboratory of Pharmacognosy, Department of Chemistry, Faculty of Pharmacy, University of Porto, 4050-313 Porto, Portugal 4 Department of Public Health and Forensic Sciences, and Medical Education, Faculty of Medicine, University of Porto, 4200-319 Porto, Portugal * Correspondence: [email protected] (D.D.-d.-S.); [email protected] (R.J.D.-O.); Tel.: +351-224-157-216 (R.J.D.-O.) Received: 21 September 2020; Accepted: 20 October 2020; Published: 23 October 2020 Abstract: Ayahuasca is a hallucinogenic botanical beverage originally used by indigenous Amazonian tribes in religious ceremonies and therapeutic practices. While ethnobotanical surveys still indicate its spiritual and medicinal uses, consumption of ayahuasca has been progressively related with a recreational purpose, particularly in Western societies. The ayahuasca aqueous concoction is typically prepared from the leaves of the N,N-dimethyltryptamine (DMT)-containing Psychotria viridis, and the stem and bark of Banisteriopsis caapi, the plant source of harmala alkaloids. -

Diapositiva 1
Characterization of the 5-HT7 receptor as a new therapeutic target for the treatment of pain Àlex Brenchat Barberà ADVERTIMENT. La consulta d’aquesta tesi queda condicionada a l’acceptació de les següents condicions d'ús: La difusió d’aquesta tesi per mitjà del servei TDX (www.tdx.cat) ha estat autoritzada pels titulars dels drets de propietat intel·lectual únicament per a usos privats emmarcats en activitats d’investigació i docència. No s’autoritza la seva reproducció amb finalitats de lucre ni la seva difusió i posada a disposició des d’un lloc aliè al servei TDX. No s’autoritza la presentació del seu contingut en una finestra o marc aliè a TDX (framing). Aquesta reserva de drets afecta tant al resum de presentació de la tesi com als seus continguts. En la utilització o cita de parts de la tesi és obligat indicar el nom de la persona autora. ADVERTENCIA. La consulta de esta tesis queda condicionada a la aceptación de las siguientes condiciones de uso: La difusión de esta tesis por medio del servicio TDR (www.tdx.cat) ha sido autorizada por los titulares de los derechos de propiedad intelectual únicamente para usos privados enmarcados en actividades de investigación y docencia. No se autoriza su reproducción con finalidades de lucro ni su difusión y puesta a disposición desde un sitio ajeno al servicio TDR. No se autoriza la presentación de su contenido en una ventana o marco ajeno a TDR (framing). Esta reserva de derechos afecta tanto al resumen de presentación de la tesis como a sus contenidos. -

(12) United States Patent (10) Patent No.: US 6,264,917 B1 Klaveness Et Al
USOO6264,917B1 (12) United States Patent (10) Patent No.: US 6,264,917 B1 Klaveness et al. (45) Date of Patent: Jul. 24, 2001 (54) TARGETED ULTRASOUND CONTRAST 5,733,572 3/1998 Unger et al.. AGENTS 5,780,010 7/1998 Lanza et al. 5,846,517 12/1998 Unger .................................. 424/9.52 (75) Inventors: Jo Klaveness; Pál Rongved; Dagfinn 5,849,727 12/1998 Porter et al. ......................... 514/156 Lovhaug, all of Oslo (NO) 5,910,300 6/1999 Tournier et al. .................... 424/9.34 FOREIGN PATENT DOCUMENTS (73) Assignee: Nycomed Imaging AS, Oslo (NO) 2 145 SOS 4/1994 (CA). (*) Notice: Subject to any disclaimer, the term of this 19 626 530 1/1998 (DE). patent is extended or adjusted under 35 O 727 225 8/1996 (EP). U.S.C. 154(b) by 0 days. WO91/15244 10/1991 (WO). WO 93/20802 10/1993 (WO). WO 94/07539 4/1994 (WO). (21) Appl. No.: 08/958,993 WO 94/28873 12/1994 (WO). WO 94/28874 12/1994 (WO). (22) Filed: Oct. 28, 1997 WO95/03356 2/1995 (WO). WO95/03357 2/1995 (WO). Related U.S. Application Data WO95/07072 3/1995 (WO). (60) Provisional application No. 60/049.264, filed on Jun. 7, WO95/15118 6/1995 (WO). 1997, provisional application No. 60/049,265, filed on Jun. WO 96/39149 12/1996 (WO). 7, 1997, and provisional application No. 60/049.268, filed WO 96/40277 12/1996 (WO). on Jun. 7, 1997. WO 96/40285 12/1996 (WO). (30) Foreign Application Priority Data WO 96/41647 12/1996 (WO). -

Biased Ligands Differentially Shape the Conformation of The
International Journal of Molecular Sciences Article Biased Ligands Differentially Shape the Conformation of the Extracellular Loop Region in 5-HT2B Receptors Katrin Denzinger, Trung Ngoc Nguyen, Theresa Noonan, Gerhard Wolber and Marcel Bermudez * Institute of Pharmacy, Freie Universität Berlin, Königin-Luise-Strasse 2-4, 14195 Berlin, Germany; [email protected] (K.D.); [email protected] (T.N.N.); [email protected] (T.N.); [email protected] (G.W.) * Correspondence: [email protected] Received: 22 November 2020; Accepted: 18 December 2020; Published: 20 December 2020 Abstract: G protein-coupled receptors are linked to various intracellular transducers, each pathway associated with different physiological effects. Biased ligands, capable of activating one pathway over another, are gaining attention for their therapeutic potential, as they could selectively activate beneficial pathways whilst avoiding those responsible for adverse effects. We performed molecular dynamics simulations with known β-arrestin-biased ligands like lysergic acid diethylamide and ergotamine in complex with the 5-HT2B receptor and discovered that the extent of ligand bias is directly connected with the degree of closure of the extracellular loop region. Given a loose allosteric coupling of extracellular and intracellular receptor regions, we delineate a concept for biased signaling at serotonin receptors, by which conformational interference with binding pocket closure restricts the signaling repertoire of the receptor. Molecular docking studies of biased ligands gathered from the BiasDB demonstrate that larger ligands only show plausible docking poses in the ergotamine-bound structure, highlighting the conformational constraints associated with bias. This emphasizes the importance of selecting the appropriate receptor conformation on which to base virtual screening workflows in structure-based drug design of biased ligands.