The Institute of Chartered Accountants of Nigeria Professional Level Examination – May 2021 Case Study Examination Instruction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

S/No Placement 1
S/NO PLACEMENT ADO - ODO/OTA LOCAL GOVERNMENT SECRETARIAT, SANGO - OTA, OGUN 1 STATE AGEGE LOCAL GOVERNMENT, BALOGUN STREET, MATERNITY, SANGO, 2 AGEGE, LAGOS STATE 3 AHMAD AL-IMAM NIG. LTD., NO 27, ZULU GAMBARI RD., ILORIN 4 AKTEM TECHNOLOGY, ILORIN, KWARA STATE 5 ALLAMIT NIG. LTD., IBADAN, OYO STATE 6 AMOULA VENTURES LTD., IKEJA, LAGOS STATE CALVERTON HELICOPTERS, 2, PRINCE KAYODE, AKINGBADE CLOSE, 7 VICTORIA ISLAND, LAGOS STATE CHI-FARM LTD., KM 20, IBADAN/LAGOS EXPRESSWAY, AJANLA, IBADAN, 8 OYO STATE CHINA CIVIL ENGINEERING CONSTRUCTION CORPORATION (CCECC), KM 3, 9 ABEOKUTA/LAGOS EXPRESSWAY, OLOMO - ORE, OGUN STATE COCOA RESEARCH INSTITUTE OF NIGERIA (CRIN), KM 14, IJEBU ODE ROAD, 10 IDI - AYANRE, IBADAN, OYO STATE COKER AGUDA LOCAL COUNCIL, 19/29, THOMAS ANIMASAUN STREET, 11 AGUDA, SURULERE, LAGOS STATE CYBERSPACE NETWORK LTD.,33 SAKA TIINUBU STREET. VICTORIA ISLAND, 12 LAGOS STATE DE KOOLAR NIGERIA LTD.,PLOT 14, HAKEEM BALOGUN STREET, OPP. 13 TECHNICAL COLLEGE, AGIDINGBI, IKEJA, LAGOS STATE DEPARTMENT OF PETROLEUM RESOURCES, 11, NUPE ROAD, OFF AHMAN 14 PATEGI ROAD, G.R.A, ILORIN, KWARA STATE DOLIGERIA BIOSYSTEMS NIGERIA LTD, 1, AFFAN COMPLEX, 1, OLD JEBBA 15 ROAD, ILORIN, KWARA STATE ESFOOS STEEL CONSTRUCTION COMPANY, OPP. SDP, OLD IFE ROAD, 16 AKINFENWA, EGBEDA, IBADAN, OYO STATE 17 FABIS FARMS NIGERIA LTD., ILORIN, KWARA STATE FEDERAL AIRPORT AUTHORITY, MURTALA MOHAMMED AIRPORT, IKEJA, 18 LAGOS STATE FEDERAL INSTITUTE OF INDUSTRIAL RESEARCH OSHODI (FIIRO), 3, FIIRO 19 ROAD, OFF CAPPA BUS STOP, AGEGE MOTOR ROAD, OSHODI, LAGOS FEDERAL MINISTRY OF AGRICULTURE & RURAL DEVELOPMENT, FOOD & STRATEGIC GRAINS RESERVE DEPARTMENT (FRSD) SILO COMPLEX, KWANA 20 WAYA, YOLA, ADAMAWA STATE 21 FRESH COUNTRY CHICKEN ENTERPRISES, SHONGA, KWARA STATE 22 GOLDEN PENNY FLOUR MILLLS, APAPA WHARF, APAPA, LAGOS STATE HURLAG TECHNOLOGIES, 7, LADIPO OLUWOLE STREET, OFF ADENIYI JONES 23 AVENUE, IKEJA, LAGOS STATE 24 IBN DEND, FARM, KM. -

PROBLEMS and CHALLENGES in MEETING the STANDARDS for EFFECTIVE RADIOTHERAPY DELIVERY in NIGERIA Timothy Akpa
PROBLEMS AND CHALLENGES IN MEETING THE STANDARDS FOR EFFECTIVE RADIOTHERAPY DELIVERY IN NIGERIA Timothy Akpa Nigerian Nuclear Regulatory Authority, Abuja OUTLINE • Introduction • Requirements for starting a Radiotherapy Facility • Safety Problems in Radiation Therapy Practice in Nigeria • Reflections on the Way Forward INTRODUCTION Prediction on Cancer Occurrence • According to the estimates from World Health Organization (WHO), the incidence of new cancer cases detected globally would rise from the existing 10.1 million in year 2000 to around 15.3 million in 2020 • This rise of 51.4% would be mainly attributed to an increase of 72.2% in the new cancer cases detected in the developing countries, (from 5.4 million in 2000 to 9.3 million in 2020). • In developed countries, the rise during the corresponding period is expected to be just around 27.6%. • Coupled with the rise in incidence of cancer in developing countries, the estimated rise in deaths could be to the tune of 75% from 3.6 million to nearly 6.3 million in the next 20 years • To cater for this predicted increase in cancer incidence in developing countries, at least some options are imperative: • to take adequate comprehensive measures directed towards cancer prevention and early diagnosis – Cancer prevention and education is an important facet of the cancer management strategy , which has to be pursued vigorously . • to establish adequate treatment and palliative care structures . (This will also make early diagnosis effective.) – Radiation therapy is an important component of the integrated cancer treatment – nearly 50 to 60% of the patients would be requiring radiation therapy at some point • to have an effective cancer management strategy, facilities for radiation therapy should be available within easy reach of the patients. -

4 Annual Conference of the Society for Quality In
4th ANNUAL CONFERENCE OF THE SOCIETY FOR QUALITY IN HEALTHCARE IN NIGERIA Venue: Colonades Hotel, 21 Alfred Rewane (Formerly Kingway Road) Ikoyi, Lagos, Nigeria Date: July 18th 2013 Time: 8:30 – 6:00 pm Time Activity Coordinator 8:30 – 9:00 am Arrival and Registration of Guests/ Welcome coffee Mrs. Bolanle Senbanjo Welcome Remarks Professor Ade Elebute 9:00 – 9:10 am Welcome Remarks Chairman, SQHN Ms. Njide Ndili 9:10 – 9:15 am Update on the Society Secretary, SQHN Session 1 – Patient Safety Practices in Nigeria Dr. Ugochi Utti Patient Safety as a marketing strategy – Obio Clinic 9:15 – 9:30am Quality Assurance Manager experience Obio Clinic Port Harcourt Patient Safety Culture in 5 SPDC-Supported facilities Assoc. Prof L. U Ogbonnaya, 9:30 – 10:10 am in the Niger Delta Region Community Health Consultant 10:10 – 10:40 am Tea Break Session II – Patient Safety and Accreditation Dr. Simbo Davidson Patient Safety with COHSASA accreditation - Quality Assurance Manager, 10:40 – 11.10am Reddington Hospital Experience Reddington Hospital 11.10 - 12:00 pm Advancing Patient Safety through Accreditation Ms. Triona Fortune Deputy CEO, ISQua 12.00 – 12:20 pm Question and Answer 12.20 -1.20 pm Lunch Break Panel Discussion - Leadership in Healthcare Quality 1:20 – 2:10 pm Developing leadership in Healthcare Quality Moderator: Prof E. Otolorin Panel Discussion: President NMA /President Country Manager JPHEIGO AGPMP/Register, MDCN SQHN Board Member 4th ANNUAL CONFERENCE OF THE SOCIETY FOR QUALITY IN HEALTHCARE IN NIGERIA Venue: Colonades Hotel, 21 Alfred Rewane (Formerly Kingway Road) Ikoyi, Lagos, Nigeria Date: July 18th 2013 Time: 8:30 – 6:00 pm Session III – Advancing Patient Safety with Information Technology Dr. -

Odo/Ota Local Government Secretariat, Sango - Agric
S/NO PLACEMENT DEPARTMENT ADO - ODO/OTA LOCAL GOVERNMENT SECRETARIAT, SANGO - AGRIC. & BIO. ENGINEERING 1 OTA, OGUN STATE AGEGE LOCAL GOVERNMENT, BALOGUN STREET, MATERNITY, AGRIC. & BIO. ENGINEERING 2 SANGO, AGEGE, LAGOS STATE AHMAD AL-IMAM NIG. LTD., NO 27, ZULU GAMBARI RD., ILORIN AGRIC. & BIO. ENGINEERING 3 4 AKTEM TECHNOLOGY, ILORIN, KWARA STATE AGRIC. & BIO. ENGINEERING 5 ALLAMIT NIG. LTD., IBADAN, OYO STATE AGRIC. & BIO. ENGINEERING 6 AMOULA VENTURES LTD., IKEJA, LAGOS STATE AGRIC. & BIO. ENGINEERING CALVERTON HELICOPTERS, 2, PRINCE KAYODE, AKINGBADE MECHANICAL ENGINEERING 7 CLOSE, VICTORIA ISLAND, LAGOS STATE CHI-FARM LTD., KM 20, IBADAN/LAGOS EXPRESSWAY, AJANLA, AGRIC. & BIO. ENGINEERING 8 IBADAN, OYO STATE CHINA CIVIL ENGINEERING CONSTRUCTION CORPORATION (CCECC), KM 3, ABEOKUTA/LAGOS EXPRESSWAY, OLOMO - ORE, AGRIC. & BIO. ENGINEERING 9 OGUN STATE COCOA RESEARCH INSTITUTE OF NIGERIA (CRIN), KM 14, IJEBU AGRIC. & BIO. ENGINEERING 10 ODE ROAD, IDI - AYANRE, IBADAN, OYO STATE COKER AGUDA LOCAL COUNCIL, 19/29, THOMAS ANIMASAUN AGRIC. & BIO. ENGINEERING 11 STREET, AGUDA, SURULERE, LAGOS STATE CYBERSPACE NETWORK LTD.,33 SAKA TIINUBU STREET. AGRIC. & BIO. ENGINEERING 12 VICTORIA ISLAND, LAGOS STATE DE KOOLAR NIGERIA LTD.,PLOT 14, HAKEEM BALOGUN STREET, AGRIC. & BIO. ENGINEERING OPP. TECHNICAL COLLEGE, AGIDINGBI, IKEJA, LAGOS STATE 13 DEPARTMENT OF PETROLEUM RESOURCES, 11, NUPE ROAD, OFF AGRIC. & BIO. ENGINEERING 14 AHMAN PATEGI ROAD, G.R.A, ILORIN, KWARA STATE DOLIGERIA BIOSYSTEMS NIGERIA LTD, 1, AFFAN COMPLEX, 1, AGRIC. & BIO. ENGINEERING 15 OLD JEBBA ROAD, ILORIN, KWARA STATE Page 1 SIWES PLACEMENT COMPANIES & ADDRESSES.xlsx S/NO PLACEMENT DEPARTMENT ESFOOS STEEL CONSTRUCTION COMPANY, OPP. SDP, OLD IFE AGRIC. & BIO. ENGINEERING 16 ROAD, AKINFENWA, EGBEDA, IBADAN, OYO STATE 17 FABIS FARMS NIGERIA LTD., ILORIN, KWARA STATE AGRIC. -
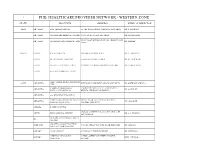
Phb Healthcare Provider Network - Western Zone
1 PHB HEALTHCARE PROVIDER NETWORK - WESTERN ZONE STATE PROVIDER ADDRESS MEDICAL DIRECTOR EKITI ADO-EKITI ADE-TADE HOSPITAL 55, OKE-BOLA STREET, AJILOSUN, ADO-EKITI DR. T. ADEDAPO ADO-EKITI FASANMADE MEDICAL CENTRE 93, IWOROKO ROAD, ADO-EKITI DR. FASANMADE 12, LITTLE BY LITTLE ROAD OFF ADEBAYO,ADO- ADO-EKITI OLUMORIN SPECIALIST HOSPITAL DR. LADELE EKITI KWARA ILORIN BALM HOSPITAL 29B, BISHOP STREET G.R.A. DR. A. ADEDAYO ILORIN OLANREWAJU HOSPITAL 5, ORO-AGO CLOSE, ILORIN DR. OLANREWAJU ILORIN OLAOLU HOSPITAL ILORIN 173 MURTALA MOHAMMED WAY, ILORIN DR OLORUNTOBA ILORIN ANCHOR MEDICAL CENTRE FIRST ALPHA MEDICAL CENTRE OGUN ABEOKUTA KUFUROJI OLUBI DRIVE,ADIGBE ABEOKUTA DR. ADEWALE ADEOLA LTD JOSEPH & CHRISTIANA 5, SURULERE STREET OFF LALUBU STREET ABEOKUTA DR. OGUNGBE SPECIALIST HOSPITAL BEHIND AFRI-BANK OKE-ILEWO ABEOKUTA SACRED HEART HOSPITAL MERCY GROUP CLINICS (MERCY MERCY ROAD, BEHIND UBA BUILDING ABEOKUTA MR. OMOJOYE COMPANY NIG. LTD) PANSEKE ABEOKUTA AGBARA ROPHE HOSPITAL 1 JOLASCO STREET, JOLASCO BUS STOP, OFF AKUTE BLISS MEDICAL CENTRE DR. A.A. WAHAB AKUTE ROAD. DEMARK CLINIC&MATERNITY IFO CENTRE AMAZING GRACE HOSPITAL IJEBU-ODE 7, ILORO STREET,OFF NEW ROAD IJEBU-ODE DR. ADELAJA (KETONIC MEDICAL LTD) SAGAMU ALPHA CLINIC 3, CATHOLIC CHURCH STREET DR. ODUWOLE MEDYTOP SPECIALIST 3, EJIMO ALEBIOSUN STREET,OJUMELE SAGAMU PROF. ODUSOGA HOSPITAL SAGAMU SANGO-OTA ACE MEDICARE CLINIC LTD KM 4, IDI- IROKO ROAD SANGO- OTA DR. KUKOYI 37, AKINWUNMI STREET{JOJO ROAD} G.R.A. SANGO-OTA FARAMED CLINICS DR. FARAYIBI SANGO OTTA ONDO AKURE FUJAH SPECIALIST HOSPITAL 22, AYETUTU STREET OPP. ISIKAN MARKET DR. FUJAH C/31, OWATUMISE STREET,BEHIND STATE AKURE INLAND MEDICAL CENTRE DR. -
(2017) Abstract of Local Government Statistics
LAGOS STATE GOVERNMENT ABSTRACT OF LOCAL GOVERNMENT STATISTICS 2017 LAGOS BUREAU OF STATISTICS MINISTRY OF ECONOMIC PLANNING AND BUDGET, SECRETARIAT, ALAUSA, IKEJA. PREFACE The Abstract of Local Government Statistics is a yearly publication produced by the Lagos Bureau of Statistics (LBS). This edition contains detailed information on Y2016 Socio Economic Statistics of the 57 Local Government and Local Council Development Areas (LG/LCDAs) in Lagos State. The activities of the LG\LCDAS are classified into ten (10) components, these are: demographic distributions and nine (9) Classifications of functions of Government (COFOG). This publication is useful to all and sundry both locally and internationally for researchers, planners, private organizations and Non Governmental Organizations to mention but a few. The State wishes to express its appreciation to the officials of the Local Government and Local Council Development Areas (LG/LCDAs) and all Agencies that contributed to the success of the publication for their responses to the data request. The Bureau would be grateful to receive contributions and recommendations from concerned bodies and individuals as a form of feedback that will add values and also enrich subsequent editions. LAGOS BUREAU OF STATISTICS MINISTRY OF ECONOMIC PLANNING AND BUDGET BLOCK 19, THE SECRETARIAT, ALAUSA, IKEJA, LAGOS. Email: [email protected], [email protected] TABLE OF CONTENTS TABLE PAGE PREFACE DEMOGRAPHY 1.1 Area of land mass/water area of the old Twenty Local Government 1 Structure in Lagos State. 1.2 Population by sex according to Local Government Area in Lagos State: 2 2006 1.3 Local Government Area by Population Density 2006 3 1.4 Population Projections of the Local Government Area and their 4 Respective Population Density 2006, 2011‐2017 MANPOWER DISTRIBUTION 2.1 Manpower Distribution by Profession and Gender According 5‐6 to Local Government/Local Council Development Areas: Year 2016. -

Avon HMO Hospital List
Avon HMO Hospital List Life Family Premium Boss Hospital State Couple Starter Life Life Life CHRIST THE KING HOSPITAL, ABA Abia Yes Yes Yes Yes Yes EKEOMA MEMORIAL HOSPITAL Abia Yes Yes Yes Yes Yes FEDERAL MEDICAL CENTRE, UMUAHIA Abia Yes Yes Yes Yes Yes LIFE CARE CLINICS LTD Abia Yes Yes Yes Yes Yes LIVING WORD MISSION HOSPITAL Abia Yes Yes Yes Yes Yes NEW ERA HOSPITAL, UMUAHIA Abia Yes Yes Yes Yes Yes NEW ERA SPECIALIST HOSPITAL, ABA Abia Yes Yes Yes Yes Yes MUBI NEW LIFE HOSPITAL Adamawa Yes Yes Yes Yes Yes PEACE HOSPITAL Adamawa Yes Yes Yes Yes Yes CALEB MEDICAL CENTER Akwa Ibom Yes Yes Yes Yes Yes DOMINGO SPECIALIST HOSPITALS Akwa Ibom Yes Yes Yes Yes Yes EVERGREEN CHRISTIAN HEALTH SERVICES Akwa Ibom Yes Yes Yes Yes Yes GOOD SHEPHERD HOSPITAL Akwa Ibom Yes Yes Yes Yes Yes MOUNT OLIVE MEDICAL CENTRE Akwa Ibom Yes Yes Yes Yes Yes TOTAL CARE CLINIC AND MATERNITY Akwa Ibom Yes Yes Yes Yes Yes UBONG ABASI HOSPITAL Akwa Ibom Yes Yes Yes Yes Yes UWEM FOUNDATION SPECIALIST CLINIC Akwa Ibom Yes Yes Yes Yes Yes VEDDYSON HOSPITAL Akwa Ibom Yes Yes Yes Yes Yes CHIBUZOR HOSPITAL & MATERNITY EKWULOBIA Anambra Yes Yes Yes Yes Yes Hospital List CHIZARAM HOSPITAL AND MATRENITY Anambra Yes Yes Yes Yes Yes CHRIST THE KING SPECIALIST & CHILDREN HO Anambra Yes Yes Yes Yes Yes FELIX OKOLO MEMORIAL HOSPITAL(SPECIALIST Anambra Yes Yes Yes Yes Yes IYI ENU MISSION HOSPITAL Anambra Yes Yes Yes Yes Yes KANAYO SPECIALIST HOSPITAL & MATERNITY Anambra Yes Yes Yes Yes Yes LIFE SPECIALIST HOSPITAL Anambra Yes Yes Yes Yes Yes MERCY SPECIALIST HOSPITAL & MATERNITY -

Echocardiographic Characteristics of Nigerian Children with Adenoidal
nal atio Me sl d n ic a in r e T Animasahun et al., Transl Med (Sunnyvale) 2016, 6:4 Translational Medicine DOI: 10.4172/2161-1025.1000189 ISSN: 2161-1025 Research Article Open Access Echocardiographic Characteristics of Nigerian Children with Adenoidal Hypertrophy: A Multicenter Study Barakat Adeola Animasahun*, Motunrayo O Adekunle, Henry Olusegun Gbelee and Olisamedua Fidelis Njokanma Department of Paediatrics Lagos State University Teaching Hospital Ikeja, Lagos, Nigeria *Corresponding author: Adeola Barakat Animasahun, Lagos State University College of Medicine, Lagos, Nigeria, Tel: +2348055341166; Fax: 2348037250264; E-mail: [email protected] Recieved date: October 27, 2016; Accepted date: November 07, 2016; Published date: November 14, 2016 Copyright: © 2016 Animasahun AB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Background: Adenoidal hypertrophy is a common respiratory disease in childhood with a lethal complication of Cor-Pulmonale. There are few studies on the prevalence of adenoidal hypertrophy in children in Nigeria. The aim of the current study is to document the echocardiographic characteristics of Nigerian Children with adenoidal hypertrophy and compare the findings with those of other children in other parts of the world. Method: The study was prospective, involving subjects from three centers which were; a tertiary hospital, a private hospital and a major cardiology center. Children with clinical and radiological diagnosis of adenoidal hypertrophy had transthoracic echocardiography done by a cardiologist. Results: A total of 1,346 children had echocardiography done within the three years studied period in the centers. -

CALL for PAPERS PAGE
WORLD SAFETY ORGANIZATION Newsletter [email protected] May/June 2015 PAGE 28th WSO International CALL for PAPERS 10 Environmental & Occupational October 25–28, 2015 Safety & Health Professional Development Symposium Solaire Resort & Casino | Manila, Philippines The 28th WSO Symposium is for you if you are: a WSO member, community leader, professional involved in the fields of Environmental or Occupa- tional Safety and Health, Transportation Safety, Loss Control Consulting, Hazardous Materials Management, Hazardous Waste Management, Fire Service, Construction Safety, Insurance, Workers’ Compensation, and all other related fields; at the corporate, managerial, and operational level; with the community, state, or federal agencies; with private industry; or associated with an educational institution, etc. The Symposium presentations this year will focus on “how to further improve the safety and health of workers by ensuring an accident and illness free workplace, improving their quality of life, and enabling them to have More Fun Being Safe! This important theme of the 2015 Symposium is how we learn from one another’s experiences in different organizations and countries. The Symposium will focus on how to develop cooperation between different organizations and cross-disciplinary research that addresses safety promotion and injury prevention. The Symposium will provide a unique opportunity for corporate managers and executives, safety, health & environmental professionals, advo- cates of safety and accident prevention, leaders of safety organizations and WSO members from around the world where the WSO is represented through the WSO International/National Offices, WSO Chapters, and individual members. The Symposium will provide a forum for information ex- change, networking, professional contact with other members and safety professionals, but most of all, learning about new programs and gaining professional knowledge at sessions, panels, and workshops presented during the Symposium. -

March 2020 Case Study Examination Instructi
ICAN/201/V/C5 Examination No......................... THE INSTITUTE OF CHARTERED ACCOUNTANTS OF NIGERIA PROFESSIONAL LEVEL EXAMINATION – MARCH 2020 CASE STUDY EXAMINATION INSTRUCTIONS PLEASE READ THESE INSTRUCTIONS BEFORE THE COMMENCEMENT OF THE PAPER 1. Check your pockets, purse, mathematical set, etc. to ensure that you do not have prohibited items such as telephone handset, electronic storage device, programmable devices or any form of written material on you in the examination hall. You will be stopped from continuing with the examination and liable to further disciplinary actions including cancellation of examination result if caught. 2. Write your EXAMINATION NUMBER in the space provided above. 3. Do NOT write anything on your question paper EXCEPT your examination number. 4. Do NOT write anything on your docket. 5. Read all instructions in each section of the question paper carefully before answering the questions. 6. All solutions should be written in BLUE or BLACK INK. Any solution written in PENCIL or RED INK will not be marked. 7. Your solutions MUST BE on the CASE STUDY answer booklet. THURSDAY, MARCH 26, 2020 DO NOT TURN OVER UNTIL YOU ARE TOLD TO DO SO THE INSTITUTE OF CHARTERED ACCOUNTANTS OF NIGERIA PROFESSIONAL LEVEL EXAMINATION – MARCH 2020 CASE STUDY Time Allowed: 4 hours (including reading time) INSTRUCTION: YOU ARE TO USE THE CASE STUDY ANSWER BOOKLET FOR THIS PAPER This case material is issued prior to the examination to enable candidates familiarise themselves with the case scenario and to undertake any research and analysis as necessary. This pre-seen part of the Case Study examination is also published on the Institute’s website: www.ican.org/students. -

Nigerian Health Sector 1105 BM Amsterdam +31 (0)20 566 7158 Market Study Report March 2015
PharmAccess Trinity Building Pietersbergweg 17 Nigerian Health Sector 1105 BM Amsterdam +31 (0)20 566 7158 Market Study Report www.hifund.org March 2015 Nigerian Health Sector Market Study Report Study commissioned by the Embassy of the Kingdom of the Netherlands in Nigeria March 2015 2 ACRONYMS ACPN Association of Community Pharmacists of Nigeria CAC Corporate Affairs Commission of Nigeria CAGR Compound Annual Growth Rate CBHIS Community Based Health Insurance Scheme CME Continuing Medical Education CT Computed Tomography CVD Cardiovascular Diseases DFI Development Finance Institution ECG Electrocardiogram FDI Foreign Direct Investment FMOH Federal Ministry of Health GDP Gross Domestic Product HEFAMAA State Health Facility Monitoring and Accreditation Agency HIV Human Immunodeficiency Virus ICRC Infrastructure Concession Regulatory Commission IFC International Finance Corporation JV Joint Venture LGAs Local Government Areas MDGs Millennium Development Goals MGI McKinsey Global Institute MoU Memorandum of Understanding MRI Magnetic Resonance Imaging NAFDAC National Agency for Food and Drug Administration and Control NHIS National Health Insurance Scheme NMA Nigerian Medical Association NNRA Nigerian Nuclear Regulatory Authority OEM Original Equipment Manufacturer OOP Out of Pocket PMV Patent Medicine Vendors PPP Public Private Partnership SMOH State Ministry of Health THE Total Health Expenditure UHC Universal Health Coverage NIGERIAN HEALTH SECTOR MArkeT STUDY REPORT 3 4 TABLE OF contEnts 1. Introduction 7 2. Overview 9 21. Socio-economic overview 9 2.2. Health sector overview 10 3. Interesting developments for Dutch companies 15 3.1. Increasing burden of non-communicable diseases and medical tourism 15 3.2. Upgrade of public tertiary hospitals 16 3.3. Public Private Partnerships 17 3.4. -

Hci Healthcare
HCI HEALTHCARE NATIONAL HOSPITAL NETWORK HEAD OFFICE: 296,HERBERT MACUALAY WAY,SABO, YABA, LAGOS Tel 01-4489820, 07030009099 Abuja Office: N01 Nairobi Street, Off Aminu Kano Crescent, Wuse 2, Abuja. Tel: 08052099066, 08052099071 Zonal Offices:Bauchi, Enugu, Kano, Port-Harcourt. Enquiries: 07034039098. Call Centre: 01-4489820. Fax: 01-4489821 E-mail:[email protected], Website: www.healthcare-ng.com STATE LGA TOWN/CITY HOSPITAL NAME ADDRESS PLAN TYPE Aba South Aba New Era Hospital Ltd 213/215 Azikiwe road, P.O.Box 2390, Aba All Plans Osisioma Living Word Hospital 5/7 Umuocham Street, Off Aba- Owerri Road, Aba All Plans Aba South Mendel Hospital 20, Tenant Road, Aba All Plans Obingwa Alpha Inland Hospital 36, Glass Industry Road, Aba All Plans Aba South St. Anthony's Hospital 62/80 Etche Road, Aba All Plans Aba North Zikora Medical Center Ogbor Hill Aba,Abia. All Plans ABIA Aba North Life Care Clinics Ltd 8, Eziukwu Road, P.O.Box 4742, Aba All Plans Umuahia South Umuahia Madonna Catholic Hospital Aba road, Umuahia All Plans Umuahia South Ngozi Hospital 9, Warri Street, All Plans Umuahia North Healing Cross Hospital Km 2, Bende Road, Umuahia All Plans Umuahia North OBIOMA HOSPITAL & MATERNIITY 21 School Rd,Umuahia All Plans Block 3, Amuzukwu Road, Amuzukwu Layout, (Near 85 Umuahia North Hammer Smith Medical Centre Uwalaka), Umuahai All Plans AMAC Abuja FCT Amana Medical Centre No 5.Ilorin Street, Off Ogbomosho Street, Area 8,Garki Titanium Ultra, Deluxe and Royal Plans AMAC Bio Royal Hospital 190, Okene/Jebba Close, Area 2, Garki All Plans No.