PROBLEMS and CHALLENGES in MEETING the STANDARDS for EFFECTIVE RADIOTHERAPY DELIVERY in NIGERIA Timothy Akpa
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
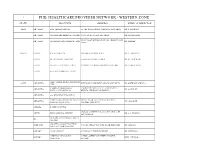
Phb Healthcare Provider Network - Western Zone
1 PHB HEALTHCARE PROVIDER NETWORK - WESTERN ZONE STATE PROVIDER ADDRESS MEDICAL DIRECTOR EKITI ADO-EKITI ADE-TADE HOSPITAL 55, OKE-BOLA STREET, AJILOSUN, ADO-EKITI DR. T. ADEDAPO ADO-EKITI FASANMADE MEDICAL CENTRE 93, IWOROKO ROAD, ADO-EKITI DR. FASANMADE 12, LITTLE BY LITTLE ROAD OFF ADEBAYO,ADO- ADO-EKITI OLUMORIN SPECIALIST HOSPITAL DR. LADELE EKITI KWARA ILORIN BALM HOSPITAL 29B, BISHOP STREET G.R.A. DR. A. ADEDAYO ILORIN OLANREWAJU HOSPITAL 5, ORO-AGO CLOSE, ILORIN DR. OLANREWAJU ILORIN OLAOLU HOSPITAL ILORIN 173 MURTALA MOHAMMED WAY, ILORIN DR OLORUNTOBA ILORIN ANCHOR MEDICAL CENTRE FIRST ALPHA MEDICAL CENTRE OGUN ABEOKUTA KUFUROJI OLUBI DRIVE,ADIGBE ABEOKUTA DR. ADEWALE ADEOLA LTD JOSEPH & CHRISTIANA 5, SURULERE STREET OFF LALUBU STREET ABEOKUTA DR. OGUNGBE SPECIALIST HOSPITAL BEHIND AFRI-BANK OKE-ILEWO ABEOKUTA SACRED HEART HOSPITAL MERCY GROUP CLINICS (MERCY MERCY ROAD, BEHIND UBA BUILDING ABEOKUTA MR. OMOJOYE COMPANY NIG. LTD) PANSEKE ABEOKUTA AGBARA ROPHE HOSPITAL 1 JOLASCO STREET, JOLASCO BUS STOP, OFF AKUTE BLISS MEDICAL CENTRE DR. A.A. WAHAB AKUTE ROAD. DEMARK CLINIC&MATERNITY IFO CENTRE AMAZING GRACE HOSPITAL IJEBU-ODE 7, ILORO STREET,OFF NEW ROAD IJEBU-ODE DR. ADELAJA (KETONIC MEDICAL LTD) SAGAMU ALPHA CLINIC 3, CATHOLIC CHURCH STREET DR. ODUWOLE MEDYTOP SPECIALIST 3, EJIMO ALEBIOSUN STREET,OJUMELE SAGAMU PROF. ODUSOGA HOSPITAL SAGAMU SANGO-OTA ACE MEDICARE CLINIC LTD KM 4, IDI- IROKO ROAD SANGO- OTA DR. KUKOYI 37, AKINWUNMI STREET{JOJO ROAD} G.R.A. SANGO-OTA FARAMED CLINICS DR. FARAYIBI SANGO OTTA ONDO AKURE FUJAH SPECIALIST HOSPITAL 22, AYETUTU STREET OPP. ISIKAN MARKET DR. FUJAH C/31, OWATUMISE STREET,BEHIND STATE AKURE INLAND MEDICAL CENTRE DR. -
(2017) Abstract of Local Government Statistics
LAGOS STATE GOVERNMENT ABSTRACT OF LOCAL GOVERNMENT STATISTICS 2017 LAGOS BUREAU OF STATISTICS MINISTRY OF ECONOMIC PLANNING AND BUDGET, SECRETARIAT, ALAUSA, IKEJA. PREFACE The Abstract of Local Government Statistics is a yearly publication produced by the Lagos Bureau of Statistics (LBS). This edition contains detailed information on Y2016 Socio Economic Statistics of the 57 Local Government and Local Council Development Areas (LG/LCDAs) in Lagos State. The activities of the LG\LCDAS are classified into ten (10) components, these are: demographic distributions and nine (9) Classifications of functions of Government (COFOG). This publication is useful to all and sundry both locally and internationally for researchers, planners, private organizations and Non Governmental Organizations to mention but a few. The State wishes to express its appreciation to the officials of the Local Government and Local Council Development Areas (LG/LCDAs) and all Agencies that contributed to the success of the publication for their responses to the data request. The Bureau would be grateful to receive contributions and recommendations from concerned bodies and individuals as a form of feedback that will add values and also enrich subsequent editions. LAGOS BUREAU OF STATISTICS MINISTRY OF ECONOMIC PLANNING AND BUDGET BLOCK 19, THE SECRETARIAT, ALAUSA, IKEJA, LAGOS. Email: [email protected], [email protected] TABLE OF CONTENTS TABLE PAGE PREFACE DEMOGRAPHY 1.1 Area of land mass/water area of the old Twenty Local Government 1 Structure in Lagos State. 1.2 Population by sex according to Local Government Area in Lagos State: 2 2006 1.3 Local Government Area by Population Density 2006 3 1.4 Population Projections of the Local Government Area and their 4 Respective Population Density 2006, 2011‐2017 MANPOWER DISTRIBUTION 2.1 Manpower Distribution by Profession and Gender According 5‐6 to Local Government/Local Council Development Areas: Year 2016. -

Avon HMO Hospital List
Avon HMO Hospital List Life Family Premium Boss Hospital State Couple Starter Life Life Life CHRIST THE KING HOSPITAL, ABA Abia Yes Yes Yes Yes Yes EKEOMA MEMORIAL HOSPITAL Abia Yes Yes Yes Yes Yes FEDERAL MEDICAL CENTRE, UMUAHIA Abia Yes Yes Yes Yes Yes LIFE CARE CLINICS LTD Abia Yes Yes Yes Yes Yes LIVING WORD MISSION HOSPITAL Abia Yes Yes Yes Yes Yes NEW ERA HOSPITAL, UMUAHIA Abia Yes Yes Yes Yes Yes NEW ERA SPECIALIST HOSPITAL, ABA Abia Yes Yes Yes Yes Yes MUBI NEW LIFE HOSPITAL Adamawa Yes Yes Yes Yes Yes PEACE HOSPITAL Adamawa Yes Yes Yes Yes Yes CALEB MEDICAL CENTER Akwa Ibom Yes Yes Yes Yes Yes DOMINGO SPECIALIST HOSPITALS Akwa Ibom Yes Yes Yes Yes Yes EVERGREEN CHRISTIAN HEALTH SERVICES Akwa Ibom Yes Yes Yes Yes Yes GOOD SHEPHERD HOSPITAL Akwa Ibom Yes Yes Yes Yes Yes MOUNT OLIVE MEDICAL CENTRE Akwa Ibom Yes Yes Yes Yes Yes TOTAL CARE CLINIC AND MATERNITY Akwa Ibom Yes Yes Yes Yes Yes UBONG ABASI HOSPITAL Akwa Ibom Yes Yes Yes Yes Yes UWEM FOUNDATION SPECIALIST CLINIC Akwa Ibom Yes Yes Yes Yes Yes VEDDYSON HOSPITAL Akwa Ibom Yes Yes Yes Yes Yes CHIBUZOR HOSPITAL & MATERNITY EKWULOBIA Anambra Yes Yes Yes Yes Yes Hospital List CHIZARAM HOSPITAL AND MATRENITY Anambra Yes Yes Yes Yes Yes CHRIST THE KING SPECIALIST & CHILDREN HO Anambra Yes Yes Yes Yes Yes FELIX OKOLO MEMORIAL HOSPITAL(SPECIALIST Anambra Yes Yes Yes Yes Yes IYI ENU MISSION HOSPITAL Anambra Yes Yes Yes Yes Yes KANAYO SPECIALIST HOSPITAL & MATERNITY Anambra Yes Yes Yes Yes Yes LIFE SPECIALIST HOSPITAL Anambra Yes Yes Yes Yes Yes MERCY SPECIALIST HOSPITAL & MATERNITY -

Nigerian Health Sector 1105 BM Amsterdam +31 (0)20 566 7158 Market Study Report March 2015
PharmAccess Trinity Building Pietersbergweg 17 Nigerian Health Sector 1105 BM Amsterdam +31 (0)20 566 7158 Market Study Report www.hifund.org March 2015 Nigerian Health Sector Market Study Report Study commissioned by the Embassy of the Kingdom of the Netherlands in Nigeria March 2015 2 ACRONYMS ACPN Association of Community Pharmacists of Nigeria CAC Corporate Affairs Commission of Nigeria CAGR Compound Annual Growth Rate CBHIS Community Based Health Insurance Scheme CME Continuing Medical Education CT Computed Tomography CVD Cardiovascular Diseases DFI Development Finance Institution ECG Electrocardiogram FDI Foreign Direct Investment FMOH Federal Ministry of Health GDP Gross Domestic Product HEFAMAA State Health Facility Monitoring and Accreditation Agency HIV Human Immunodeficiency Virus ICRC Infrastructure Concession Regulatory Commission IFC International Finance Corporation JV Joint Venture LGAs Local Government Areas MDGs Millennium Development Goals MGI McKinsey Global Institute MoU Memorandum of Understanding MRI Magnetic Resonance Imaging NAFDAC National Agency for Food and Drug Administration and Control NHIS National Health Insurance Scheme NMA Nigerian Medical Association NNRA Nigerian Nuclear Regulatory Authority OEM Original Equipment Manufacturer OOP Out of Pocket PMV Patent Medicine Vendors PPP Public Private Partnership SMOH State Ministry of Health THE Total Health Expenditure UHC Universal Health Coverage NIGERIAN HEALTH SECTOR MArkeT STUDY REPORT 3 4 TABLE OF contEnts 1. Introduction 7 2. Overview 9 21. Socio-economic overview 9 2.2. Health sector overview 10 3. Interesting developments for Dutch companies 15 3.1. Increasing burden of non-communicable diseases and medical tourism 15 3.2. Upgrade of public tertiary hospitals 16 3.3. Public Private Partnerships 17 3.4. -

Hci Healthcare
HCI HEALTHCARE NATIONAL HOSPITAL NETWORK HEAD OFFICE: 296,HERBERT MACUALAY WAY,SABO, YABA, LAGOS Tel 01-4489820, 07030009099 Abuja Office: N01 Nairobi Street, Off Aminu Kano Crescent, Wuse 2, Abuja. Tel: 08052099066, 08052099071 Zonal Offices:Bauchi, Enugu, Kano, Port-Harcourt. Enquiries: 07034039098. Call Centre: 01-4489820. Fax: 01-4489821 E-mail:[email protected], Website: www.healthcare-ng.com STATE LGA TOWN/CITY HOSPITAL NAME ADDRESS PLAN TYPE Aba South Aba New Era Hospital Ltd 213/215 Azikiwe road, P.O.Box 2390, Aba All Plans Osisioma Living Word Hospital 5/7 Umuocham Street, Off Aba- Owerri Road, Aba All Plans Aba South Mendel Hospital 20, Tenant Road, Aba All Plans Obingwa Alpha Inland Hospital 36, Glass Industry Road, Aba All Plans Aba South St. Anthony's Hospital 62/80 Etche Road, Aba All Plans Aba North Zikora Medical Center Ogbor Hill Aba,Abia. All Plans ABIA Aba North Life Care Clinics Ltd 8, Eziukwu Road, P.O.Box 4742, Aba All Plans Umuahia South Umuahia Madonna Catholic Hospital Aba road, Umuahia All Plans Umuahia South Ngozi Hospital 9, Warri Street, All Plans Umuahia North Healing Cross Hospital Km 2, Bende Road, Umuahia All Plans Umuahia North OBIOMA HOSPITAL & MATERNIITY 21 School Rd,Umuahia All Plans Block 3, Amuzukwu Road, Amuzukwu Layout, (Near 85 Umuahia North Hammer Smith Medical Centre Uwalaka), Umuahai All Plans AMAC Abuja FCT Amana Medical Centre No 5.Ilorin Street, Off Ogbomosho Street, Area 8,Garki Titanium Ultra, Deluxe and Royal Plans AMAC Bio Royal Hospital 190, Okene/Jebba Close, Area 2, Garki All Plans No. -

Federal Government of Nigeria 2012 Budget Federal
FEDERAL GOVERNMENT OF NIGERIA 2012 BUDGET SUMMARY FEDERAL MINISTRY OF LAND AND HOUSING TOTAL TOTAL PERSONNEL OVERHEAD TOTAL TOTAL CODE MDA COST COST RECURRENT TOTAL CAPITAL ALLOCATION =N= =N= =N= =N= =N= MINISTRY OF 025000 LANDS & 1 HOUSING 5,803,793,227 378,608,608 6,182,401,835 41,919,081,732 48,101,483,567 TOTAL 5,803,793,227 378,608,608 6,182,401,835 41,919,081,732 48,101,483,567 NATIONAL ASSEMBLY 1756 2012 APPROPRIATION FEDERAL GOVERNMENT OF NIGERIA 2012 BUDGET 2012 APPROPRATION CODE LINE ITEM =N= TOTAL: MINISTRY OF LANDS & HOUSING 48,101,483,567 0250001 MINISTRY OF LANDS & HOUSING TOTAL ALLOCATION: 48,101,483,567 21 PERSONNEL COST 5,803,793,227 2101 SALARY 5,160,221,958 210101 SALARIES AND WAGES 5,160,221,958 21010101 CONSOLIDATED SALARY 5,160,221,958 2102 ALLOWANCES AND SOCIAL CONTRIBUTION 643,571,270 210202 SOCIAL CONTRIBUTIONS 643,571,270 21020201 NHIS 257,428,508 21020202 CONTRIBUTORY PENSION 386,142,762 22 TOTAL GOODS AND NON - PERSONAL SERVICES - GENERAL 378,608,608 2202 OVERHEAD COST 378,608,608 220201 TRAVEL& TRANSPORT - GENERAL 107,199,610 22020101 LOCAL TRAVEL & TRANSPORT: TRAINING 22,671,783 22020102 LOCAL TRAVEL & TRANSPORT: OTHERS 44,998,750 22020103 INTERNATIONAL TRAVEL & TRANSPORT: TRAINING 18,986,355 22020104 INTERNATIONAL TRAVEL & TRANSPORT: OTHERS 20,542,722 220202 UTILITIES - GENERAL 12,727,319 22020201 ELECTRICITY CHARGES 6,042,500 22020202 TELEPHONE CHARGES 3,424,083 22020203 INTERNET ACCESS CHARGES 871,934 22020205 WATER RATES 1,885,260 22020206 SEWERAGE CHARGES 503,542 220203 MATERIALS & SUPPLIES - GENERAL -

List of Coded Health Facilities in LAGOS STATE.Pdf
LAGOS STATE HEALTH FACILITY LISTING LGA WARD NAME OF HEALTH FACILITY FACILITY TYPE OWNERSHIP CODE (PUBLIC/ PRIVATE) LGA STATE OWNERSHIP FACILITY NO FACILITY FACILITY TYPE FACILITY Madek Hospital And Maternity Home Primary Private 24 01 1 2 0001 Atobaje Adu Medical Clinic Primary Private 24 01 1 2 0002 Motolani Medical Centre Secondary Private 24 01 2 2 0003 Mayflower Clinic & Maternity Home Primary Private 24 01 1 2 0004 Awori Habibat Convalescent Home Primary Private 24 01 1 2 0005 Desmond Dental Clinic Primary Private 24 01 1 2 0006 Promise Medical Centre Secondary Private 24 01 2 2 0007 Mobonike Hospital Secondary Private 24 01 2 2 0008 E-Cares Medical Centre Primary Private 24 01 1 2 0009 Aisha Memorial Nursing Home Primary Private 24 01 1 2 0010 Dopemu Cradle Medical Ltd Primary Private 24 01 1 2 0011 Al-Imaan Hospital & Maternity Home Primary Private 24 01 1 2 0012 Olaotan Nursing Home Primary Private 24 01 1 2 0013 Dopemu PHC Primary Public 24 01 1 1 0014 Salam-Salam Nursing Home Primary Private 24 01 1 2 0015 Isale odo Country Home Clinic Primary Private 24 01 1 2 0016 Beta Hospital Secondary Private 24 01 2 2 0017 St Sabina Clinic Primary Private 24 01 1 2 0018 St Victoria Maternity Home Primary Private 24 01 1 2 0019 Best Hope Clinic Primary Private 24 01 1 2 0020 Prime Health Gate Medicare Primary Private 24 01 1 2 0021 Isale oja T Happy Home Clinic Primary Private 24 01 1 2 0022 White Chapel Hospital Secondary Private 24 01 2 2 0023 Iloro PHC Primary Public 24 01 1 1 0024 Dopemu HP Primary Public 24 01 1 1 0025 Krobon Hospital -
Interns' Knowledge of Clinical Pharmacology and Therapeutics
BMC Medical Education BioMed Central Research article Open Access Interns' knowledge of clinical pharmacology and therapeutics after undergraduate and on-going internship training in Nigeria: a pilot study Kazeem A Oshikoya*1,2, Idowu O Senbanjo2 and Olufemi O Amole1 Address: 1Pharmacology Department, Lagos State University College of Medicine, P.M.B 21266, Ikeja, Lagos, Nigeria and 2Paediatric Department, Lagos State University Teaching Hospital, Ikeja, Lagos, Nigeria Email: Kazeem A Oshikoya* - [email protected]; Idowu O Senbanjo - [email protected]; Olufemi O Amole - [email protected] * Corresponding author Published: 28 July 2009 Received: 25 February 2009 Accepted: 28 July 2009 BMC Medical Education 2009, 9:50 doi:10.1186/1472-6920-9-50 This article is available from: http://www.biomedcentral.com/1472-6920/9/50 © 2009 Oshikoya et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Background: A sound knowledge of pathophysiology of a disease and clinical pharmacology and therapeutics (CPT) of a drug is required for safe and rational prescribing. The aim of this study was therefore to assess how adequately the undergraduate CPT teaching had prepared interns in Nigeria for safe and rational prescribing and retrospectively, to know how they wanted the undergraduate curriculum to be modified so as to improve appropriate prescribing. The effect of internship training on the prescribing ability of the interns was also sought. -

Download Hospital List
BAND S/N NAME OF PROVIDER ADDRESS LOCATION STATE LGA ABIA A* 1 Living Word Mission 5/7, Umuocham street, Obayi, Aba Aba Abia ABA SOUTH A* 2 Life care clinics Ltd 8, Ezinkwu Street Aba, Aba Abia ABA SOUTH A* 3 New Era Hospital, 213/215 Azikiwe Road, Aba Aba Abia ABA SOUTH A* 4 New Era Hospital, 90B Orji River Road, Umuahia Umuahia Abia UMUAHIA SOUTH A* 5 J-Medicare Hospital 73, Bonny Street, Umuahia By Enugu Road Umuahia Abia A* 6 Obioma Hospital & Mat. 21, School road, umuahia Umuahia Abia UMUAHIA NORTH ABUJA B* 1 Limi Hospital & Maternity Ltd Plot 541, Behind ICPC, Central Area, Central Central Abuja MUNICIPAL Rouz Hospital & Maternity 10,Mobolaji Johnson street,Apo Quarters,Zone D,2nd Gate,Gudu District Abuja Abuja A* 2 MUNICIPAL A* 3 Adonai Hospital 3, Adonai Close, Mararaba, Garki Garki Abuja MUNICIPAL A* 4 Jerab Hospital Plot 145, Kutunku, Near Radio House, Gwagwalada Gwagwalada Abuja GWAGWALADA A* 5 Kingscare Hosp. Mararaba Along Keffi Rd, Mararaba Road, Mararaba Mararaba Abuja A* 6 Sauki Private Hospital Wuse Zone 6, Wuse Wuse Abuja MUNICIPAL A* 7 King's Care Hospital Plot 2181, Ibrahim Babangida Way, Wuse Zone 4., Wuse Wuse Abuja MUNICIPAL A* 8 King's Care Hospital (Kubwa) 7, Chrismass road, Behind Police affairs, Kubwa Kubwa Abuja BWARI A* 9 Living Stream Specialist Medical Centre 43/45, Street A, Phase 1, off University road, Gwagwalada Abuja Gwagwalada A* 10 Sisters of Nativity Hospital Phase 1, Jikwoyi, Abuja Municipal Area Council Abuja Abuja B* 11 LIfePoint Medical Centre Mabushi FCT, Abuja Abuja A* 12 Pan Raf Hospital Nyanya -

Accredited Healthcare Providers
ACCREDITED HEALTHCARE PROVIDERS HEALTHCARE PROVIDERS'HEALTHCARE CODE PROVIDRES KEY AB/0001/P Sancta Maria Specialist & Mat. AB - ABIA AB/0002/P All Saints Hospital AD - ADAMAWA AB/0003/P Janent Memorial Hospital AK - AKWA IBOM AB/0004/P Abia State University Teaching Hospital AN - ANAMBRA AB/0005/P Life Care Clinics Ltd BA - BAUCHI AB/0006/P New Era Specialist Hospital BN - BENUE AB/0007/P John Okarie Memorial Hospital BO - BORNO AB/0008/P St.Anthony's Hospital BY - BAYELSA AB/0009/S Sancta Maria Specialist Hospital CR - CROSS RIVER AB/0010/S Abia State University Teaching Hospital DT - DELTA AB/0011/S New Era Specialist Hospital EB - EBONYI AB/0012/S Ucheoma Hospital ED - EDO AB/0013/P Delta Hospital Ltd. EK - EKITI AB/0014/P Federal Medical Centre, Umuahia EN - ENUGU AB/0015/P Obioma Hospital & Maternity FCT - ABUJA AB/0016/P Priscillia Memorial Hospital GM - GOMBE AB/0017/S Federal Medical Centre IM - IMO AB/0018/P General Hospital, Ama-Achara JG - JIGAWA AB/0019/P Mendel Hospital KB - KEBBI AB/0020/P Clehansan Hospital & Maternity KD - KADUNA AB/0022/P Alpha Inland Hospital KG - KOGI AB/0023/P Todac Clinic Ltd. KN - KANO AB/0024/P Living Word Hospital KT - KATSINA AB/0025/P Living Word Hospital KW - KWARA AB/0027/P Ebemma Hospital LA - LAGOS AB/0028/P Horstman Hospital NG - NIGER AB/0030/P Princess May Specialist Hospital NW - NASARAWA AB/0031/P Austin Grace Hospital OD - ONDO AB/0034/P St. Paul Hospital OG - OGUN AB/0035/P Seven Days Adventist Hospital OS - OSUN AB/0036/P New Lead Hospital & Mat. -

Nigeria Provider List
Contents ABIA 4 ABUJA (FCT) 6 ADAMAWA 18 AKWA IBOM 19 ANAMBRA 22 BAUCHI 24 BAYELSA 25 BENUE 26 BORNO 28 CROSS RIVER 29 DELTA 31 EBONYI 35 EDO 36 EKITI 38 ENUGU 39 GOMBE 41 IMO 42 JIGAWA 44 KADUNA 45 KANO 47 KATSINA 49 KEBBI 50 KOGI 51 KWARA 52 2 of 116 LAGOS 53 NASARAWA 91 NIGER 92 OGUN 93 ONDO 97 OSUN 98 OYO 99 PLATEAU 103 RIVERS 104 SOKOTO 115 TARABA 116 3 of 116 ABIA Hospital Name State or Region Address CHRISTIANA DENTAL ABIA 24 AZIKIWE ROAD, UMUAHIA CLINIC ROYAL DENTAL CLINIC ABIA 51, SCHOOL ROAD, ABA NIGER OPTICAL- ABA ABIA 18 ASA ROAD NIGER OPTICAL- UMUAHIA ABIA 12 BENDE ROAD ROYAL EYE CLINIC ABIA 51, SCHOOL ROAD, ABA SHALOM EYE CENTRE ABIA DANPET AVENUE OFF 190 ABA OWERRI ROAD, ABA ZENITH EYE CARE CENTRE ABIA 71 /73ABA-OWERRI ROAD, UMUNGASI (ROSEVINE HOSPITAL) ABA AUSTINE GRACES ABIA 16, OKIGWE ROAD, ABA HOSPITAL LTD HEALING CROSS ABIA KLM 2, OFF BENDE ROAD, UMUAHIA HOSPITAL HORSTMAN HOSPITAL ABIA 32 OKIGWE ROAD, ABA IVORY HOSPITAL LIMITED ABIA 175 FAULKS ROAD BY POWERLINE, ABA LIFE CARE CLINIC ABIA 120A OLD GRA BEHIND SLOT OPPOSITE ABIA POLY ABA MARANATHA HOSPITAL ABIA 1, AMUZUKWU ROAD, UMUAHIA NEW ERA HOSPITAL ABIA 90B, OJI RIVER STREET, UMUAHIA PRISCILLA MEMORIAL ABIA 32 BONNY STREET UMUAHIA HOSPITAL ROMALEX HOSPITAL ABIA 45 UMUIMO ROAD ROAD ABAYI ABA ROSEVINE HOSPITAL ABIA 1 SHALOM WAY OFF 70 ABA-OWERRI ROAD, ABA SIMEONE SPECIALIST ABIA 2/4 ABAGANA STREET, OFF 156 ABA- OWERRI ROAD, OPP HOSPITAL EJINAKA BUS STOP, UMUOCHA, ABA 4 of 116 Hospital Name State or Region Address SPRINGS CLINIC ABIA 18, SCOTLAND CRESCENT, ABA ST. -

Receptivity of Pregnant Women in Lagos State to Communication Campaign Messages on Adoption of Insecticide Treated Nets for Malaria Prevention
RECEPTIVITY OF PREGNANT WOMEN IN LAGOS STATE TO COMMUNICATION CAMPAIGN MESSAGES ON ADOPTION OF INSECTICIDE TREATED NETS FOR MALARIA PREVENTION BY AMOBI THERESA IFEOMA MATRIC NO: 839009031 B.A. (HONS) Mass Comm., (UNN); MPA (UNILAG); M. Sc. Mass Comm., (UNILAG) Department of Mass Communication, School of Postgraduate Studies, University of Lagos, Lagos, Nigeria March, 2012 1 2 RECEPTIVITY OF PREGNANT WOMEN IN LAGOS STATE TO COMMUNICATION CAMPAIGN MESSAGES ON ADOPTION OF INSECTICIDE TREATED NETS FOR MALARIA PREVENTION BY AMOBI THERESA IFEOMA MATRIC NO: 839009031 B.A. (HONS) Mass Comm., (UNN); MPA (UNILAG); M. Sc. Mass Comm., (UNILAG) Department of Mass Communication, University of Lagos, Lagos, Nigeria THESIS SUBMITTED TO THE SCHOOL OF POSTGRADUATE STUDIES, UNIVERSITY OF LAGOS, IN PARTIAL FULFILMENT OF THE REQUIREMENTS FOR THE AWARD OF THE DEGREE OF DOCTOR OF PHILOSOPHY (Ph.D.) IN MASS COMMUNICATION MARCH, 2012 3 DECLARATION I, Theresa Ifeoma Amobi, declare that this Ph.D. thesis was originally written by me, and that to the best of my knowledge, this research has not been submitted to any other school or university for any other degree. I also declare that both published and unpublished materials used in this study are appropriately acknowledged. Name: Theresa Ifeoma Amobi Signature....................................................................... Date: 4 CERTIFICATION 5 TABLE OF CONTENTS Content Page First title page i Second title page ii Declaration iii Certification iv Table of contents v List of Acronyms vii List of tables/figures