Guidance for Family Healthcare Services
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Internal Ex-Post Evaluation for Technical Cooperation Project
Internal Ex-Post Evaluation for Technical Cooperation Project conducted by China Office: January, 2020 Country Name Project for Strengthening of Health Education for Prevention of Infectious Diseases People’s Republic of China through Family Health I. Project Outline Thirty years had passed since the implementation of family planning policy in the People’s Republic of China. In consequence, the birth rate had decreased, while some issues had emerged, such as the disproportionate ratio of male to female, and a drastic increase in migrant population. In other words, population issues had changed from a quantitative to a qualitative issue. In terms of health administration, the family planning system, which controls the family planning as well as the narrowly-defined “reproductive health (1)”, had a full-fledged network from the central down to the village level. Meanwhile, the health care system, which controls the maternal and child health as well as public health services, had some weaknesses in networks of rural areas. In this regard, the National Population and Family Planning Commission (hereafter, “NPFPC”) started to take some roles in promoting the maternal and child health as well as public health services, and their services were to reach to individual households of the entire population. Under the circumstances, the JICA technical cooperation project, namely “Project for Capacity Building of Reproductive Health and Family Care Service in Central and Western Region (2006-2009)” was carried out, which aimed at health improvement of the rural population by establishing family health services(2) as well as the capacity Background enhancement of health care providers at the NPFPC. -

Henan Wastewater Management and Water Supply Sector Project (11 Wastewater Management and Water Supply Subprojects)
Environmental Assessment Report Summary Environmental Impact Assessment Project Number: 34473-01 February 2006 PRC: Henan Wastewater Management and Water Supply Sector Project (11 Wastewater Management and Water Supply Subprojects) Prepared by Henan Provincial Government for the Asian Development Bank (ADB). The summary environmental impact assessment is a document of the borrower. The views expressed herein do not necessarily represent those of ADB’s Board of Directors, Management, or staff, and may be preliminary in nature. CURRENCY EQUIVALENTS (as of 02 February 2006) Currency Unit – yuan (CNY) CNY1.00 = $0.12 $1.00 = CNY8.06 The CNY exchange rate is determined by a floating exchange rate system. In this report a rate of $1.00 = CNY8.27 is used. ABBREVIATIONS ADB – Asian Development Bank BOD – biochemical oxygen demand COD – chemical oxygen demand CSC – construction supervision company DI – design institute EIA – environmental impact assessment EIRR – economic internal rate of return EMC – environmental management consultant EMP – environmental management plan EPB – environmental protection bureau GDP – gross domestic product HPG – Henan provincial government HPMO – Henan project management office HPEPB – Henan Provincial Environmental Protection Bureau HRB – Hai River Basin H2S – hydrogen sulfide IA – implementing agency LEPB – local environmental protection bureau N – nitrogen NH3 – ammonia O&G – oil and grease O&M – operation and maintenance P – phosphorus pH – factor of acidity PMO – project management office PM10 – particulate -
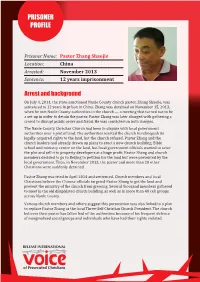
PRISONER PROFILE Prisoner Name: Pastor Zhang Shaojie Location: China
PRISONER PROFILE Prisoner Name: Pastor Zhang Shaojie Location: China Arrested: November 2013 Prisoner Name: Pastor Zhang Shaojie Sentence: 12 years’ imprisonment Location: China Arrested: November 2013 Arrest and background Sentence: 12 years imprisonment On July 4, 2014, the state-sanctioned Nanle CountyArrest church and pastor, background Shaojie Zhang, was sentenced to 12 years in prison in China. Zhang was detained onOn November July 4, 2014, the 15, state-sanctioned 2013, when Nanle Countyhe met church Nanle pastor, CountyShaojie, was sentenced to 12 years in prison in China. Zhang was detained on November 15, 2013, authorities in the church — a meeting that turned whenout heto met be Nanle a set-up County authorities in order in the to church detain — a meeting the pastor. Zhangthat turned Pastor out to be a set-up in order to detain the pastor. Pastor Zhang was later charged with gathering a Zhang was later charged with gathering a crowd tocrowd disrupt to disrupt public public order order and fraud.and Hefraud. was convicted He was on both convicted charges. on both charges. The Nanle County Christian Church had been in dispute with local government The alleged victim of fraud, Ms Li Cairen, has been authoritiesdetained over in a plot an of undisclosed land. The authorities location wanted the sincechurch to December relinquish its legally-acquired rights to the land, but the church refused. Pastor Zhang and the 21, 2013, when police caught her attempting to hidechurch from leaders them had already at the drawn Zhang up plans household.to erect a new church Pastor building, Zhang’s Bible lawyers explained that when Li’s son was killed in aschool work-related and ministry centre accident on the land, in but 2010, local government Zhang officialshelped wanted her to seize the plot and sell it to property developers at a huge profit. -

Addition of Clopidogrel to Aspirin in 45 852 Patients with Acute Myocardial Infarction: Randomised Placebo-Controlled Trial
Articles Addition of clopidogrel to aspirin in 45 852 patients with acute myocardial infarction: randomised placebo-controlled trial COMMIT (ClOpidogrel and Metoprolol in Myocardial Infarction Trial) collaborative group* Summary Background Despite improvements in the emergency treatment of myocardial infarction (MI), early mortality and Lancet 2005; 366: 1607–21 morbidity remain high. The antiplatelet agent clopidogrel adds to the benefit of aspirin in acute coronary See Comment page 1587 syndromes without ST-segment elevation, but its effects in patients with ST-elevation MI were unclear. *Collaborators and participating hospitals listed at end of paper Methods 45 852 patients admitted to 1250 hospitals within 24 h of suspected acute MI onset were randomly Correspondence to: allocated clopidogrel 75 mg daily (n=22 961) or matching placebo (n=22 891) in addition to aspirin 162 mg daily. Dr Zhengming Chen, Clinical Trial 93% had ST-segment elevation or bundle branch block, and 7% had ST-segment depression. Treatment was to Service Unit and Epidemiological Studies Unit (CTSU), Richard Doll continue until discharge or up to 4 weeks in hospital (mean 15 days in survivors) and 93% of patients completed Building, Old Road Campus, it. The two prespecified co-primary outcomes were: (1) the composite of death, reinfarction, or stroke; and Oxford OX3 7LF, UK (2) death from any cause during the scheduled treatment period. Comparisons were by intention to treat, and [email protected] used the log-rank method. This trial is registered with ClinicalTrials.gov, number NCT00222573. or Dr Lixin Jiang, Fuwai Hospital, Findings Allocation to clopidogrel produced a highly significant 9% (95% CI 3–14) proportional reduction in death, Beijing 100037, P R China [email protected] reinfarction, or stroke (2121 [9·2%] clopidogrel vs 2310 [10·1%] placebo; p=0·002), corresponding to nine (SE 3) fewer events per 1000 patients treated for about 2 weeks. -

Congressional-Executive Commission on China
CONGRESSIONAL-EXECUTIVE COMMISSION ON CHINA ANNUAL REPORT 2017 ONE HUNDRED FIFTEENTH CONGRESS FIRST SESSION OCTOBER 5, 2017 Printed for the use of the Congressional-Executive Commission on China ( Available via the World Wide Web: http://www.cecc.gov VerDate Nov 24 2008 16:24 Oct 04, 2017 Jkt 000000 PO 00000 Frm 00001 Fmt 6011 Sfmt 5011 U:\DOCS\26811 DIEDRE 2017 ANNUAL REPORT VerDate Nov 24 2008 16:24 Oct 04, 2017 Jkt 000000 PO 00000 Frm 00002 Fmt 6019 Sfmt 6019 U:\DOCS\26811 DIEDRE CONGRESSIONAL-EXECUTIVE COMMISSION ON CHINA ANNUAL REPORT 2017 ONE HUNDRED FIFTEENTH CONGRESS FIRST SESSION OCTOBER 5, 2017 Printed for the use of the Congressional-Executive Commission on China ( Available via the World Wide Web: http://www.cecc.gov U.S. GOVERNMENT PUBLISHING OFFICE 26–811 PDF WASHINGTON : 2017 For sale by the Superintendent of Documents, U.S. Government Publishing Office Internet: bookstore.gpo.gov Phone: toll free (866) 512–1800; DC area (202) 512–1800 Fax: (202) 512–2104 Mail: Stop IDCC, Washington, DC 20402–0001 VerDate Nov 24 2008 16:24 Oct 04, 2017 Jkt 000000 PO 00000 Frm 00003 Fmt 5011 Sfmt 5011 U:\DOCS\26811 DIEDRE CONGRESSIONAL-EXECUTIVE COMMISSION ON CHINA LEGISLATIVE BRANCH COMMISSIONERS Senate House MARCO RUBIO, Florida, Chairman CHRISTOPHER H. SMITH, New Jersey, JAMES LANKFORD, Oklahoma Cochairman TOM COTTON, Arkansas ROBERT PITTENGER, North Carolina STEVE DAINES, Montana TRENT FRANKS, Arizona TODD YOUNG, Indiana RANDY HULTGREN, Illinois DIANNE FEINSTEIN, California MARCY KAPTUR, Ohio JEFF MERKLEY, Oregon TIMOTHY J. WALZ, Minnesota GARY PETERS, Michigan TED LIEU, California ANGUS KING, Maine EXECUTIVE BRANCH COMMISSIONERS Department of State, To Be Appointed Department of Labor, To Be Appointed Department of Commerce, To Be Appointed At-Large, To Be Appointed At-Large, To Be Appointed ELYSE B. -

China's Green Bond Issuance and Investment Opportunity Report
China’s Green Bond Issuance and Investment Opportunity Report Report prepared by Climate Bonds Initiative and SynTao Green Finance Supported by UK PACT China’s Green Bond Issuance and Investment Opportunity Report Climate Bonds Initiative 1 Table of contents 1. Introduction and report highlights 3 Climate Bonds Initiative 2. China’s green investment potential 4 The Climate Bonds Initiative (Climate Bonds) is an international 3. China’s policy on green finance and 8 investor-focused not-for-profit organisation working to mobilise green bonds the USD100tn bond market for climate change solutions. 4. Opportunities for green bond issuance 12 It promotes investment in projects and assets needed for in China’s green finance pilot zones a rapid transition to a low carbon and climate resilient economy. The mission focus is to help drive down the cost of capital for large-scale climate and infrastructure projects and to Zhejiang Province support governments seeking increased capital markets investment to meet climate and greenhouse gas (GHG) Guangdong Province emission reduction goals. Xinjiang Province Climate Bonds carries out market analysis, policy research, market development; advises governments and regulators; Guizhou Province and administers the Climate Bonds Standards and Certification Scheme. Jiangxi Province Gansu Province 5. Moving forward: challenges and 18 opportunities to financing green projects in China 6. Appendices 20 Appendix 1: Green debt instruments Appendix 2: Sample Green Pipeline Appendix 3: Climate Bonds Taxonomy SynTao Green Finance SynTao Green Finance is a leading ESG service provider in China, that is dedicated to professional services in green finance and sustainable investment. It is committed to providing professional services ranging from ESG data and rating, green bond assurance, to the consulting and researching services in the sustainable investment and green finance areas. -

Zhang Shaojie (China)
Lent Prayer Project 2015 Week 1: Pray for Zhang Shaojie (China) Arrest and Sentence Zhang Shaojie (49) is pastor of Nanle County Christian Church in Henan province, central China, and is local president of the government-approved Three-Self Church. He was arrested in November 2013 after a dispute with local Communist Party officials who, according to church members, were trying to seize church land. In December 2013, a Sky News crew reporting on the church's plight and lawyers representing the Christians were attacked and expelled from the area by government officials. On 4 July 2014, he was sentenced to twelve years in prison for “gathering a crowd to disrupt public order” and fraud. Church members believe the government's persecution of Pastor Zhang stems from his defence of marginalised people who have had their rights violated, and that it is part of a plan to replace him as local Three-Self Church president. Rights lawyer Liu Weiguo said, "I strongly believe Zhang Shaojie is innocent. This is a total set-up by the local government." Meanwhile, Nanle County government officials have petitioned Nanle County People's Court to lengthen Pastor Zhang's sentence. Family Pastor Zhang’s eldest daughter Yunyun and her husband and baby daughter had to go into hiding, and in July 2014 they used China Aid's "underground railroad" to flee from China to the USA (pictured). On 5 November 2014, more than 20 officials violently abducted another daughter, Shanshan, and locked her in a soundproofed room. On the day of her release, 14 November, the authorities went to the Zhang family home to attempt to force the family to leave so the house and car could be auctioned, as Pastor Zhang had not paid 700,000 Yuan (€98,000) in restitution for his fraud charge. -

In the Face of Rapidly Deteriorating Status of Human Rights, It Is Time to Say “No” to Oppressors
In the face of rapidly deteriorating status of human rights, it is time to say “No” to oppressors Hearing of the Committee on Foreign Affairs to be held by the Subcommittee on Africa, Global Health, Global Human Rights, and International Organizations in Room 2172 of the Rayburn House Office Building DATE: Thursday, December 5, 2013 TIME: 11:00 a.m. SUBJECT: The Daughters Appeal to Beijing: “Let Our Fathers Go!” CHAIRMAN: Christopher H. Smith(R-NJ) Pastor Bob Fu, president of China Aid Association Honorable Chairman and Vice Chairman of the U.S. House Committee on Foreign Affairs, members of Congressmen, and friends, This is the third time in this year that I sit here to testify before the U. S. Congress, the international community, and all the people concerned with China’s human rights condition about the rapid deterioration of human rights condition in China. Having in front of me the five daughters of imprisoned men in China, who were sentenced to long prison terms simply because they held different views, peacefully expressed their views, or peacefully protested against the tyranny of the Chinese Communist authorities, and Chen Guangfu, brother of the Chinese blind rights defender Chen Guangcheng, whose son is still in prison and denied medical treatment he needs for his illness, I can’t express with words the pain and anger in my heart. China Aid Association has been monitoring China’s human rights condition for 11 years, and because we specifically focus on religious persecution, human rights violations, and the promotion of the rule of law in China, we got to know hundreds and thousands of sons, daughters and family members of the prisons of conscience like Ti-Anna Wang, Lisa Jiayin Peng, Grace Ge Geng, Bridgette Qiao Chen and Danielle Xiaodan Wang. -

China COI Compilation-March 2014
China COI Compilation March 2014 ACCORD is co-funded by the European Refugee Fund, UNHCR and the Ministry of the Interior, Austria. Commissioned by the United Nations High Commissioner for Refugees, Division of International Protection. UNHCR is not responsible for, nor does it endorse, its content. Any views expressed are solely those of the author. ACCORD - Austrian Centre for Country of Origin & Asylum Research and Documentation China COI Compilation March 2014 This COI compilation does not cover the Special Administrative Regions of Hong Kong and Macau, nor does it cover Taiwan. The decision to exclude Hong Kong, Macau and Taiwan was made on the basis of practical considerations; no inferences should be drawn from this decision regarding the status of Hong Kong, Macau or Taiwan. This report serves the specific purpose of collating legally relevant information on conditions in countries of origin pertinent to the assessment of claims for asylum. It is not intended to be a general report on human rights conditions. The report is prepared on the basis of publicly available information, studies and commentaries within a specified time frame. All sources are cited and fully referenced. This report is not, and does not purport to be, either exhaustive with regard to conditions in the country surveyed, or conclusive as to the merits of any particular claim to refugee status or asylum. Every effort has been made to compile information from reliable sources; users should refer to the full text of documents cited and assess the credibility, relevance and timeliness of source material with reference to the specific research concerns arising from individual applications. -

Nanle County Seat Wastewater Treatment Sub-Project Under Henan
REVISED RESETTLEMENT PLAN Nanle County Seat Wastewater Treatment Sub-project Under Henan Wastewater Management and Water Supply Sector Project IN THE PEOPLE’S REPUBLIC OF CHINA Nanle County Seat Wastewater Treatment Company August 2006 The resettlement plan is a document of the borrower. The views expressed herein do not necessarily represent those of ADB’s Board of Directors, Management, or staff, and may be preliminary in nature. 1 Endorsement Letter of the Resettlement Plan Nanle County Seat Wastewater Treatment Company has prepared the resettlement plan for Asian Development Bank (ADB) financed wastewater treatment project in our county. This resettlement plan fully complies with requirements of the relevant laws, regulations and policies of People’s Republic of China and Henan Province as well as complies with ADB’s policy on involuntary resettlement. Nanle County People’s Government hereby confirms the content of this resettlement plan and will guarantee the land acquisition, compensation and relocation budget being provided according to the provisions of this resettlement plan. This resettlement plan is based on the detailed design and the detailed measurement surveys. Signature of Head of the County: Wu Xinpu Nanle County People’s Government August 25th, 2006 2 ABBREVIATIONS RP Resettlement Plan PRC People’s Republic of China APs Affected Persons ADB Asian Development Bank FSR Feasibility study report EIA Environment Impact Assessment AAOV Annual Average Output Value WWTP Wastewater Treatment Plant (Project) LARO Land Acquisition -

2017 Annual Report .Pdf
CONGRESSIONAL-EXECUTIVE COMMISSION ON CHINA ANNUAL REPORT 2017 ONE HUNDRED FIFTEENTH CONGRESS FIRST SESSION OCTOBER 5, 2017 Printed for the use of the Congressional-Executive Commission on China ( Available via the World Wide Web: http://www.cecc.gov VerDate Nov 24 2008 16:24 Oct 04, 2017 Jkt 000000 PO 00000 Frm 00001 Fmt 6011 Sfmt 5011 U:\DOCS\26811 DIEDRE 2017 ANNUAL REPORT VerDate Nov 24 2008 16:24 Oct 04, 2017 Jkt 000000 PO 00000 Frm 00002 Fmt 6019 Sfmt 6019 U:\DOCS\26811 DIEDRE CONGRESSIONAL-EXECUTIVE COMMISSION ON CHINA ANNUAL REPORT 2017 ONE HUNDRED FIFTEENTH CONGRESS FIRST SESSION OCTOBER 5, 2017 Printed for the use of the Congressional-Executive Commission on China ( Available via the World Wide Web: http://www.cecc.gov U.S. GOVERNMENT PUBLISHING OFFICE 26–811 PDF WASHINGTON : 2017 For sale by the Superintendent of Documents, U.S. Government Publishing Office Internet: bookstore.gpo.gov Phone: toll free (866) 512–1800; DC area (202) 512–1800 Fax: (202) 512–2104 Mail: Stop IDCC, Washington, DC 20402–0001 VerDate Nov 24 2008 16:24 Oct 04, 2017 Jkt 000000 PO 00000 Frm 00003 Fmt 5011 Sfmt 5011 U:\DOCS\26811 DIEDRE CONGRESSIONAL-EXECUTIVE COMMISSION ON CHINA LEGISLATIVE BRANCH COMMISSIONERS Senate House MARCO RUBIO, Florida, Chairman CHRISTOPHER H. SMITH, New Jersey, JAMES LANKFORD, Oklahoma Cochairman TOM COTTON, Arkansas ROBERT PITTENGER, North Carolina STEVE DAINES, Montana TRENT FRANKS, Arizona TODD YOUNG, Indiana RANDY HULTGREN, Illinois DIANNE FEINSTEIN, California MARCY KAPTUR, Ohio JEFF MERKLEY, Oregon TIMOTHY J. WALZ, Minnesota GARY PETERS, Michigan TED LIEU, California ANGUS KING, Maine EXECUTIVE BRANCH COMMISSIONERS Department of State, To Be Appointed Department of Labor, To Be Appointed Department of Commerce, To Be Appointed At-Large, To Be Appointed At-Large, To Be Appointed ELYSE B. -
The 2018 Annual Report
CONGRESSIONAL-EXECUTIVE COMMISSION ON CHINA ANNUAL REPORT 2018 ONE HUNDRED FIFTEENTH CONGRESS SECOND SESSION OCTOBER 10, 2018 Printed for the use of the Congressional-Executive Commission on China ( Available via the World Wide Web: https://www.cecc.gov VerDate Nov 24 2008 19:55 Oct 09, 2018 Jkt 081003 PO 00000 Frm 00001 Fmt 6011 Sfmt 5011 K:\DOCS\31388.TXT DAVID 2018 ANNUAL REPORT VerDate Nov 24 2008 19:55 Oct 09, 2018 Jkt 081003 PO 00000 Frm 00002 Fmt 6019 Sfmt 6019 K:\DOCS\31388.TXT DAVID CONGRESSIONAL-EXECUTIVE COMMISSION ON CHINA ANNUAL REPORT 2018 ONE HUNDRED FIFTEENTH CONGRESS SECOND SESSION OCTOBER 10, 2018 Printed for the use of the Congressional-Executive Commission on China ( Available via the World Wide Web: https://www.cecc.gov U.S. GOVERNMENT PUBLISHING OFFICE 31–388 PDF WASHINGTON : 2018 VerDate Nov 24 2008 19:55 Oct 09, 2018 Jkt 081003 PO 00000 Frm 00003 Fmt 5011 Sfmt 5011 K:\DOCS\31388.TXT DAVID CONGRESSIONAL-EXECUTIVE COMMISSION ON CHINA LEGISLATIVE BRANCH COMMISSIONERS Senate House MARCO RUBIO, Florida, Chairman CHRISTOPHER H. SMITH, New Jersey, JAMES LANKFORD, Oklahoma Cochairman TOM COTTON, Arkansas ROBERT PITTENGER, North Carolina STEVE DAINES, Montana RANDY HULTGREN, Illinois TODD YOUNG, Indiana MARCY KAPTUR, Ohio DIANNE FEINSTEIN, California TIMOTHY J. WALZ, Minnesota JEFF MERKLEY, Oregon TED LIEU, California GARY PETERS, Michigan ANGUS KING, Maine EXECUTIVE BRANCH COMMISSIONERS Department of State, To Be Appointed Department of Labor, To Be Appointed Department of Commerce, To Be Appointed At-Large, To Be Appointed At-Large, To Be Appointed ELYSE B. ANDERSON, Staff Director PAUL B.