RX.PA.119.E.MPC REVISION DATE: 03/20 PAGE NUMBER: 1 of 3
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Epidemiology of Mucopolysaccharidoses Update
diagnostics Review Epidemiology of Mucopolysaccharidoses Update Betul Celik 1,2 , Saori C. Tomatsu 2 , Shunji Tomatsu 1 and Shaukat A. Khan 1,* 1 Nemours/Alfred I. duPont Hospital for Children, Wilmington, DE 19803, USA; [email protected] (B.C.); [email protected] (S.T.) 2 Department of Biological Sciences, University of Delaware, Newark, DE 19716, USA; [email protected] * Correspondence: [email protected]; Tel.: +302-298-7335; Fax: +302-651-6888 Abstract: Mucopolysaccharidoses (MPS) are a group of lysosomal storage disorders caused by a lysosomal enzyme deficiency or malfunction, which leads to the accumulation of glycosaminoglycans in tissues and organs. If not treated at an early stage, patients have various health problems, affecting their quality of life and life-span. Two therapeutic options for MPS are widely used in practice: enzyme replacement therapy and hematopoietic stem cell transplantation. However, early diagnosis of MPS is crucial, as treatment may be too late to reverse or ameliorate the disease progress. It has been noted that the prevalence of MPS and each subtype varies based on geographic regions and/or ethnic background. Each type of MPS is caused by a wide range of the mutational spectrum, mainly missense mutations. Some mutations were derived from the common founder effect. In the previous study, Khan et al. 2018 have reported the epidemiology of MPS from 22 countries and 16 regions. In this study, we aimed to update the prevalence of MPS across the world. We have collected and investigated 189 publications related to the prevalence of MPS via PubMed as of December 2020. In total, data from 33 countries and 23 regions were compiled and analyzed. -

Pathophysiology of Mucopolysaccharidosis
Pathophysiology of Mucopolysaccharidosis Dr. Christina Lampe, MD The Center for Rare Diseases, Clinics for Pediatric and Adolescent Medicine Helios Dr. Horst Schmidt Kliniken, Wiesbaden, Germany Inborn Errors of Metabolism today - more than 500 diseases (~10 % of the known genetic diseases) 5000 genetic diseases - all areas of metabolism involved - vast majority are recessive conditions 500 metabolic disorders - individually rare or very rare - overall frequency around 1:800 50 LSD (similar to Down syndrome) LSDs: 1: 5.000 live births MPS: 1: 25.000 live births 7 MPS understanding of pathophysiology and early diagnosis leading to successful therapy for several conditions The Lysosomal Diseases (LSD) TAY SACHS DIS. 4% WOLMAN DIS. ASPARTYLGLUCOSAMINURIA SIALIC ACID DIS. SIALIDOSIS CYSTINOSIS 4% SANDHOFF DIS. 2% FABRY DIS. 7% POMPE 5% NIEMANN PICK C 4% GAUCHER DIS. 14% Mucopolysaccharidosis NIEMANN PICK A-B 3% MULTIPLE SULPH. DEF. Mucolipidosis MUCOLIPIDOSIS I-II 2% Sphingolipidosis MPSVII Oligosaccharidosis GM1 GANGLIOSIDOSIS 2% MPSVI Neuronale Ceroid Lipofuszinois KRABBE DIS. 5% MPSIVA others MPSIII D A-MANNOSIDOSIS MPSIII C MPSIIIB METACHROMATIC LEUKOD. 8% MPS 34% MPSIIIA MPSI MPSII Initial Description of MPS Charles Hunter, 1917: “A Rare Disease in Two Brothers” brothers: 10 and 8 years hearing loss dwarfism macrocephaly cardiomegaly umbilical hernia joint contractures skeletal dysplasia death at the age of 11 and 16 years Description of the MPS Types... M. Hunter - MPS II (1917) M. Hurler - MPS I (1919) M. Morquio - MPS IV (1929) M. Sanfilippo - MPS III (1963) M. Maroteaux-Lamy - MPS IV (1963) M. Sly - MPS VII (1969) M. Scheie - MPS I (MPS V) (1968) M. Natowicz - MPS IX (1996) The Lysosome Lysosomes are.. -

Megalencephaly and Macrocephaly
277 Megalencephaly and Macrocephaly KellenD.Winden,MD,PhD1 Christopher J. Yuskaitis, MD, PhD1 Annapurna Poduri, MD, MPH2 1 Department of Neurology, Boston Children’s Hospital, Boston, Address for correspondence Annapurna Poduri, Epilepsy Genetics Massachusetts Program, Division of Epilepsy and Clinical Electrophysiology, 2 Epilepsy Genetics Program, Division of Epilepsy and Clinical Department of Neurology, Fegan 9, Boston Children’s Hospital, 300 Electrophysiology, Department of Neurology, Boston Children’s Longwood Avenue, Boston, MA 02115 Hospital, Boston, Massachusetts (e-mail: [email protected]). Semin Neurol 2015;35:277–287. Abstract Megalencephaly is a developmental disorder characterized by brain overgrowth secondary to increased size and/or numbers of neurons and glia. These disorders can be divided into metabolic and developmental categories based on their molecular etiologies. Metabolic megalencephalies are mostly caused by genetic defects in cellular metabolism, whereas developmental megalencephalies have recently been shown to be caused by alterations in signaling pathways that regulate neuronal replication, growth, and migration. These disorders often lead to epilepsy, developmental disabilities, and Keywords behavioral problems; specific disorders have associations with overgrowth or abnor- ► megalencephaly malities in other tissues. The molecular underpinnings of many of these disorders are ► hemimegalencephaly now understood, providing insight into how dysregulation of critical pathways leads to ► -
![Hurler Syndrome (Mucopolysaccharidosis Type 1) in a Young Female Patient [Version 1; Peer Review: 3 Approved with Reservations]](https://docslib.b-cdn.net/cover/5921/hurler-syndrome-mucopolysaccharidosis-type-1-in-a-young-female-patient-version-1-peer-review-3-approved-with-reservations-825921.webp)
Hurler Syndrome (Mucopolysaccharidosis Type 1) in a Young Female Patient [Version 1; Peer Review: 3 Approved with Reservations]
F1000Research 2020, 9:367 Last updated: 06 AUG 2021 CASE REPORT Case Report: Hurler syndrome (Mucopolysaccharidosis Type 1) in a young female patient [version 1; peer review: 3 approved with reservations] Sadaf Saleem Sheikh1, Dipak Kumar Yadav 2, Ayesha Saeed3 1Punjab Medical College, Faisalabad, Pakistan 2Nobel Medical College Teaching Hospital, Biratnagar, Nepal 3The Children’s Hospital, Institute of Child Health, Faisalabad, Pakistan v1 First published: 15 May 2020, 9:367 Open Peer Review https://doi.org/10.12688/f1000research.23532.1 Latest published: 15 May 2020, 9:367 https://doi.org/10.12688/f1000research.23532.1 Reviewer Status Invited Reviewers Abstract Hurler syndrome is a rare autosomal recessive disorder of 1 2 3 mucopolysaccharide metabolism. Here, we present the case of a young female patient who presented with features of respiratory version 1 distress. In addition, the patient had gingival hypertrophy, spaced 15 May 2020 report report report dentition, misaligned eruptive permanent dentition, microdontia, coarse facial features, low set ears, depressed nasal bridge, distended 1. Sanghamitra Satpathi , Hi-Tech Medical abdomen, pectus carinatum, umbilical hernia and J-shaped Sella Turcica on an X-ray of the skull. A diagnosis of Hurler syndrome College and Hospital, Rourkela, India (Mucopolysaccharidosis Type I) was made. The patient was kept on ventilator support from the third day; however, she died on the fifth 2. Alla N. Semyachkina , Research and day of admission. Enzyme replacement modality of treatment can Clinical Institute for Pediatrics of the Pirogov increase a patient's survival rate if an early diagnosis can be made. To Russian National Research Medical the best of our knowledge, only a few cases of Hurler syndrome have been reported in Pakistan. -

Medical Genetics and Genomic Medicine in the United States of America
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by George Washington University: Health Sciences Research Commons (HSRC) Himmelfarb Health Sciences Library, The George Washington University Health Sciences Research Commons Pediatrics Faculty Publications Pediatrics 7-1-2017 Medical genetics and genomic medicine in the United States of America. Part 1: history, demographics, legislation, and burden of disease. Carlos R Ferreira George Washington University Debra S Regier George Washington University Donald W Hadley P Suzanne Hart Maximilian Muenke Follow this and additional works at: https://hsrc.himmelfarb.gwu.edu/smhs_peds_facpubs Part of the Genetics and Genomics Commons APA Citation Ferreira, C., Regier, D., Hadley, D., Hart, P., & Muenke, M. (2017). Medical genetics and genomic medicine in the United States of America. Part 1: history, demographics, legislation, and burden of disease.. Molecular Genetics and Genomic Medicine, 5 (4). http://dx.doi.org/10.1002/mgg3.318 This Journal Article is brought to you for free and open access by the Pediatrics at Health Sciences Research Commons. It has been accepted for inclusion in Pediatrics Faculty Publications by an authorized administrator of Health Sciences Research Commons. For more information, please contact [email protected]. GENETICS AND GENOMIC MEDICINE AROUND THE WORLD Medical genetics and genomic medicine in the United States of America. Part 1: history, demographics, legislation, and burden of disease Carlos R. Ferreira1,2 , Debra S. Regier2, Donald W. Hadley1, P. Suzanne Hart1 & Maximilian Muenke1 1National Human Genome Research Institute, National Institutes of Health, Bethesda, Maryland 2Rare Disease Institute, Children’s National Health System, Washington, District of Columbia Correspondence Carlos R. -
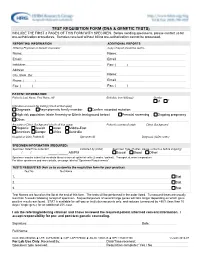
Test Requisition Form (Dna & Genetic Tests)
TEST REQUISITION FORM (DNA & GENETIC TESTS) INCLUDE THE FIRST 3 PAGES OF THIS FORM WITH SPECIMEN. Before sending specimens, please contact us for pre-authorization procedures. Samples received without billing pre-authorization cannot be processed. REPORTING INFORMATION ADDITIONAL REPORTS Ordering Physician or Genetic Counselor Copy of report should be sent to Name: Name: Email: Email: Institution: Fax: ( ) Address: City, State, Zip: Name: Phone: ( ) Email: Fax: ( ) Fax: ( ) PATIENT INFORMATION Patient's Last Name, First Name, MI Birthdate (mm/dd/yyyy) Gender M F Indication or reason for testing (check all that apply) Diagnosis Asymptomatic family member Confirm recorded mutation: High risk population (state Ancestry or Ethnic background below) Prenatal screening Ongoing pregnancy Other: Ancestry or Ethnic Background (check all that apply) Patient's country of origin Ethnic Background Hispanic Jewish Asian Middle-East Americas Europe Africa Australia Hospital or Clinic Patient ID Specimen ID Diagnosis (ICD9 codes) SPECIMEN INFORMATION (REQUIRED) Specimen Date/Time Collected Collected by (initial) Specimen Type (If other, please contact us before shipping) / / _____:_____ AM/PM Buccal Blood Other: Specimen may be submitted as whole blood or buccal epithelial cells (2 swabs / patient). Transport at room temperature. For other specimens and more details, see page labeled "Specimen Requirements". TESTS REQUESTED (Ask us to customize the requisition form for your practice) Test No. Test Name 1. Stat 2. Stat 3. Stat Test Names are found on the list at the end of this form. The tests will be performed in the order listed. Turnaround times are usually less than 5 weeks following receipt of specimen. Sequential panels of several large genes will take longer depending on which gene positive results are found. -

Anesthetic Considerations and Clinical Manifestations 243
MUCOPOLYSACCHARIDOSES: ANESTHETIC CONSIDERATIONS AND CLINICAL MANIFESTATIONS 243 MUCOPOLYSACCHARIDOSES: ANESTHETIC CONSIDERATIONS AND CLINICAL MANIFESTATIONS * ** *** JERMALE A. SAM , AMIR R. BALUCH , RASHID S. NIAZ , *** **** LINDSEY LONADIER AND ALAN D. KAYE Abstract Mucopolysaccharidosis (MPS) is a group of genetic disorders that presents challenges during anesthetic care and in particular difficulty with airway management. Patients should be managed by experienced anesthesiologists at centers that are familiar with these types of conditions. Rarely encountered disease states have been identified as important topics in the continuing education of clinical anesthesiologists. This review will define MPS, describe the pathophysiology of MPS, describe how patients with this rare lysosomal storage disorders have dysfunction of tissues, cite the incidence of MPS, list the clinical manifestations and specific problems associated with the administration of anesthesia to patients with MPS, present treatment options for patients with MPS, define appropriate preoperative evaluation and perioperative management of these patients, including, to anticipate potential postoperative airway problems. Introduction Mucopolysaccharidoses (MPS) are a group of rare genetic lysosomal storage disorders characterized by the deficiency in or complete lack of necessary lysosomal enzymes required for the stepwise breakdown of glycosaminoglycans (GAGs, also known as mucopolysaccharidoses)1-5. Consequently, fragments of GAGs accumulate intracellularly in the lysosome resulting in cellular enlargement causing disruption/dysfunction of structure and function of tissues. This process leads to numerous clinical abnormalities. Incidence of all types of MPS is reported to be between 1in 10,000 to 1 in 30,000 live births and are transmitted autosomal recessive except for MPS II which is X-linked1,4,5. Pathophysiology Glycosaminoglycans are long-chain complex carbohydrates consisting of repeating sulfated acidic and amino sugar disaccharide units. -

Long-Term Follow-Up Posthematopoietic Stem Cell Transplantation in a Japanese Patient with Type-VII Mucopolysaccharidosis
diagnostics Case Report Long-Term Follow-up Posthematopoietic Stem Cell Transplantation in a Japanese Patient with Type-VII Mucopolysaccharidosis Kenji Orii 1,*, Yasuyuki Suzuki 2 , Shunji Tomatsu 1,3,4, Tadao Orii 1 and Toshiyuki Fukao 1 1 Department of Pediatrics, Gifu University Graduate School of Medicine, Yanagido 1-1, Gifu 501-1194, Japan; [email protected] (S.T.); [email protected] (T.O.); [email protected] (T.F.) 2 Medical Education Development Center, Gifu University, Yanagido 1-1, Gifu 501-1194, Japan; [email protected] 3 Nemours/Alfred I. Dupont Hospital for Children, 1600 Rockland Rd., Wilmington, DE 19803, USA 4 Department of Pediatrics, Thomas Jefferson University, Philadelphia, PA 19144, USA * Correspondence: [email protected]; Tel.: +81-58-230-6386 Received: 15 January 2020; Accepted: 13 February 2020; Published: 16 February 2020 Abstract: The effectiveness of hematopoietic stem cell transplantation (HSCT) for type-VII mucopolysaccharidosis (MPS VII, Sly syndrome) remains controversial, although recent studies have shown that it has a clinical impact. In 1998, Yamada et al. reported the first patient with MPS VII, who underwent HSCT at 12 years of age. Here, we report the results of a 22-year follow-up of that patient post-HSCT, who harbored the p.Ala619Val mutation associated with an attenuated phenotype. The purpose of this study was to evaluate changes in physical symptoms, the activity of daily living (ADL), and the intellectual status in the 34-year-old female MPS VII patient post-HSCT, and to prove the long-term effects of HSCT in MPS VII. -

Ocular Manifestations of Inherited Diseases Maya Eibschitz-Tsimhoni
10 Ocular Manifestations of Inherited Diseases Maya Eibschitz-Tsimhoni ecognizing an ocular abnormality may be the first step in Ridentifying an inherited condition or syndrome. Identifying an inherited condition may corroborate a presumptive diagno- sis, guide subsequent management, provide valuable prognostic information for the patient, and determine if genetic counseling is needed. Syndromes with prominent ocular findings are listed in Table 10-1, along with their alternative names. By no means is this a complete listing. Two-hundred and thirty-five of approxi- mately 1900 syndromes associated with ocular or periocular manifestations (both inherited and noninherited) identified in the medical literature were chosen for this chapter. These syn- dromes were selected on the basis of their frequency, the char- acteristic or unique systemic or ocular findings present, as well as their recognition within the medical literature. The boldfaced terms are discussed further in Table 10-2. Table 10-2 provides a brief overview of the common ocular and systemic findings for these syndromes. The table is organ- ized alphabetically; the boldface name of a syndrome is followed by a common alternative name when appropriate. Next, the Online Mendelian Inheritance in Man (OMIM™) index num- ber is listed. By accessing the OMIM™ website maintained by the National Center for Biotechnology Information at http://www.ncbi.nlm.nih.gov, the reader can supplement the material in the chapter with the latest research available on that syndrome. A MIM number without a prefix means that the mode of inheritance has not been proven. The prefix (*) in front of a MIM number means that the phenotype determined by the gene at a given locus is separate from those represented by other 526 chapter 10: ocular manifestations of inherited diseases 527 asterisked entries and that the mode of inheritance of the phe- notype has been proven. -

Mucopolysaccharidosis VII in Brazil
Giugliani et al. Orphanet J Rare Dis (2021) 16:238 https://doi.org/10.1186/s13023-021-01870-w RESEARCH Open Access Mucopolysaccharidosis VII in Brazil: natural history and clinical fndings Roberto Giugliani1* , Anneliese Lopes Barth2, Melissa Rossi Calvão Dumas3, José Francisco da Silva Franco4, Liane de Rosso Giuliani5, Carlos Henrique Paiva Grangeiro6, Dafne Dain Gandelman Horovitz2, Chong Ae Kim7, Emilia Katiane Embiruçu de Araújo Leão8, Paula Frassinetti Vasconcelos de Medeiros9, Diego Santana Chaves Geraldo Miguel10, Maria Espírito Santo Almeida Moreira11, Helena Maria Guimarães Pimentel dos Santos3, Luiz Carlos Santana da Silva12, Luiz Roberto da Silva13, Isabel Neves de Souza14, Tatiele Nalin15 and Daniel Garcia15 Abstract Background: Mucopolysaccharidosis type VII (MPS VII), also known as Sly syndrome, caused by defciency of the lysosomal enzyme β-glucuronidase, is an ultra-rare disorder with scarce epidemiological data and few publications about natural history and clinical spectrum. Methods: We conducted a case series report which included retrospective data from all MPS VII patients diagnosed through the “MPS Brazil Network” who were known to be alive in 2020 in Brazil (N 13). Clinical data were obtained from a review of the medical records and descriptive statistics and variables were =summarized using counts and per- centages of the total population. Results: The majority of the patients were from the Northeast region of Brazil. Among the signs and symptoms that raised the clinical suspicion of MPS, coarse face was the most frequent; 58% of the patients had a history of non- immune hydrops fetalis. All the subjects presented short neck and trunk. The majority presented typical phenotypical signs of MPS disorders. -

Application Number
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 761047Orig1s000 CLINICAL REVIEW(S) Clinical Review BLA 761047 UX003/rhGUS UNIFIED CLINICAL REVIEW Application Type BLA Application Number(s) 761,047 Priority or Standard Priority Submit Date(s) March 16, 2017 Received Date(s) March 16, 2017 PDUFA Goal Date November 16, 2017 Division/Office ODEIII/DGIEP Review Completion Date November 16, 2017 Medical Officer Dina Zand, M.D. Cross Discipline Team Kathleen Donohue, M.D. Leader Deputy Division Director Dragos Roman, M.D. Director of the Office of Julie Beitz, M.D. Drug Evaluation III Established Name UX003/rhGUS (Proposed) Trade Name Mepsevii (vestronidase alfa) Applicant Ultragenyx Formulation(s) IV Dosing Regimen 4 mg/kg by IV every other week Applicant Proposed Sly Syndrome Indication(s)/Population(s) Recommendation on Approval Regulatory Action Recommended Patients with a confirmed diagnosis of Mucopolysaccharidosis Indication(s)/Population(s) type 7 (MPS VII) (if applicable) 1 Reference ID: 4181013 Clinical Review BLA 761047 UX003/rhGUS Table of Contents Glossary................................................................................................................................... 7 1 Executive Summary .......................................................................................................... 9 Product Introduction ........................................................................................................ 9 Conclusions on the Substantial Evidence of Effectiveness ............................................. -

A Guide to Understanding MPS VII
A Guide to Understanding MPS VII Sly Syndrome Table of Contents Introduction ..........................................................................................2 What causes MPS VII?............................................................................3 How common is MPS VII? ....................................................................4 How is MPS VII inherited? ....................................................................4 How is MPS VII diagnosed? ..................................................................5 Prenatal diagnosis ..................................................................................6 Clinical problems in MPS VII ..............................................................6 Nose, throat, chest and ear problems ..................................................8 Mouth....................................................................................................11 The National MPS Society exists to find cures for Heart......................................................................................................11 MPS and related diseases. We provide hope and Liver and spleen ..................................................................................12 support for affected individuals and their families through research, advocacy and awareness of Abdomen and hernias ........................................................................13 these devastating diseases. Bowel problems....................................................................................13