WHO, Child Health in Somalia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Somali Democratic Republic Ministry of Agriculture
Somali Democratic Republic Ministry of Agriculture Directorate of Planning and-Training /Food Security Project "Maize Supply and Price Situation in Somalia: An Historical Overview zond Analysis of Recent Char.oes by John S. Holtzwan WORKING PAPER No. 5 May 1987. Working Paper Series MAIZE SUPPLY AND PRICE SITUATION IN SOMALIA: AN HISTOR:CAL OVERVIEW A,'D ANALYSIS OF RECEMT CHANGF.51 John S. Holtzman Food Security Project, MOA/MSU 1.0 Introduction Maize is a basic staple in southern Somalia, whose output has expanded luring the past decada. The available official statistics suigest tiat Somali producers have cultivated more land to maizu U'uring the 1980s than during the 1970s. Aggregate moize production has expanded, while sorghum production has stagnated. Maize yields appear to have risen more rapidly than sorghum yields. tuiorts have fluctuated considerably, depending on overall availability of food grains in particular years. What are the factori that have contributed to increased maize output in Somalia- How important have rainfall, market liberalization, and -'eal price trends been in the expansion of taize prouction Pnd stagnation of sorghum prodUction? The objectives of this paper are thrcefold. First, it will present and discuss the av.i lable data on the maize supply and rice situation in Somalia, with special focus on changes in the 1980s (section 2.0). Second, the paper kill examine factors contributing to maize expansion (section 3.0). Last, it will assess in a preliminary way the possibility and opportunity for continued expansion in maip output (section 4.0). 2.0 Mzize Supoly and Price Situation in the 11B0s 2.1 Inconsistent Data: The Food Security Analyst's Dilemma In Somalia, as in many African countries, thi available sources .-f cereali production and impprt data are not always consistent. -

Somalia Hunger Crisis Response.Indd
WORLD VISION SOMALIA HUNGER RESPONSE SITUATION REPORT 5 March 2017 RESPONSE HIGHLIGHTS 17,784 people received primary health care 66,256 people provided with KEY MESSAGES 24,150,700 litres of safe drinking water • Drought has led to increased displacement education. In Somaliland more than 118 of people in Somalia. In February 2017 schools were closed as a result of the alone, UNHCR estimates that up to looming famine. 121,000 people were displaced. • Urgent action at this stage has a high • There is a sharp increase in the number of chance of saving over 300,000 children Acute Water Diarrhoea (AWD/cholera) who are acutely malnourished as well cases. From January to March, 875 AWD as over 6 million people facing possible cases and 78 deaths were recorded in starvation across the country. 22,644 Puntland, Somaliland and Jubaland. • Despite encouraging donor contributions, • There is an urgent need to scale up the Somalia humanitarian operational people provided with support for health interventions in the plan is less than 20% funded (UNOCHA, South West State (SWS) especially FTS, 7th March 2017). Approximately 5,917 in districts that have been hard hit by US$825 million is required to reach 5.5 NFI kits outbreaks of Acute Watery Diarrhoea million Somalis facing possible famine until (AWD). Only few agencies have funding June 2017. to support access to health care services. • More than 6 million people or over 50% • According to Somaliland MOH, high of Somalia’s population remain in crisis cases of measles, diarrhea and pneumonia and face possible famine if aid does not have been reported since November as match the scale of need between now main health complications caused by the and June 2017. -

Minutes for Regional Wash Cluster Meeting
Somalia WASH (Water, Sanitation, Hygiene) CLUSTER MINUTES FOR REGIONAL WASH CLUSTER MEETING Soma AGENDA Date: 19/05/2016 Time: 10:00: am-12:00pm Venue: Ministry of Health Chair: Abdullahinur Kassim Kindly confirm attendance for security access to: Sadia Hussein ([email protected]) and cc: [email protected] Standing items (for every meeting) 1. Introductions (5 min) 2. Review and endorsement of the last cluster meeting minutes and follow up on the action points (10 min) (give updates on the previous action points. NB: all updates should be captured in the meeting minutes) 3. Updates on AWD/cholera and ongoing response in the region 4. Updates on floods in the region and its impact in the affected areas and humanitarian response so far. 5. Ongoing/Planned response by partners (who is doing what, where and when- 4W matrix). 6. WASH gaps and current response. Can they be filled by agencies present in meeting with existing funds? 7. Elections of the District Lead Agencies (DLAs)/ District Focal Points (DFPs)MoHBanadir WASH Coordinator presentation on Regional WASH coordination. 8. Any other challenge or constraint affecting all agencies? Agree action 9. A.O.B File Name: Draft Agenda Banadir/Lower Shabelle meeting, 19th May, 2016 Somalia REGIONAL WASH CLUSTER MINUTES OF THE MEETING – BANADIR AND L/SHABELLE Date: 19/05/2016 Time: 10.00 am-12:00pm Venue: Ministry of Health Chair: AbdullahinurKassim Agenda Summary of discussion Action point Focal Time line point/Agency Introduction The meeting was chaired by Kassim, the WASH cluster regional focal point. It was opened with prayers. The chairman, welcomed the partners and gave them chance of introduction in general. -

Food Market and Supply Situation in Southern Somalia
Food Market and Supply Situation in Southern Somalia October 2011 Issa Sanogo 2 Acknowledgement This report is drawn from the findings of a programme mission by Annalisa Conte, Issa Sanogo and Simon Clements from August 30th to September 20th, which was undertaken to assess the suitability of cash-and-voucher based responses in southern Somalia. I wish to acknowledge valuable contributions made by various WFP Headquarters and country office colleagues, namely Rogerio Bonifacio, Oscar Caccavale, Simon Clements, Migena Cumani, Maliki Amadou Mahamane, Nichola Peach, and Francesco Slaviero. Many thanks also to Joyce Luma, Arif Husain and Mario Musa for proof reading the report. Many thanks to the Senior Management of WFP Somalia Country Office, Logistic, Procurement, Programme, Security and VAM staff who provided valuable insights and helped at various stages of this mission. I wish also to thank various partners (INGOs, Local NGOs, UN Organizations, Bilateral and Multilateral Organizations and Technical Partners) and traders for making time available to provide the mission with valuable field updates and perspectives. Secondary data, comments and suggestions provided by FAO, FSNAU and FEWSNET are fully acknowledged. While I acknowledge the contributions made by all the partners in various ways, I take full responsibility for the outcome. 3 I. Summary of Findings ............................................................................................................ 5 II. Markets and Supply Conditions ............................................................................................ -

Exploring the Old Stone Town of Mogadishu
Exploring the Old Stone Town of Mogadishu Exploring the Old Stone Town of Mogadishu By Nuredin Hagi Scikei Exploring the Old Stone Town of Mogadishu By Nuredin Hagi Scikei This book first published 2017 Cambridge Scholars Publishing Lady Stephenson Library, Newcastle upon Tyne, NE6 2PA, UK British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library Copyright © 2017 by Nuredin Hagi Scikei All rights for this book reserved. No part of this book may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the copyright owner. ISBN (10): 1-5275-0331-3 ISBN (13): 978-1-5275-0331-1 Dedicated to my father Hagi Scikei Abati, my mother Khadija Ali Omar, my sister Zuhra and my brother Sirajadin. CONTENTS Preface ........................................................................................................ xi Acknowledgements .................................................................................. xiii Chapter One ................................................................................................. 1 Introduction Who are the Banaadiri Maritime Traders and Ancient Banaadiri Settlements Religion and Learning The Growth of Foreign Trade, Urbanisation and the First Industries of Banaadir Chapter Two .............................................................................................. 11 The Campaign of Defamation against the Banaadiri -

(I) the SOCIAL STRUCTUBE of Soumn SOMALI TRIB by Virginia I?
(i) THE SOCIAL STRUCTUBE OF SOumN SOMALI TRIB by Virginia I?lling A thesis submitted for the Degree of Doctor of Philosophy at the University of London. October 197]. (ii) SDMMARY The subject is the social structure of a southern Somali community of about six thousand people, the Geledi, in the pre-colonial period; and. the manner in which it has reacted to colonial and other modern influences. Part A deals with the pre-colonial situation. Section 1 deals with the historical background up to the nineteenth century, first giving the general geographic and ethnographic setting, to show what elements went to the making of this community, and then giving the Geledj's own account of their history and movement up to that time. Section 2 deals with the structure of the society during the nineteenth century. Successive chapters deal with the basic units and categories into which this community divided both itself and the others with which it was in contact; with their material culture; with economic life; with slavery, which is shown to have been at the foundation of the social order; with the political and legal structure; and with the conduct of war. The chapter on the examines the politico-religious office of the Sheikh or Sultan as the focal point of the community, and how under successive occupants of this position, the Geledi became the dominant power in this part of Somalia. Part B deals with colonial and post-colonial influences. After an outline of the history of Somalia since 1889, with special reference to Geledi, the changes in society brought about by those events are (iii) described. -

Trees of Somalia
Trees of Somalia A Field Guide for Development Workers Desmond Mahony Oxfam Research Paper 3 Oxfam (UK and Ireland) © Oxfam (UK and Ireland) 1990 First published 1990 Revised 1991 Reprinted 1994 A catalogue record for this publication is available from the British Library ISBN 0 85598 109 1 Published by Oxfam (UK and Ireland), 274 Banbury Road, Oxford 0X2 7DZ, UK, in conjunction with the Henry Doubleday Research Association, Ryton-on-Dunsmore, Coventry CV8 3LG, UK Typeset by DTP Solutions, Bullingdon Road, Oxford Printed on environment-friendly paper by Oxfam Print Unit This book converted to digital file in 2010 Contents Acknowledgements IV Introduction Chapter 1. Names, Climatic zones and uses 3 Chapter 2. Tree descriptions 11 Chapter 3. References 189 Chapter 4. Appendix 191 Tables Table 1. Botanical tree names 3 Table 2. Somali tree names 4 Table 3. Somali tree names with regional v< 5 Table 4. Climatic zones 7 Table 5. Trees in order of drought tolerance 8 Table 6. Tree uses 9 Figures Figure 1. Climatic zones (based on altitude a Figure 2. Somali road and settlement map Vll IV Acknowledgements The author would like to acknowledge the assistance provided by the following organisations and individuals: Oxfam UK for funding me to compile these notes; the Henry Doubleday Research Association (UK) for funding the publication costs; the UK ODA forestry personnel for their encouragement and advice; Peter Kuchar and Richard Holt of NRA CRDP of Somalia for encouragement and essential information; Dr Wickens and staff of SEPESAL at Kew Gardens for information, advice and assistance; staff at Kew Herbarium, especially Gwilym Lewis, for practical advice on drawing, and Jan Gillet for his knowledge of Kew*s Botanical Collections and Somalian flora. -

Somali Republic Ministry of Education, Culture & Higher
National Education Plan Somali Republic Ministry of Education, Culture & Higher Education National Education Plan. May 2011 1 National Education Plan Preface The collapse of central government of Somalia in 1991 and the civil war that erupted and the continues foreign intervention has caused total destruction of national institution especially those who were providing services to our citizen like health, education, water ad electricity institutions. The destruction has affected the economics of the country both Public and private properties. The country has became a place where there is no law and order and insecurity prevailed and killing, looting and displacement has become day to day with the live of Somalis. The ministry of education, culture and higher education and its department was among the sectors that were spared that resulted total closure of all offices and centers that was dealing with education services and most of education staffs left the country as refugees. It was early 1992, when Somali educationalists regrouped again to revive the education sector of the country to provide the education service that our people used to get from the national education institution that was not functioning at all. Education umbrellas, privately owned school, colleges and higher education institutions have been established to cover the services that the ministry of education was providing to the people before 1991. But again this effort could not provide quality free education throughout the country. The role of the international and local organization towards the education sector of Somalia together with the support of citizens has made the sector with little improved. -
Immigration and Refugee Board of Canada Home > Research Program > Responses to Information Requests Responses to Information Requests
Responses to Information Requests - Immigration and Refugee Board of C... http://www.irb-cisr.gc.ca/Eng/ResRec/RirRdi/Pages/index.aspx?doc=45... Immigration and Refugee Board of Canada Home > Research Program > Responses to Information Requests Responses to Information Requests Responses to Information Requests (RIR) respond to focused Requests for Information that are submitted to the Research Directorate in the course of the refugee protection determination process. The database contains a seven-year archive of English and French RIRs. Earlier RIRs may be found on the UNHCR's Refworld website. 3 December 2012 SOM104240.E Somalia: The Bravanese (Barawan) ethnic group, including the location of their traditional homeland, affiliated clans and risks they face from other clans Research Directorate, Immigration and Refugee Board of Canada, Ottawa 1. Overview The Bravanese people [also known as Barawan, Barawani, Baravani, Reer Brava, Reer Baraawe] are an ethnic minority group in Somalia (UK 17 Jan. 2012, para. 19.21; ACCORD Dec. 2009, 17). They originate from the coastal city of Brava [also known as Barawe or Baraawe] and speak Chimiini [also known as Chimwini, Chimbalazi, Af Baraawe] (Academic 15 Nov. 2012; MRG Oct. 2010, 11), a dialect of Swahili (ibid., 16; Norway 22 July 2011, 11). According to Minority Rights Group International (MRG), the Bravanese also speak a local Tunni subclan dialect, Af-Maymay (Oct. 2010, 11). In correspondence with the Research Directorate, a UK based academic of Bravanese origin who has researched and published on the Bravanese explained that Bravanese people are called Waantu Wa Miini in Chimiini and are also known as Wa Mbalazi in Bravanese religious poetry (15 Nov. -
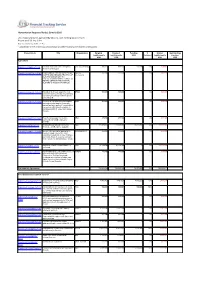
With Funding Status of Each Report As
Humanitarian Response Plan(s): Somalia 2016 List of appeal projects (grouped by Cluster), with funding status of each Report as of 23-Sep-2021 http://fts.unocha.org (Table ref: R3) Compiled by OCHA on the basis of information provided by donors and recipient organizations. Project Code Title Organization Original Revised Funding % Unmet Outstanding requirements requirements USD Covered requirements pledges USD USD USD USD Agriculture SOM-16/A/84942/5110 Puntland and Lower Juba Emergency VSF (Switzerland) 998,222 998,222 588,380 59% 409,842 0 Animal Health Support SOM-16/A/86501/15092 PROVISION OF FISHING INPUTS FOR SAFUK- 352,409 352,409 0 0% 352,409 0 YOUTHS AND MEN AND TRAINING OF International MEN AND WOMEN ON FISH PRODUCTION AND MAINTENANCE OF FISHING GEARS IN THE COASTAL REGIONS OF MUDUG IN SOMALIA. SOM-16/A/86701/14592 Integrated livelihoods support to most BRDO 500,000 500,000 0 0% 500,000 0 vulnerable conflict affected 2850 farming and fishing households in Marka district Lower Shabelle. SOM-16/A/86746/14852 Provision of essential livelihood support HOD 500,000 500,000 0 0% 500,000 0 and resilience building for Vulnerable pastoral and agro pastoral households in emergency, crisis and stress phase in Kismaayo district of Lower Juba region, Somalia SOM-16/A/86775/17412 Food Security support for destitute NRO 499,900 499,900 0 0% 499,900 0 communities in Middle and Lower Shabelle SOM-16/A/87833/123 Building Household and Community FAO 111,805,090 111,805,090 15,981,708 14% 95,823,382 0 Resilience and Response Capacity SOM-16/A/88141/17597 Access to live-saving for population in SHARDO Relief 494,554 494,554 0 0% 494,554 0 emergency and crises of the most vulnerable households in lower Shabelle and middle Shabelle regions, and build their resilience to withstand future shocks. -

A Moder N H O F Soma
COLLO... :,<.,r;: cc r i -J I.- .. P*!,!, REVISED, UPDATED, AND EXPANDED EDITION lì. A MODERN HISTORY OF SOMALIA Natlon and State in thè Horn of Africa I. M. LEWIS, Westview Press ^'5?x BOULDER & LONDON >^'*. \ K:%: jv^i -/ / o/ • /.-Ay v>; CONTENTS Preface to che 1988 Editìon vii Preface to thè First Edition ix Chapter I The Physica! and Social Setting 1 II Ecfore Partition 18 This Westview softcover editìon il printed un aud-frue pnper and bound in softcovecs thac III The Imperiai Partition: 1860-97 40 curry thè bighe» rating of thè National Aurxìation of State Textbook Adminìstracors, in tons» Iration wich thè Association of American Publiihcrs and thè Hook Manu faci uters' IV The Dervish Fight for Freedom: 1900-20 63 Inscitutf. V Somali Unificatìon: The Italian East*Afrìcan Empire Ali rights reserved. No pare of chis publkarion may be reproduced oc transmitted in any 92 forni or by any means, electronic or mechanical, including photocopy, rccording, or any in for m uri un Storage and retrieva! System, wichout pcrmìssion in wticing from thè publisher. VI The Restoration of Colonial Frontiere: 1940-50 116 Copyright © 1965, 1980, 1988 by I. M. Lewis VII From Trusteeship to Independence: 1950-60 139 Vili The Problems of Independence Fine published in thè United States of America in 1988 by Wesrvicw Press, Inc.; Frederick 166 Prjegcr, Publisher, 5500 Cenerai Avenue, Boulder, Colorado 80301 A. IX The Somali Revolution: 1969-76 205 First edìtion published in 1980 by Longman Group Limited; chapters 1 through 8 published X Nationalism, Ethnicity and Revolution in thè in 1965 by Weidenfeld ;»nd Nkolson Horn of Africa 226 Maps Library of Congress CaraJoging-in-PublicatÌon Data 267 Lewis, I. -
Transition Initiatives for Stabilization Plus (Tis+) Program Year Three – Annual Work Plan
TRANSITION INITIATIVES FOR STABILIZATION PLUS (TIS+) PROGRAM YEAR THREE – ANNUAL WORK PLAN (OCTOBER 1, 2017 – SEPTEMBER 30, 2018) Revised November 2017 This publication was produced for review by the United States Agency for International Development. It was prepared by AECOM. Annual Work plan | Transition Initiatives for Stabilization Plus (TIS+) Program i TRANSITION INITIATIVES FOR STABILIZATION PLUS (TIS+) PROGRAM YEAR THREE – ANNUAL WORK PLAN (OCTOBER 1, 2017 – SEPTEMBER 30, 2018) Contract No: AID-623-C-15-00001 Submitted to: USAID | Somalia Prepared by: AECOM International Development DISCLAIMER: The authors’ views expressed in this document do not necessarily reflect the views of the United States Agency for International Development or the United States Government. Year Three - Annual Work Plan | Transition Initiatives for Stabilization Plus (TIS+) Program i TABLE OF CONTENTS Table of Contents ........................................................................................................................................ ii Acronym List .............................................................................................................................................. iii Stabilization Context .................................................................................................................................. 5 Goals and Objectives of USAID and TIS+ ............................................................................................... 6 Methodology ........................................................................................................................................