World Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Coexistence of Antibodies to Tick-Borne
Mem Inst Oswaldo Cruz, Rio de Janeiro, Vol. 98(3): 311-318, April 2003 311 Coexistence of Antibodies to Tick-borne Agents of Babesiosis and Lyme Borreliosis in Patients from Cotia County, State of São Paulo, Brazil Natalino Hajime Yoshinari/+, Milena Garcia Abrão, Virginia Lúcia Nazário Bonoldi, Cleber Oliveira Soares*, Claudio Roberto Madruga*, Alessandra Scofield**, Carlos Luis Massard**, Adivaldo Henrique da Fonseca** Laboratório de Investigação em Reumatologia (LIM-17), Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo, Av. Dr. Arnaldo 455, 3º andar, 01246-903 São Paulo, SP, Brasil *Embrapa Gado de Corte, Campo Grande, MS, Brasil **Universidade Federal Rural do Rio de Janeiro, Seropédica, RJ, Brasil This paper reports a case of coinfection caused by pathogens of Lyme disease and babesiosis in brothers. This was the first case of borreliosis in Brazil, acquired in Cotia County, State of São Paulo, Brazil. Both children had tick bite history, presented erythema migrans, fever, arthralgia, mialgia, and developed positive serology (ELISA and Western-blotting) directed to Borrelia burgdorferi G 39/40 and Babesia bovis antigens, mainly of IgM class antibodies, suggestive of acute disease. Also, high frequencies of antibodies to B. bovis was observed in a group of 59 Brazilian patients with Lyme borreliosis (25.4%), when compared with that obtained in a normal control group (10.2%) (chi-square = 5.6; p < 0.05). Interestingly, both children presented the highest titers for IgM antibodies directed to both infective diseases, among all patients with Lyme borreliosis. Key words: lyme borreliosis - lyme disease - spirochetosis - borreliosis - babesiosis - coinfection - tick-borne disease - Brazil Babesiosis is a tick-borne disease distributed world- The first case of babesiosis in a healthy person, with wide, caused by hemoprotozoans of the genus Babesia, intact spleen, was reported in 1969 in a woman from Nan- which infects wild and domestic animals, promoting eco- tucket Island (Massachusetts, USA)(Wester et al. -

Hookworm (Ancylostomiasis)
Hookworm (ancylostomiasis) Hookworm (ancylostomiasis) rev Jan 2018 BASIC EPIDEMIOLOGY Infectious Agent Hookworm is a soil transmitted helminth. Human infections are caused by the nematode parasites Necator americanus and Ancylostoma duodenale. Transmission Transmission primarily occurs via direct contact with fecal contaminated soil. Soil becomes contaminated with eggs shed in the feces of an individual infected with hookworm. The eggs must incubate in the soil for several days before they become infectious and are able to be transmitted to another person. Oral transmission can sometimes occur from consuming improperly washed food grown or exposed to fecal contaminated soil. Transmission can also occur (rarely) between a mother and her fetus/infant via infected placental or mammary tissue. Incubation Period Eggs must incubate in the soil for 5-10 days before they mature into infectious filariform larvae that can penetrate the skin. Within the first 10 days following penetration of the skin filariform larvae will migrate to the lungs and occasionally cause respiratory symptoms. Three to five weeks after skin penetration the larvae will migrate to the intestinal tract where they will mature into an adult worm. Adult worms may live in the intestine for 1-5 years depending on the species. Communicability Human to human transmission of hookworm does NOT occur because part of the worm’s life cycle must be completed in soil before becoming infectious. However, vertical transmission of dormant filariform larvae can occur between a mother and neonate via contaminated breast milk. These dormant filariform larvae can remain within in a host for months to years. Soil contamination is perpetuated by fecal contamination from infected individuals who can shed eggs in feces for several years after infection. -

Bacterial Infections Diseases Picture Cause Basic Lesion
page: 117 Chapter 6: alphabetical Bacterial infections diseases picture cause basic lesion search contents print last screen viewed back next Bacterial infections diseases Impetigo page: 118 6.1 Impetigo alphabetical Bullous impetigo Bullae with cloudy contents, often surrounded by an erythematous halo. These bullae rupture easily picture and are rapidly replaced by extensive crusty patches. Bullous impetigo is classically caused by Staphylococcus aureus. cause basic lesion Basic Lesions: Bullae; Crusts Causes: Infection search contents print last screen viewed back next Bacterial infections diseases Impetigo page: 119 alphabetical Non-bullous impetigo Erythematous patches covered by a yellowish crust. Lesions are most frequently around the mouth. picture Lesions around the nose are very characteristic and require prolonged treatment. ß-Haemolytic streptococcus is cause most frequently found in this type of impetigo. basic lesion Basic Lesions: Erythematous Macule; Crusts Causes: Infection search contents print last screen viewed back next Bacterial infections diseases Ecthyma page: 120 6.2 Ecthyma alphabetical Slow and gradually deepening ulceration surmounted by a thick crust. The usual site of ecthyma are the legs. After healing there is a permanent scar. The pathogen is picture often a streptococcus. Ecthyma is very common in tropical countries. cause basic lesion Basic Lesions: Crusts; Ulcers Causes: Infection search contents print last screen viewed back next Bacterial infections diseases Folliculitis page: 121 6.3 Folliculitis -

Eisai Announces Results and Continued Support Of
No.17-18 April 19, 2017 Eisai Co., Ltd. EISAI ANNOUNCES RESULTS AND CONTINUED SUPPORT OF INITIATIVES FOR ELIMINATION OF LYMPHATIC FILARIASIS 5 YEAR ANNIVERSARY OF LONDON DECLARATION ON NEGLECTED TROPICAL DISEASES Eisai Co., Ltd. (Headquarters: Tokyo, CEO: Haruo Naito, “Eisai”) has announced the results of its initiatives for the elimination of lymphatic filariasis (LF), and its continued support of this cause in the future. This announcement was made at an event held in Geneva, Switzerland, on April 18, marking the 5th anniversary of the London Declaration on Neglected Tropical Diseases (NTDs), an international public-private partnership. Announced in January 2012, the London Declaration is the largest public-private partnership in the field of global health, and represents a coordinated effort by global pharmaceutical companies, the Bill & Melinda Gates Foundation, the World Health Organization (WHO), the United States, United Kingdom and NTD-endemic country governments, as well as other partners, to eliminate 10 NTDs by the year 2020. Since the signing of the London Declaration, donations of medical treatments by pharmaceutical companies have increased by 70 percent, and these treatments contribute to the prevention and cure of disease in approximately 1 billion people every year. Under the London Declaration, Eisai signed an agreement with WHO to supply 2.2 billion high-quality diethylcarbamazine (DEC) tablets, which were running in short supply worldwide, at Price Zero (free of charge) by the year 2020. These DEC tablets are manufactured at Eisai’s Vizag Plant in India. As of the end of March 2017, 1 billion tablets have been supplied to 27 endemic countries. -

Pathophysiology and Gastrointestinal Impacts of Parasitic Helminths in Human Being
Research and Reviews on Healthcare: Open Access Journal DOI: 10.32474/RRHOAJ.2020.06.000226 ISSN: 2637-6679 Research Article Pathophysiology and Gastrointestinal Impacts of Parasitic Helminths in Human Being Firew Admasu Hailu1*, Geremew Tafesse1 and Tsion Admasu Hailu2 1Dilla University, College of Natural and Computational Sciences, Department of Biology, Dilla, Ethiopia 2Addis Ababa Medical and Business College, Addis Ababa, Ethiopia *Corresponding author: Firew Admasu Hailu, Dilla University, College of Natural and Computational Sciences, Department of Biology, Dilla, Ethiopia Received: November 05, 2020 Published: November 20, 2020 Abstract Introduction: This study mainly focus on the major pathologic manifestations of human gastrointestinal impacts of parasitic worms. Background: Helminthes and protozoan are human parasites that can infect gastrointestinal tract of humans beings and reside in intestinal wall. Protozoans are one celled microscopic, able to multiply in humans, contributes to their survival, permits serious infections, use one of the four main modes of transmission (direct, fecal-oral, vector-borne, and predator-prey) and also helminthes are necked multicellular organisms, referred as intestinal worms even though not all helminthes reside in intestines. However, in their adult form, helminthes cannot multiply in humans and able to survive in mammalian host for many years due to their ability to manipulate immune response. Objectives: The objectives of this study is to assess the main pathophysiology and gastrointestinal impacts of parasitic worms in human being. Methods: Both primary and secondary data were collected using direct observation, books and articles, and also analyzed quantitativelyResults and and conclusion: qualitatively Parasites following are standard organisms scientific living temporarily methods. in or on other organisms called host like human and other animals. -
From Confusion to Coma: a Catastrophic Deterioration
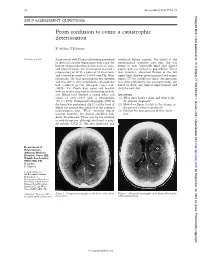
52 Postgrad Med J 2001;77:52–55 Postgrad Med J: first published as 10.1136/pmj.77.903.53a on 1 January 2001. Downloaded from SELF ASSESSMENT QUESTIONS From confusion to coma: a catastrophic deterioration K Ashkan, F Johnston Answers on p 56. A previously well 45 year old woman presented ventilated before transfer. On arrival at the to the local casualty department with a one day neurosurgical intensive care unit, she was history of generalised headache, neck stiVness, found to have bilaterally fixed and dilated and blurred vision. On examination she had a pupils, with no corneal or gag reflexes. There temperature of 38°C, a pulse of 80 beats/min, was, however, abnormal flexion of the left and a blood pressure of 130/80 mm Hg. Neu- upper limb. She was given mannitol and urgent rologically, she had spontaneous eye opening repeat CT was carried out (fig 2). An operation and was able to obey commands, although she was then performed, but postoperatively she had confused speech (Glasgow coma scale failed to show any clinical improvement and (GCS), 14). Pupils were equal and reactive died the next day. with no cranial or peripheral neurological defi- cits. Blood tests showed a raised white cell Questions count of 20.9 × 109/l with a neutrophilia (1) What does figure 1 show and what is the (19.2 × 109/l). Computed tomography (CT) of diVerential diagnosis? the brain was performed (fig 1), on the basis of (2) How does figure 2 relate to the change in which the patient was referred to the regional the patient’s clinical condition? neurosurgical unit. -
Hypervitaminosis - an Emerging Pathological Condition
International Journal of Health Sciences and Research www.ijhsr.org ISSN: 2249-9571 Review Article Hypervitaminosis - An Emerging Pathological Condition J K Roop PG Department of Zoology, JC DAV College (Affiliated to Panjab University, Chandigarh), Dasuya-144205, District Hoshiarpur, Punjab, India ABSTRACT Vitamins are essential organic compounds that are required in small amounts to regulate various metabolic activities in the body. Prolonged and overconsumption of pharmaceutical forms of both water-soluble and fat-soluble vitamins may lead to toxicity and/or hypervitaminosis. Hypervitaminosis is an acute emerging pathological condition of the body due to excess accumulation of any of the vitamins. In case of acute poisoning with vitamin supplements/drugs, emergency assistance is required to detoxify the effects and restore the organization, structure and function of body’s tissues and organs. Sometimes death may occur due to intoxication to liver, kidney and heart. So, to manage any type of hypervitaminosis, proper diagnosis is essential to initiate eliminating the cause of its occurrence and accelerate the elimination of the supplement from the body. The present review discusses the symptoms of hypervitaminosis that seems to be a matter of concern today and management strategies to overcome toxicity or hypervitaminosis. Keywords: Hypervitaminosis, Toxicity, Vitamins, Vitamin pathology, Fat-soluble vitamin, Water- soluble vitamin. INTRODUCTION body, particularly in the liver. Vitamin B Vitamins are potent organic Complex and vitamin C are water- soluble. compounds present in small concentrations They are dissolved easily in food during in various fruits and vegetables. They cooking and a portion of these vitamins may regulate physiological functions and help in be destroyed by heating. -

Hookworm-Related Cutaneous Larva Migrans
326 Hookworm-Related Cutaneous Larva Migrans Patrick Hochedez , MD , and Eric Caumes , MD Département des Maladies Infectieuses et Tropicales, Hôpital Pitié-Salpêtrière, Paris, France DOI: 10.1111/j.1708-8305.2007.00148.x Downloaded from https://academic.oup.com/jtm/article/14/5/326/1808671 by guest on 27 September 2021 utaneous larva migrans (CLM) is the most fre- Risk factors for developing HrCLM have specifi - Cquent travel-associated skin disease of tropical cally been investigated in one outbreak in Canadian origin. 1,2 This dermatosis fi rst described as CLM by tourists: less frequent use of protective footwear Lee in 1874 was later attributed to the subcutane- while walking on the beach was signifi cantly associ- ous migration of Ancylostoma larvae by White and ated with a higher risk of developing the disease, Dove in 1929. 3,4 Since then, this skin disease has also with a risk ratio of 4. Moreover, affected patients been called creeping eruption, creeping verminous were somewhat younger than unaffected travelers dermatitis, sand worm eruption, or plumber ’ s itch, (36.9 vs 41.2 yr, p = 0.014). There was no correla- which adds to the confusion. It has been suggested tion between the reported amount of time spent on to name this disease hookworm-related cutaneous the beach and the risk of developing CLM. Consid- larva migrans (HrCLM).5 ering animals in the neighborhood, 90% of the Although frequent, this tropical dermatosis is travelers in that study reported seeing cats on the not suffi ciently well known by Western physicians, beach and around the hotel area, and only 1.5% and this can delay diagnosis and effective treatment. -

Albendazole: a Review of Anthelmintic Efficacy and Safety in Humans
S113 Albendazole: a review of anthelmintic efficacy and safety in humans J.HORTON* Therapeutics (Tropical Medicine), SmithKline Beecham International, Brentford, Middlesex, United Kingdom TW8 9BD This comprehensive review briefly describes the history and pharmacology of albendazole as an anthelminthic drug and presents detailed summaries of the efficacy and safety of albendazole’s use as an anthelminthic in humans. Cure rates and % egg reduction rates are presented from studies published through March 1998 both for the recommended single dose of 400 mg for hookworm (separately for Necator americanus and Ancylostoma duodenale when possible), Ascaris lumbricoides, Trichuris trichiura, and Enterobius vermicularis and, in separate tables, for doses other than a single dose of 400 mg. Overall cure rates are also presented separately for studies involving only children 2–15 years. Similar tables are also provided for the recommended dose of 400 mg per day for 3 days in Strongyloides stercoralis, Taenia spp. and Hymenolepis nana infections and separately for other dose regimens. The remarkable safety record involving more than several hundred million patient exposures over a 20 year period is also documented, both with data on adverse experiences occurring in clinical trials and with those in the published literature and\or spontaneously reported to the company. The incidence of side effects reported in the published literature is very low, with only gastrointestinal side effects occurring with an overall frequency of just "1%. Albendazole’s unique broad-spectrum activity is exemplified in the overall cure rates calculated from studies employing the recommended doses for hookworm (78% in 68 studies: 92% for A. duodenale in 23 studies and 75% for N. -

Skin Disease and Disorders
Sports Dermatology Robert Kiningham, MD, FACSM Department of Family Medicine University of Michigan Health System Disclosures/Conflicts of Interest ◼ None Goals and Objectives ◼ Review skin infections common in athletes ◼ Establish a logical treatment approach to skin infections ◼ Discuss ways to decrease the risk of athlete’s acquiring and spreading skin infections ◼ Discuss disqualification and return-to-play criteria for athletes with skin infections ◼ Recognize and treat non-infectious skin conditions in athletes Skin Infections in Athletes ◼ Bacterial ◼ Herpetic ◼ Fungal Skin Infections in Athletes ◼ Very common – most common cause of practice-loss time in wrestlers ◼ Athletes are susceptible because: – Prone to skin breakdown (abrasions, cuts) – Warm, moist environment – Close contacts Cases 1 -3 ◼ 21 year old male football player with 4 day h/o left axillary pain and tenderness. Two days ago he noticed a tender “bump” that is getting bigger and more tender. ◼ 16 year old football player with 3 day h/o mildly tender lesions on chin. Started as a single lesion, but now has “spread”. Over the past day the lesions have developed a dark yellowish crust. ◼ 19 year old wrestler with a 3 day h/o lesions on right side of face. Noticed “tingling” 4 days ago, small fluid filled lesions then appeared that have now started to crust over. Skin Infections Bacterial Skin Infections ◼ Cellulitis ◼ Erysipelas ◼ Impetigo ◼ Furunculosis ◼ Folliculitis ◼ Paronychea Cellulitis Cellulitis ◼ Diffuse infection of connective tissue with severe inflammation of dermal and subcutaneous layers of the skin – Triad of erythema, edema, and warmth in the absence of underlying foci ◼ S. aureus or S. pyogenes Erysipelas Erysipelas ◼ Superficial infection of the dermis ◼ Distinguished from cellulitis by the intracutaneous edema that produces palpable margins of the skin. -

Question of the Day Archives: Monday, December 5, 2016 Question: Calcium Oxalate Is a Widespread Toxin Found in Many Species of Plants
Question Of the Day Archives: Monday, December 5, 2016 Question: Calcium oxalate is a widespread toxin found in many species of plants. What is the needle shaped crystal containing calcium oxalate called and what is the compilation of these structures known as? Answer: The needle shaped plant-based crystals containing calcium oxalate are known as raphides. A compilation of raphides forms the structure known as an idioblast. (Lim CS et al. Atlas of select poisonous plants and mushrooms. 2016 Disease-a-Month 62(3):37-66) Friday, December 2, 2016 Question: Which oral chelating agent has been reported to cause transient increases in plasma ALT activity in some patients as well as rare instances of mucocutaneous skin reactions? Answer: Orally administered dimercaptosuccinic acid (DMSA) has been reported to cause transient increases in ALT activity as well as rare instances of mucocutaneous skin reactions. (Bradberry S et al. Use of oral dimercaptosuccinic acid (succimer) in adult patients with inorganic lead poisoning. 2009 Q J Med 102:721-732) Thursday, December 1, 2016 Question: What is Clioquinol and why was it withdrawn from the market during the 1970s? Answer: According to the cited reference, “Between the 1950s and 1970s Clioquinol was used to treat and prevent intestinal parasitic disease [intestinal amebiasis].” “In the early 1970s Clioquinol was withdrawn from the market as an oral agent due to an association with sub-acute myelo-optic neuropathy (SMON) in Japanese patients. SMON is a syndrome that involves sensory and motor disturbances in the lower limbs as well as visual changes that are due to symmetrical demyelination of the lateral and posterior funiculi of the spinal cord, optic nerve, and peripheral nerves. -

Pediatric Cutaneous Bacterial Infections Dr
PEDIATRIC CUTANEOUS BACTERIAL INFECTIONS DR. PEARL C. KWONG MD PHD BOARD CERTIFIED PEDIATRIC DERMATOLOGIST JACKSONVILLE, FLORIDA DISCLOSURE • No relevant relationships PRETEST QUESTIONS • In Staph scalded skin syndrome: • A. The staph bacteria can be isolated from the nares , conjunctiva or the perianal area • B. The patients always have associated multiple system involvement including GI hepatic MSK renal and CNS • C. common in adults and adolescents • D. can also be caused by Pseudomonas aeruginosa • E. None of the above PRETEST QUESTIONS • Scarlet fever • A. should be treated with penicillins • B. should be treated with sulfa drugs • C. can lead to toxic shock syndrome • D. can be associated with pharyngitis or circumoral pallor • E. Both A and D are correct PRETEST QUESTIONS • Strep can be treated with the following antibiotics • A. Penicillin • B. First generation cephalosporin • C. clindamycin • D. Septra • E. A B or C • F. A and D only PRETEST QUESTIONS • MRSA • A. is only acquired via hospital • B. can be acquired in the community • C. is more aggressive than OSSA • D. needs treatment with first generation cephalosporin • E. A and C • F. B and C CUTANEOUS BACTERIAL PATHOGENS • Staphylococcus aureus: OSSA and MRSA • Gp A Streptococcus GABHS • Pseudomonas aeruginosa CUTANEOUS BACTERIAL INFECTIONS • Folliculitis • Non bullous Impetigo/Bullous Impetigo • Furuncle/Carbuncle/Abscess • Cellulitis • Acute Paronychia • Dactylitis • Erysipelas • Impetiginization of dermatoses BACTERIAL INFECTION • Important to diagnose early • Almost always