Pleural Effusions and Pneumothoraces
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pleural Effusion and Ventilation/Perfusion Scan Interpretation for Acute Pulmonary Embolus
ventricular function by radionuclide angiography during exercise in normal subjects 33. Verani MS. Myocardial perfusion imaging versus two-dimensional echocardiography: and patients with chronic coronary heart disease. J Am Coll Cardiol 1983;1:1518- comparative value in the diagnosis of coronary artery disease. J NucÃCardiol 1529. 1994;1:399-414. 29. Adam WE. Tarkowska A, Bitter F, Stauch M, Geffers H. Equilibrium (gated) 34. Foster T, McNeill AJ, Salustri A, et al. Simultaneous dobutamine stress echocardiog radionuclide ventriculography. Cardiovasc Radial 1979;2:161-173. raphy and technetium-99m SPECT in patients with suspected coronary artery disease. 30. Hurwitz RA, TrêvesS, Kuroc A. Right ventricular and left ventricular ejection fraction J Am Coll Cardiol I993;21:1591-I596. in pediatrie patients with normal hearts: first pass radionuclide angiography. Am 35. Marwick TH, D'Hondt AM, Mairesse GH, Baudhuin T, Wijins W, Detry JM, Meiin Heart J 1984;107:726-732. 31. Freeman ML, Palac R, Mason J, et al. A comparison of dobutamine infusion and JA. Comparative ability of dobutamine and exercise stress in inducing myocardial ischemia in active patients. Br Heart J 1994:72:31-38. supine bicycle exercise for radionuclide cardiac stress testing. Clin NucÃMed 1984:9:251-255. 36. Senior R, Sridhara BS, Anagnostou E, Handler C, Raftery EB, Lahiri A. Synergistic 32. Cohen JL, Greene TO, Ottenweller J, Binebaum SZ, Wilchfort SD, Kim CS. value of simultaneous stress dobutamine sestamibi single-photon-emission computer Dobutamine digital echocardiography for detecting coronary artery disease. Am J ized tomography and echocardiography in the detection of coronary artery disease. -

Lung Pathology: Embryologic Abnormalities
Chapter2C Lung Pathology: Embryologic Abnormalities Content and Objectives Pulmonary Sequestration 2C-3 Chest X-ray Findings in Arteriovenous Malformation of the Great Vein of Galen 2C-7 Situs Inversus Totalis 2C-10 Congenital Cystic Adenomatoid Malformation of the Lung 2C-14 VATER Association 2C-20 Extralobar Sequestration with Congenital Diaphragmatic Hernia: A Complicated Case Study 2C-24 Congenital Chylothorax: A Case Study 2C-37 Continuing Nursing Education Test CNE-1 Objectives: 1. Explain how the diagnosis of pulmonary sequestration is made. 2. Discuss the types of imaging studies used to diagnose AVM of the great vein of Galen. 3. Describe how imaging studies are used to treat AVM. 4. Explain how situs inversus totalis is diagnosed. 5. Discuss the differential diagnosis of congenital cystic adenomatoid malformation. (continued) Neonatal Radiology Basics Lung Pathology: Embryologic Abnormalities 2C-1 6. Describe the diagnosis work-up for VATER association. 7. Explain the three classifications of pulmonary sequestration. 8. Discuss the diagnostic procedures for congenital chylothorax. 2C-2 Lung Pathology: Embryologic Abnormalities Neonatal Radiology Basics Chapter2C Lung Pathology: Embryologic Abnormalities EDITOR Carol Trotter, PhD, RN, NNP-BC Pulmonary Sequestration pulmonary sequestrations is cited as the 1902 theory of Eppinger and Schauenstein.4 The two postulated an accessory he clinician frequently cares for infants who present foregut tracheobronchia budding distal to the normal buds, Twith respiratory distress and/or abnormal chest x-ray with caudal migration giving rise to the sequestered tissue. The findings of undetermined etiology. One of the essential com- type of sequestration, intralobar or extralobar, would depend ponents in the process of patient evaluation is consideration on the timing of the accessory foregut budding (Figure 2C-1). -
Edition 2 Trauma Basics
Welcome to the Trauma Alert Education Newsletter brought to you by Beacon Trauma Services. Edition 2 Trauma Basics Trauma resuscitation is the initial stabilization and early life saving interventions provided to the trauma patient. It doesn’t mean that CPR was performed. When assessing the trauma patient it is important to recognize clues that indicate what is wrong now and what could go wrong later. Investigating the mechanism of injury is one of the most important clues to evaluate. This can be done by listening carefully to the MIST report from EMS and utilizing the 60 second time out for EMS to give report Source: https://tinyurl.com/ycjssbr3 What is wrong with me? EMS MIST 43 year old male M= unrestrained driver, while texting drove off road at 40 mph into a tree, with impact to driver’s door, 20 minute extrication time I= Deformity to left femur, pain to left chest, skin pink and warm S= B/P- 110/72, HR- 128 normal sinus, RR- 28, Spo2- 94% GCS=14 (Eyes= 4 Verbal= 4 Motor= 6) T= rigid cervical collar, IV Normal Saline at controlled rate, splint left femur What are your concerns? (think about the mechanism and the EMS report), what would you prepare prior to the patient arriving? Ten minutes after arrival in the emergency department the patient starts to have shortness of breath with stridorous sound. He is now diaphoretic and pale. B/P- 80/40, HR- 140, RR- 36 labored. Absent breath sounds on the left. What is the patients’ underlying problem?- Answer later in the newsletter Excellence in Trauma Nursing Award Awarded in May for National Trauma Month This year the nominations were very close so we chose one overall winner and two honorable mentions. -

Boerhaave's Syndrome – Tension Hydropneumothorax and Rapidly
Boerhaave’s syndrome – tension hydropneumothorax and rapidly developing hydropneumothorax: two radiographic clues in one case Lam Nguyen Ho, Ngoc Tran Van & Thuong Vu Le Department of Internal Medicine, Faculty of Medicine, University of Medicine and Pharmacy, Ho Chi Minh City, Vietnam. Keywords Abstract Boerhaave’s syndrome, hydropneumothorax, methylene blue, pleural effusion, tension Boerhaave’s syndrome is a rare and severe condition with high mortality partly pneumothorax. because of its atypical presentation resulting in delayed diagnosis and management. Diagnostic clues play an important role in the approach to this syndrome. Here, we Correspondence report a 48 year-old male patient hospitalized with fever and left chest pain radiating Nguyen Ho Lam, Department of Internal into the interscapular area. Two chest radiographs undertaken 22 h apart showed a Medicine, Faculty of Medicine, University of rapidly developing tension hydropneumothorax. The amylase level in the pleural Medicine and Pharmacy, 217 Hong Bang fl fl Street, Ward 11, District 5, Ho Chi Minh City, uid was high. The uid in the chest tube turned bluish after the patient drank Vietnam. E-mail: [email protected] methylene blue. The diagnosis of Boerhaave’s syndrome was suspected based on the aforementioned clinical clues and confirmed at the operation. The patient Received: 17 January 2016; Revised: recovered completely with the use of antibiotics and surgical treatment. In this case, 25 February 2016; Accepted: 10 March 2016 we describe key findings on chest radiographs that are useful in diagnosing Boerhaave’s syndrome. Respirology Case Reports, 4(4),2016,e00160 doi: 10.1002/rcr2.160 Introduction severe left chest pain radiating into the interscapular area. -

Chest and Abdominal Radiograph 101
Chest and Abdominal Radiograph 101 Ketsia Pierre MD, MSCI July 16, 2010 Objectives • Chest radiograph – Approach to interpreting chest films – Lines/tubes – Pneumothorax/pneumomediastinum/pneumopericar dium – Pleural effusion – Pulmonary edema • Abdominal radiograph – Tubes – Bowel gas pattern • Ileus • Bowel obstruction – Pneumoperitoneum First things first • Turn off stray lights, optimize room lighting • Patient Data – Correct patient – Patient history – Look at old films • Routine Technique: AP/PA, exposure, rotation, supine or erect Approach to Reading a Chest Film • Identify tubes and lines • Airway: trachea midline or deviated, caliber change, bronchial cut off • Cardiac silhouette: Normal/enlarged • Mediastinum • Lungs: volumes, abnormal opacity or lucency • Pulmonary vessels • Hila: masses, lymphadenopathy • Pleura: effusion, thickening, calcification • Bones/soft tissues (four corners) Anatomy of a PA Chest Film TUBES Endotracheal Tubes Ideal location for ETT Is 5 +/‐ 2 cm from carina ‐Normal ETT excursion with flexion and extension of neck 2 cm. ETT at carina Right mainstem Intubation ‐Right mainstem intubation with left basilar atelectasis. ETT too high Other tubes to consider DHT down right mainstem DHT down left mainstem NGT with tip at GE junction CENTRAL LINES Central Venous Line Ideal location for tip of central venous line is within superior vena cava. ‐ Risk of thrombosis decreased in central veins. ‐ Catheter position within atrium increases risk of perforation Acceptable central line positions • Zone A –distal SVC/superior atriocaval junction. • Zone B – proximal SVC • Zone C –left brachiocephalic vein. Right subclavian central venous catheter directed cephalad into IJ Where is this tip? Hemiazygous Or this one? Right vertebral artery Pulmonary Arterial Catheter Ideal location for tip of PA catheter within mediastinal shadow. -

Pneumothorax Ex Vacuo in a Patient with Malignant Pleural Effusion After Pleurx Catheter Placement
The Medicine Forum Volume 16 Article 20 2015 Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 Thomas Jefferson University, [email protected] Loheetha Ragupathi, MD Thomas Jefferson University, [email protected] Follow this and additional works at: https://jdc.jefferson.edu/tmf Part of the Medicine and Health Sciences Commons Let us know how access to this document benefits ouy Recommended Citation Bhardwaj, MS4, Meera and Ragupathi, MD, Loheetha (2015) "Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement," The Medicine Forum: Vol. 16 , Article 20. DOI: https://doi.org/10.29046/TMF.016.1.019 Available at: https://jdc.jefferson.edu/tmf/vol16/iss1/20 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in The Medicine Forum by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Bhardwaj, MS4 and Ragupathi, MD: Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 and Loheetha Ragupathi, MD INTRODUCTION Pneumothorax ex vacuo (“without vaccuum”) is a type of pneumothorax that can develop in patients with large pleural effusions. -
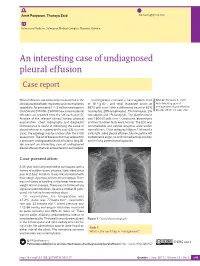
An Interesting Case of Undiagnosed Pleural Effusion Case Report
Amit Panjwani, Thuraya Zaid [email protected] Pulmonary Medicine, Salmaniya Medical Complex, Manama, Bahrain. An interesting case of undiagnosed pleural effusion Case report Pleural effusions are commonly encountered in the Investigations revealed a haemoglobin level Cite as: Panjwani A, Zaid T. clinical practise of both respiratory and nonrespiratory of 16.4 g⋅dL−1, and total leukocyte count of An interesting case of specialists. An estimated 1–1.5 million new cases in 8870 cells⋅mm−3 with a differential count of 62% undiagnosed pleural effusion. the USA and 200 000–250 000 new cases of pleural neutrophils, 28% lymphocytes, 7% monocytes, 2% Breathe 2017; 13: e46–e52. effusions are reported from the UK each year [1]. eosinophils and 1% basophils. The platelet count Analysis of the relevant clinical history, physical was 160 000 cells⋅mm−3. Creatinine, electrolytes examination, chest radiography and diagnostic and liver function tests were normal. The ECG was thoracentesis is useful in identifying the cause of unremarkable and cardiac enzymes were within pleural effusion in majority of the cases [2]. In a few normal limits. Chest radiograph (figure 1) showed a cases, the aetiology may be unclear after the initial mild, right-sided pleural effusion, blunting of the left assessment. The list of diseases that may account for costophrenic angle, no shift of mediastinal position a persistent undiagnosed pleural effusion is long [3]. and no lung parenchymal opacities. We present an interesting case of undiagnosed pleural effusion that was encountered in our hospital. R Case presentation A 33-year-old male presented to our hospital with a history of sudden-onset, pleuritic, right-sided chest pain of 2 days’ duration. -

Prenatal Diagnosis of Frequently Seen Fetal Syndromes (AZ)
Prenatal diagnosis of frequently seen fetal syndromes (A-Z) Ibrahim Bildirici,MD Professor of OBGYN ACIBADEM University SOM Attending Perinatologist ACIBADEM MASLAK Hospital Amniotic band sequence: Amniotic band sequence refers to a highly variable spectrum of congenital anomalies that occur in association with amniotic bands The estimated incidence of ABS ranges from 1:1200 to 1:15,000 in live births, and 1:70 in stillbirths Anomalies include: Craniofacial abnormalities — eg, encephalocele, exencephaly, clefts, which are often in unusual locations; anencephaly. Body wall defects (especially if not in the midline), abdominal or thoracic contents may herniate through a body wall defect and into the amniotic cavity. Limb defects — constriction rings, amputation, syndactyly, clubfoot, hand deformities, lymphedema distal to a constriction ring. Visceral defects — eg, lung hypoplasia. Other — Autotransplanted tissue on skin tags, spinal defects, scoliosis, ambiguous genitalia, short umbilical cord due to restricted motion of the fetus Arthrogryposis •Multiple congenital joint contractures/ankyloses involving two or more body areas •Pena Shokeir phenotype micrognathia, multiple contractures, camptodactyly (persistent finger flexion), polyhydramnios *many are AR *Lethal due to pulmonary hypoplasia • Distal arthrogryposis Subset of non-progressive contractures w/o associated primary neurologic or muscle disease Beckwith Wiedemannn Syndrome Macrosomia Hemihyperplasia Macroglossia Ventral wall defects Predisposition to embryonal tumors Neonatal hypoglycemia Variable developmental delay 85% sporadic with normal karyotype 10-15% autosomal dominant inheritance 10-20% with paternal uniparental disomy (Both copies of 11p15 derived from father) ***Imprinting related disorder 1/13 000. Binder Phenotype a flat profile and depressed nasal bridge. Short nose, short columella, flat naso-labial angle and perialar flattening Isolated Binder Phenotype transmission would be autosomal dominant Binder Phenotype can also be an important sign of chondrodysplasia punctata (CDDP) 1. -

Nonimmune Hydrops Foetalis: Value of Perinatal Autopsy and Placental Examination in Determining Aetiology
International Journal of Research in Medical Sciences Ramya T et al. Int J Res Med Sci. 2018 Oct;6(10):3327-3334 www.msjonline.org pISSN 2320-6071 | eISSN 2320-6012 DOI: http://dx.doi.org/10.18203/2320-6012.ijrms20184041 Original Research Article Nonimmune hydrops foetalis: value of perinatal autopsy and placental examination in determining aetiology Ramya T.1, Umamaheswari G2*, Chaitra V.2 1Department of Obstetrics and Gynaecology, 2Department of Pathology, PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India Received: 29 July 2018 Accepted: 29 August 2018 *Correspondence: Dr. Umamaheswari G., E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Background: Authors sought to determine the possible factors in the causation of nonimmune hydrops foetalis by perinatal autopsy with placental examination and to reduce the number of cases in which the cause remains elusive. Methods: Twenty five cases of nonimmune hydrops foetalis were identified in about 200 consecutive perinatal autopsies (including placental examination) performed during a 11 year period. The results were correlated with clinical, laboratory and imaging characteristics in an attempt to establish the aetiology. Results: Perinatal autopsy and placental examination confirmed the following aetiologies: cardiovascular causes (8) [isolated (4), syndromic (3) and associated chromosomal (1)], placental causes (5), chromosomal (4) [isolated(3) and associated cardiovascular disease (1)], intrathoracic (3), genitourinary causes (3), infections(1),gastrointestinal lesions (1) and idiopathic causes (1). -

Recurrent Non Immune Hydrops Fetalis: a Case Report
International Journal of Reproduction, Contraception, Obstetrics and Gynecology Nigam S et al. Int J Reprod Contracept Obstet Gynecol. 2016 May;5(5):1640-1642 www.ijrcog.org pISSN 2320-1770 | eISSN 2320-1789 DOI: http://dx.doi.org/10.18203/2320-1770.ijrcog20161341 Case Report Recurrent non immune hydrops fetalis: a case report Shipra Nigam*, Kundavi Shankar, Thankam Rana Varma Institute of Reproductive Medicine and Women’sTushar Health, Kanti Madras Das Medical Mission Hospital, A-4, Dr. J. Jayalalitha Nagar, Mogappair East, Chennai- 600037, Tamil Nadu, India Received: 23 February 2016 Revised: 23 March 2016 Accepted: 30 March 2016 *Correspondence: Dr. Shilpa Nigam, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Recurrent non-immune fetal hydrops (NIHF) is a known but rare disease. We report a case of recurrent fetal hydrops in a multipara with no significant surgical or medical history. She presented for a preconceptional counselling with a background history of having two previous pregnancies affected by hydrops. Both the affected pregnancies resulted in mid trimester pregnancy termination. Detailed evaluation of the couple was done in our hospital before planning the third pregnancy. No obvious cause of recurrent hydrops was found. She conceived spontaneously and finally delivered a healthy baby. This case highlights the fact that thorough investigation is essential in case of hydrops fetalis so that further pregnancies are not affected. -

Non-Immune Hydrops Fetalis Caused by Herpes Simplex Virus Type 2 in the Setting of Recurrent Maternal Infection
Journal of Perinatology (2013) 33, 817–820 & 2013 Nature America, Inc. All rights reserved 0743-8346/13 www.nature.com/jp PERINATAL/NEONATAL CASE PRESENTATION Non-immune hydrops fetalis caused by herpes simplex virus type 2 in the setting of recurrent maternal infection KM Pfister1, MR Schleiss2, RC Reed3 and TN George1 We report a case of non-immune hydrops fetalis (NIHF) caused by herpes simplex virus type 2 (HSV-2) in an infant whose mother had recurrent HSV-2 infection. In spite of prematurity, severe disseminated infection and hydrops, the infant survived and was neurologically intact. HSV-2-induced NIHF is extremely rare, particularly in the setting of recurrent maternal infection, and this case is, to our knowledge, the first report of a surviving infant. HSV-2 should be considered in the differential diagnosis of NIHF and early initiation of empiric acyclovir therapy is recommended in this setting, pending the results of virologic diagnostic tests. Journal of Perinatology (2013) 33, 817–820; doi:10.1038/jp.2013.68 Keywords: neonatal HSV infection; fetal hydrops; HSV-2 infection; placental infection; acyclovir; torch infection INTRODUCTION Following transfer to our neonatal intensive care unit from a Non-immune hydrops fetalis (NIHF), which occurs in 1 in 2500 to referring facility on day of life (DOL) 1, examination was remark- 4000 pregnancies, continues to have a very high perinatal mortality able for a severely hydropic-appearing premature infant with a rate, ranging from 50 to 90%.1,2 Cardiac disorders, genetic distended abdomen and an enlarged, firm liver. Skin examination abnormalities, fetal malformations, hematologic disorders and showed diffuse erythema, non-tense bullae on the chest and infections can all lead to NIHF. -

Allergic Bronchopulmonary Aspergillosis: a Perplexing Clinical Entity Ashok Shah,1* Chandramani Panjabi2
Review Allergy Asthma Immunol Res. 2016 July;8(4):282-297. http://dx.doi.org/10.4168/aair.2016.8.4.282 pISSN 2092-7355 • eISSN 2092-7363 Allergic Bronchopulmonary Aspergillosis: A Perplexing Clinical Entity Ashok Shah,1* Chandramani Panjabi2 1Department of Pulmonary Medicine, Vallabhbhai Patel Chest Institute, University of Delhi, Delhi, India 2Department of Respiratory Medicine, Mata Chanan Devi Hospital, New Delhi, India This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. In susceptible individuals, inhalation of Aspergillus spores can affect the respiratory tract in many ways. These spores get trapped in the viscid spu- tum of asthmatic subjects which triggers a cascade of inflammatory reactions that can result in Aspergillus-induced asthma, allergic bronchopulmo- nary aspergillosis (ABPA), and allergic Aspergillus sinusitis (AAS). An immunologically mediated disease, ABPA, occurs predominantly in patients with asthma and cystic fibrosis (CF). A set of criteria, which is still evolving, is required for diagnosis. Imaging plays a compelling role in the diagno- sis and monitoring of the disease. Demonstration of central bronchiectasis with normal tapering bronchi is still considered pathognomonic in pa- tients without CF. Elevated serum IgE levels and Aspergillus-specific IgE and/or IgG are also vital for the diagnosis. Mucoid impaction occurring in the paranasal sinuses results in AAS, which also requires a set of diagnostic criteria. Demonstration of fungal elements in sinus material is the hall- mark of AAS.