Pediatric Neurology: a Case-Based Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Statin Myopathy: a Common Dilemma Not Reflected in Clinical Trials
REVIEW CME EDUCATIONAL OBJECTIVE: Readers will assess possible statin-induced myopathy in their patients on statins CREDIT GENARO FERNANDEZ, MD ERICA S. SPATZ, MD CHARLES JABLECKI, MD PAUL S. PHILLIPS, MD Internal Medicine Residency Program, Robert Wood Johnson Clinical Scholars Department of Neurosciences, University Director, Interventional Cardiology, The University of Utah, Salt Lake City Program, Cardiovascular Disease Fellow, of California San Diego, La Jolla Department of Cardiology, Scripps Mercy Yale University School of Medicine, New Hospital, San Diego, CA Haven, CT Statin myopathy: A common dilemma not reflected in clinical trials ■■ ABSTRACT hen a patient taking a statin complains Wof muscle aches, is he or she experiencing Although statins are remarkably effective, they are still statin-induced myopathy or some other prob- underprescribed because of concerns about muscle toxic- lem? Should statin therapy be discontinued? Statins have proven efficacy in preventing ity. We review the aspects of statin myopathy that are 1 important to the primary care physician and provide a heart attacks and death, and they are the most guide for evaluating patients on statins who present with widely prescribed drugs worldwide. Neverthe- less, they remain underused, with only 50% of muscle complaints. We outline the differential diagnosis, those who would benefit from being on a statin the risks and benefits of statin therapy in patients with receiving one.2,3 In addition, at least 25% of possible toxicity, and the subsequent treatment options. adults who start taking statins stop taking them 4 ■■ by 6 months, and up to 60% stop by 2 years. KEY POINTS Patient and physician fears about myopathy There is little consensus on the definition of statin-in- remain a key reason for stopping. -

(Lcrs) in 22Q11 Mediate Deletions, Duplications, Translocations, and Genomic Instability: an Update and Literature Review Tamim H
review January/February 2001 ⅐ Vol. 3 ⅐ No. 1 Evolutionarily conserved low copy repeats (LCRs) in 22q11 mediate deletions, duplications, translocations, and genomic instability: An update and literature review Tamim H. Shaikh, PhD1, Hiroki Kurahashi, MD, PhD1, and Beverly S. Emanuel, PhD1,2 Several constitutional rearrangements, including deletions, duplications, and translocations, are associated with 22q11.2. These rearrangements give rise to a variety of genomic disorders, including DiGeorge, velocardiofacial, and conotruncal anomaly face syndromes (DGS/VCFS/CAFS), cat eye syndrome (CES), and the supernumerary der(22)t(11;22) syndrome associated with the recurrent t(11;22). Chromosome 22-specific duplications or low copy repeats (LCRs) have been directly implicated in the chromosomal rearrangements associated with 22q11.2. Extensive sequence analysis of the different copies of 22q11 LCRs suggests a complex organization. Examination of their evolutionary origin suggests that the duplications in 22q11.2 may predate the divergence of New World monkeys 40 million years ago. Based on the current data, a number of models are proposed to explain the LCR-mediated constitutional rearrangements of 22q11.2. Genetics in Medicine, 2001:3(1):6–13. Key Words: duplication, evolution, 22q11, deletion and translocation Although chromosome 22 represents only 2% of the haploid The 22q11.2 deletion syndrome, which includes DGS/ human genome,1 recurrent, clinically significant, acquired, VCFS/CAFS, is the most common microdeletion syndrome. and somatic -

RD-Action Matchmaker – Summary of Disease Expertise Recorded Under
Summary of disease expertise recorded via RD-ACTION Matchmaker under each Thematic Grouping and EURORDIS Members’ Thematic Grouping Thematic Reported expertise of those completing the EURORDIS Member perspectives on Grouping matchmaker under each heading Grouping RD Thematically Rare Bone Achondroplasia/Hypochondroplasia Achondroplasia Amelia skeletal dysplasia’s including Achondroplasia/Growth hormone cleidocranial dysostosis, arthrogryposis deficiency/MPS/Turner Brachydactyly chondrodysplasia punctate Fibrous dysplasia of bone Collagenopathy and oncologic disease such as Fibrodysplasia ossificans progressive Li-Fraumeni syndrome Osteogenesis imperfecta Congenital hand and fore-foot conditions Sterno Costo Clavicular Hyperostosis Disorders of Sex Development Duchenne Muscular Dystrophy Ehlers –Danlos syndrome Fibrodysplasia Ossificans Progressiva Growth disorders Hypoparathyroidism Hypophosphatemic rickets & Nutritional Rickets Hypophosphatasia Jeune’s syndrome Limb reduction defects Madelung disease Metabolic Osteoporosis Multiple Hereditary Exostoses Osteogenesis imperfecta Osteoporosis Paediatric Osteoporosis Paget’s disease Phocomelia Pseudohypoparathyroidism Radial dysplasia Skeletal dysplasia Thanatophoric dwarfism Ulna dysplasia Rare Cancer and Adrenocortical tumours Acute monoblastic leukaemia Tumours Carcinoid tumours Brain tumour Craniopharyngioma Colon cancer, familial nonpolyposis Embryonal tumours of CNS Craniopharyngioma Ependymoma Desmoid disease Epithelial thymic tumours in -

SUPPLEMENTARY MATERIAL Supplementary 1. International
SUPPLEMENTARY MATERIAL Supplementary 1. International Myositis Classification Criteria Project Steering Committee Supplementary 2. Pilot study Supplementary 3. International Myositis Classification Criteria Project questionnaire Supplementary 4. Glossary and definitions for the International Myositis Classification Criteria Project questionnaire Supplementary 5. Adult comparator cases in the International Myositis Classification Criteria Project dataset Supplementary 6. Juvenile comparator cases in the International Myositis Classification Criteria Project dataset Supplementary 7. Validation cohort from the Euromyositis register Supplementary 8. Validation cohort from the Juvenile dermatomyositis cohort biomarker study and repository (UK and Ireland) 1 Supplementary 1. International Myositis Classification Criteria Project Steering Committee Name Affiliation Lars Alfredsson Institute for Environmental Medicine, Karolinska Institutet, Stockholm, Sweden Anthony A Amato Department of Neurology, Brigham and Women’s Hospital, Harvard Medical School, Boston, USA Richard J Barohn Department of Neurology, University of Kansas Medical Center, Kansas City, USA Matteo Bottai Institute for Environmental Medicine, Karolinska Institutet, Stockholm, Sweden Matthew H Liang Division of Rheumatology, Immunology and Allergy, Brigham and Women´s Hospital, Boston, USA Ingrid E Lundberg (Project Director) Rheumatology Unit, Department of Medicine, Karolinska University Hospital, Solna, Karolinska Institutet, Stockholm, Sweden Frederick W Miller Environmental -

Abstracts from the 50Th European Society of Human Genetics Conference: Electronic Posters
European Journal of Human Genetics (2019) 26:820–1023 https://doi.org/10.1038/s41431-018-0248-6 ABSTRACT Abstracts from the 50th European Society of Human Genetics Conference: Electronic Posters Copenhagen, Denmark, May 27–30, 2017 Published online: 1 October 2018 © European Society of Human Genetics 2018 The ESHG 2017 marks the 50th Anniversary of the first ESHG Conference which took place in Copenhagen in 1967. Additional information about the event may be found on the conference website: https://2017.eshg.org/ Sponsorship: Publication of this supplement is sponsored by the European Society of Human Genetics. All authors were asked to address any potential bias in their abstract and to declare any competing financial interests. These disclosures are listed at the end of each abstract. Contributions of up to EUR 10 000 (ten thousand euros, or equivalent value in kind) per year per company are considered "modest". Contributions above EUR 10 000 per year are considered "significant". 1234567890();,: 1234567890();,: E-P01 Reproductive Genetics/Prenatal and fetal echocardiography. The molecular karyotyping Genetics revealed a gain in 8p11.22-p23.1 region with a size of 27.2 Mb containing 122 OMIM gene and a loss in 8p23.1- E-P01.02 p23.3 region with a size of 6.8 Mb containing 15 OMIM Prenatal diagnosis in a case of 8p inverted gene. The findings were correlated with 8p inverted dupli- duplication deletion syndrome cation deletion syndrome. Conclusion: Our study empha- sizes the importance of using additional molecular O¨. Kırbıyık, K. M. Erdog˘an, O¨.O¨zer Kaya, B. O¨zyılmaz, cytogenetic methods in clinical follow-up of complex Y. -

Orphanet Report Series Rare Diseases Collection
Marche des Maladies Rares – Alliance Maladies Rares Orphanet Report Series Rare Diseases collection DecemberOctober 2013 2009 List of rare diseases and synonyms Listed in alphabetical order www.orpha.net 20102206 Rare diseases listed in alphabetical order ORPHA ORPHA ORPHA Disease name Disease name Disease name Number Number Number 289157 1-alpha-hydroxylase deficiency 309127 3-hydroxyacyl-CoA dehydrogenase 228384 5q14.3 microdeletion syndrome deficiency 293948 1p21.3 microdeletion syndrome 314655 5q31.3 microdeletion syndrome 939 3-hydroxyisobutyric aciduria 1606 1p36 deletion syndrome 228415 5q35 microduplication syndrome 2616 3M syndrome 250989 1q21.1 microdeletion syndrome 96125 6p subtelomeric deletion syndrome 2616 3-M syndrome 250994 1q21.1 microduplication syndrome 251046 6p22 microdeletion syndrome 293843 3MC syndrome 250999 1q41q42 microdeletion syndrome 96125 6p25 microdeletion syndrome 6 3-methylcrotonylglycinuria 250999 1q41-q42 microdeletion syndrome 99135 6-phosphogluconate dehydrogenase 67046 3-methylglutaconic aciduria type 1 deficiency 238769 1q44 microdeletion syndrome 111 3-methylglutaconic aciduria type 2 13 6-pyruvoyl-tetrahydropterin synthase 976 2,8 dihydroxyadenine urolithiasis deficiency 67047 3-methylglutaconic aciduria type 3 869 2A syndrome 75857 6q terminal deletion 67048 3-methylglutaconic aciduria type 4 79154 2-aminoadipic 2-oxoadipic aciduria 171829 6q16 deletion syndrome 66634 3-methylglutaconic aciduria type 5 19 2-hydroxyglutaric acidemia 251056 6q25 microdeletion syndrome 352328 3-methylglutaconic -

Download File
Freely available online Conference Proceedings Proceedings of the Ninth International Meeting on Neuroacanthocytosis Syndromes 1 1,2,3 Editors: Kevin Peikert & Andreas Hermann 1 Department of Neurology, University Hospital Carl Gustav Carus, Technische Universita¨t Dresden, Dresden, Germany, 2 Center for Regenerative Therapies Dresden (CRTD), Technische Universita¨t Dresden, Dresden, Germany, 3 German Center for Neurodegenerative Diseases (DZNE) Dresden, Dresden, Germany Citation: Peikert K, Hermann A, editors. Proceedings of the ninth international meeting on neuroacanthocytosis syndromes; 2018 March 23–25; Dresden, Germany. Tremor Other Hyperkinet Mov. 2018; 8. doi: 10.7916/D8ZC9KCW Published: July 17, 2018 Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution–Noncommercial–No Derivatives License, which permits the user to copy, distribute, and transmit the work provided that the original author(s) and source are credited; that no commercial use is made of the work; and that the work is not altered or transformed. Introduction its genetic basis in 2001. In spite of the wealth of in vivo and in The 9th International Meeting on Neuroacanthocytosis Syndromes vitro models presented at neuroacanthocytosis symposia past and was held on March 23th–25th, 2018 in Dresden, Germany. The present, its function (or functions) has so far remained elusive. conference followed the tradition of the previous eight international It may be worthwhile to review features of the disease for clues. symposia, the last of which was held in Ann Arbor, USA in May, 2016. 1) ChAc is an autosomal-recessive condition. 2) Gender distribution Following the positive response to the previous meeting, a major appears equal. -

The Genetic Relationship Between Paroxysmal Movement Disorders and Epilepsy
Review article pISSN 2635-909X • eISSN 2635-9103 Ann Child Neurol 2020;28(3):76-87 https://doi.org/10.26815/acn.2020.00073 The Genetic Relationship between Paroxysmal Movement Disorders and Epilepsy Hyunji Ahn, MD, Tae-Sung Ko, MD Department of Pediatrics, Asan Medical Center Children’s Hospital, University of Ulsan College of Medicine, Seoul, Korea Received: May 1, 2020 Revised: May 12, 2020 Seizures and movement disorders both involve abnormal movements and are often difficult to Accepted: May 24, 2020 distinguish due to their overlapping phenomenology and possible etiological commonalities. Par- oxysmal movement disorders, which include three paroxysmal dyskinesia syndromes (paroxysmal Corresponding author: kinesigenic dyskinesia, paroxysmal non-kinesigenic dyskinesia, paroxysmal exercise-induced dys- Tae-Sung Ko, MD kinesia), hemiplegic migraine, and episodic ataxia, are important examples of conditions where Department of Pediatrics, Asan movement disorders and seizures overlap. Recently, many articles describing genes associated Medical Center Children’s Hospital, University of Ulsan College of with paroxysmal movement disorders and epilepsy have been published, providing much infor- Medicine, 88 Olympic-ro 43-gil, mation about their molecular pathology. In this review, we summarize the main genetic disorders Songpa-gu, Seoul 05505, Korea that results in co-occurrence of epilepsy and paroxysmal movement disorders, with a presenta- Tel: +82-2-3010-3390 tion of their genetic characteristics, suspected pathogenic mechanisms, and detailed descriptions Fax: +82-2-473-3725 of paroxysmal movement disorders and seizure types. E-mail: [email protected] Keywords: Dyskinesias; Movement disorders; Seizures; Epilepsy Introduction ies, and paroxysmal dyskinesias [3,4]. Paroxysmal dyskinesias are an important disease paradigm asso- Movement disorders often arise from the basal ganglia nuclei or ciated with overlapping movement disorders and seizures [5]. -
The Frequency of Seizures with Roseola. the Study Corroborates the Suggestion That Seizures with Roseola, HHV-6, and Fever Are Not Always Simple in Type
the frequency of seizures with roseola. The study corroborates the suggestion that seizures with roseola, HHV-6, and fever are not always simple in type. They are frequently prolonged, recurrent, and complex, and sometimes a manifestation of encephalitis or encephalopathy. (Progress in Pediatric Neurology II. Millichap JG, Ed, PNB Publ, 1994, pp 410, 415). These findings further weaken the hypothesis of the so-called simple febrile seizure as a distinct disease entity. For abstracts from the 16th annual conference on febrile convulsions held in Tokyo, Dec 18, 1993, see Fukuyama Y. Brain Dev July/Aug 1994;16:339-346. Papers included neurochemical aspects, EEG studies, and clinical, epidemiological, and treatment reports. The reputed safety and effectiveness of intermittent oral diazepam (0.4 mg/kg, 3 doses) at times of fever for prevention of recurrence of febrile seizures was supported in 23 children treated at Shimane Medical University and Central Hospital, Japan. GLUTAMATE IN PYRIDOXINE-DEPENDENT EPILEPSY Cerebrospinal fluid levels of glutamate, g-aminobutyric acid, and pyridoxal-5-phosphate examined in a patient with pyridoxine dependency while on and off vitamin B6 treatment are reported from Universitat Munchen, and Universitats-Nervenklinik, Wurzburg, Germany. Seizures began at age 3 weeks. Despite phenobarbital, status epilepticus occurred at 3 months and was followed by infantile spasms and hypsarrhythmia. The addition of ACTH and vitamin B6 controlled the seizures and the EEG became normal. Seizures recurred on each of several occasions when vitamin B6 was withdrawn. CSF glutamate was elevated 200-fold, whereas GABA and PLP were normal. After vitamin B6 (5 mg/kg BW/day) was reintroduced, seizures stopped and the EEG was normal, but CSF glutamate was still elevated 10 fold. -

Febrile Seizures: Clinical Practice Guideline for the Long-Term Management of the Child with Simple Febrile Seizures
CLINICAL PRACTICE GUIDELINE Febrile Seizures: Clinical Practice Guideline for the Long-term Management of the Child With Simple Febrile Seizures Steering Committee on Quality Improvement and Management, Subcommittee on Febrile Seizures ABSTRACT Febrile seizures are the most common seizure disorder in childhood, affecting 2% to 5% of children between the ages of 6 and 60 months. Simple febrile seizures are www.pediatrics.org/cgi/doi/10.1542/ peds.2008-0939 defined as brief (Ͻ15-minute) generalized seizures that occur once during a 24-hour period in a febrile child who does not have an intracranial infection, doi:10.1542/peds.2008-0939 metabolic disturbance, or history of afebrile seizures. This guideline (a revision of All clinical reports from the American Academy of Pediatrics automatically expire the 1999 American Academy of Pediatrics practice parameter [now termed clinical 5 years after publication unless reaffirmed, practice guideline] “The Long-term Treatment of the Child With Simple Febrile revised, or retired at or before that time. Seizures”) addresses the risks and benefits of both continuous and intermittent The guidance in this report does not anticonvulsant therapy as well as the use of antipyretics in children with simple indicate an exclusive course of treatment febrile seizures. It is designed to assist pediatricians by providing an analytic or serve as a standard of medical care. Variations, taking into account individual framework for decisions regarding possible therapeutic interventions in this pa- circumstances, may be appropriate. tient population. It is not intended to replace clinical judgment or to establish a Key Word protocol for all patients with this disorder. -

EM Guidemap - Myopathy and Myoglobulinuria
myopathy EM guidemap - Myopathy and myoglobulinuria Click on any of the headings or subheadings to rapidly navigate to the relevant section of the guidemap Introduction General principles ● endocrine myopathy ● toxic myopathy ● periodic paralyses ● myoglobinuria Introduction - this short guidemap supplements the neuromuscular weakness guidemap and offers the reader supplementary information on myopathies, and a short section on myoglobulinuria - this guidemap only consists of a few brief checklists of "causes of the different types of myopathy" that an emergency physician may encounter in clinical practice when dealing with a patient with acute/subacute muscular weakness General principles - a myopathy is suggested when generalized muscle weakness involves large proximal muscle groups, especially around the shoulder and proximal girdle, and when the diffuse muscle weakness is associated with normal tendon reflexes and no sensory findings - a simple classification of myopathy:- Hereditary ● muscular dystrophies ● congenital myopathies http://www.homestead.com/emguidemaps/files/myopathy.html (1 of 13)8/20/2004 5:14:27 PM myopathy ● myotonias ● channelopathies (periodic paralysis syndromes) ● metabolic myopathies ● mitochondrial myopathies Acquired ● inflammatory myopathy ● endocrine myopathies ● drug-induced/toxic myopathies ● myopathy associated with systemic illness - a myopathy can present with fixed weakness (muscular dystrophy, inflammatory myopathy) or episodic weakness (periodic paralysis due to a channelopathy, metabolic myopathy -
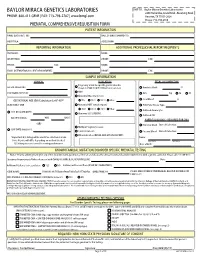
Prenatal Testing Requisition Form
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 PRENATAL COMPREHENSIVE REQUISITION FORM PATIENT INFORMATION NAME (LAST,FIRST, MI): DATE OF BIRTH (MM/DD/YY): HOSPITAL#: ACCESSION#: REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: SAMPLE INFORMATION CLINICAL INDICATION FETAL SPECIMEN TYPE Pregnancy at risk for specific genetic disorder DATE OF COLLECTION: (Complete FAMILIAL MUTATION information below) Amniotic Fluid: cc AMA PERFORMING PHYSICIAN: CVS: mg TA TC Abnormal Maternal Screen: Fetal Blood: cc GESTATIONAL AGE (GA) Calculation for AF-AFP* NTD TRI 21 TRI 18 Other: SELECT ONLY ONE: Abnormal NIPT (attach report): POC/Fetal Tissue, Type: TRI 21 TRI 13 TRI 18 Other: Cultured Amniocytes U/S DATE (MM/DD/YY): Abnormal U/S (SPECIFY): Cultured CVS GA ON U/S DATE: WKS DAYS PARENTAL BLOODS - REQUIRED FOR CMA -OR- Maternal Blood Date of Collection: Multiple Pregnancy Losses LMP DATE (MM/DD/YY): Parental Concern Paternal Blood Date of Collection: Other Indication (DETAIL AND ATTACH REPORT): *Important: U/S dating will be used if no selection is made. Name: Note: Results will differ depending on method checked. Last Name First Name U/S dating increases overall screening performance. Date of Birth: KNOWN FAMILIAL MUTATION/DISORDER SPECIFIC PRENATAL TESTING Notice: Prior to ordering testing for any of the disorders listed, you must call the lab and discuss the clinical history and sample requirements with a genetic counselor.