Investigation of Anti-Iglon5-Induced Neurodegenerative Changes in Human Neurons
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pathologic Thr175 Tau Phosphorylation in CTE and CTE with ALS
Published Ahead of Print on January 3, 2018 as 10.1212/WNL.0000000000004899 ARTICLE OPEN ACCESS Pathologic Thr175 tau phosphorylation in CTE and CTE with ALS Alexander J. Moszczynski, PhD, Wendy Strong, BSc, Kathy Xu, MSc, Ann McKee, MD, Arthur Brown, PhD, Correspondence and Michael J. Strong, MD Dr. M.J. Strong [email protected] Neurology® 2018;90:e1-8. doi:10.1212/WNL.0000000000004899 Abstract Objective To investigate whether chronic traumatic encephalopathy (CTE) and CTE with amyotrophic lateral sclerosis (CTE-ALS) exhibit features previously observed in other tauopathies of pathologic phosphorylation of microtubule-associated protein tau at Thr175 (pThr175 tau) and Thr231 (pThr231 tau), and glycogen synthase kinase–3β (GSK3β) activation, and whether these pathologic features are a consequence of traumatic brain injury (TBI). Methods Tau isoform expression was assayed by western blot in 6 stage III CTE cases. We also used immunohistochemistry to analyze 5 cases each of CTE, CTE-ALS, and 5 controls for ex- pression of activated GSK3β, pThr175 tau, pThr231 tau, and oligomerized tau within spinal cord tissue and hippocampus. Using a rat model of moderate TBI, we assessed tau pathology and phospho-GSK3β expression at 3 months postinjury. Results CTE and CTE-ALS are characterized by the presence of all 6 tau isoforms in both soluble and insoluble tau isolates. Activated GSK3β, pThr175 tau, pThr231 tau, and oligomerized tau protein expression was observed in hippocampal neurons and spinal motor neurons. We observed tau neuronal pathology (fibrillar inclusions and axonal damage) and increased levels of pThr175 tau and activated GSK3β in moderate TBI rats. Conclusions Pathologic phosphorylation of tau at Thr175 and Thr231 and activation of GSK3β are features of the tauopathy of CTE and CTE-ALS. -

Immune Effector Mechanisms and Designer Vaccines Stewart Sell Wadsworth Center, New York State Department of Health, Empire State Plaza, Albany, NY, USA
EXPERT REVIEW OF VACCINES https://doi.org/10.1080/14760584.2019.1674144 REVIEW How vaccines work: immune effector mechanisms and designer vaccines Stewart Sell Wadsworth Center, New York State Department of Health, Empire State Plaza, Albany, NY, USA ABSTRACT ARTICLE HISTORY Introduction: Three major advances have led to increase in length and quality of human life: Received 6 June 2019 increased food production, improved sanitation and induction of specific adaptive immune Accepted 25 September 2019 responses to infectious agents (vaccination). Which has had the most impact is subject to debate. KEYWORDS The number and variety of infections agents and the mechanisms that they have evolved to allow Vaccines; immune effector them to colonize humans remained mysterious and confusing until the last 50 years. Since then mechanisms; toxin science has developed complex and largely successful ways to immunize against many of these neutralization; receptor infections. blockade; anaphylactic Areas covered: Six specific immune defense mechanisms have been identified. neutralization, cytolytic, reactions; antibody- immune complex, anaphylactic, T-cytotoxicity, and delayed hypersensitivity. The role of each of these mediated cytolysis; immune immune effector mechanisms in immune responses induced by vaccination against specific infectious complex reactions; T-cell- mediated cytotoxicity; agents is the subject of this review. delayed hypersensitivity Expertopinion: In the past development of specific vaccines for infections agents was largely by trial and error. With an understanding of the natural history of an infection and the effective immune response to it, one can select the method of vaccination that will elicit the appropriate immune effector mechanisms (designer vaccines). These may act to prevent infection (prevention) or eliminate an established on ongoing infection (therapeutic). -

An Autopsy Case of Progressive Supranuclear Palsy with Incidental
Letters Discussion | This pilot study successfully explored the effect size 3. Korte J-M, Kaila T, Saari KM. Systemic bioavailability and cardiopulmonary of timolol eyedrops on migraine headaches. Several partici- effects of 0.5% timolol eyedrops. Graefes Arch Clin Exp Ophthalmol. 2002;240 (6):430-435. pants responded extremely well to the timolol. Further re- 4. Migliazzo CV, Hagan JC III. Beta blocker eyedrops for treatment of acute search is needed to determine what patient factors might pre- migraine. Mo Med. 2014;111(4):283-288. dict responsiveness to timolol. 5. Chiam PJT. Topical beta-blocker treatment for migraine. Int Ophthalmol. 2012; 32(1):85-88. Limitations. Study limitations include a small sample size, a 6. Headache Classification Committee of the International Headache Society. lack of investigator masking, and an imperfect placebo, as The international classification of headache disorders, 3rd edition (beta artificial tears tend to cause less of a burning sensation than version). https://www.ichd-3.org/wp-content/uploads/2016/08/International -Headache-Classification-III-ICHD-III-2013-Beta-1.pdf. Accessed June 1, 2016. timolol. With a half-life of 4 hours, timolol ophthalmic is unlikely to have had an association with repeated head- aches or beyond the 3-day washout period. Four 50-μL drops of timolol, 0.5%, represent 1 mg of timolol, which An Autopsy Case of Progressive Supranuclear compares with an oral prophylactic dosage of 10 to 30 mg of Palsy With Incidental ATXN2 Expansion timolol daily. Future research should aim for a target enroll- A case of multiple system atrophy with predominant parkin- ment of more than 86 participants and explore optimal dos- sonism (MSA-P) with ATXN2 (OMIM 601517) expansion was ing regimens. -
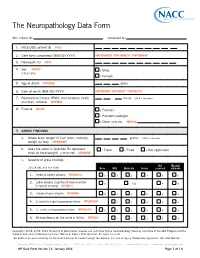
The Neuropathology Data Form
The Neuropathology Data Form ADC subject ID: Completed by: 1. MDS/UDS patient ID PTID 2. Date form completed (MM/DD/ YYYY) NPFORMMO / NPFORMDY / NPFORMYR 3. Neuropath ID NPID 4. Sex NPSEX 1 Male (CHECK ONE) 2 Female 5. Age at death NPDAGE years 6. Date of death (MM/ DD/ YYYY) NPDODMO / NPDODDY / NPDODYR 7. Postmortem interval (PMI): time between death . hours (99.9 = unknown) and brain removal NPPMIH 8. Fixative NPFIX 1 Formalin 2 Paraformaldehyde 7 Other (SPECIFY): NPFIXX 9. GROSS FINDINGS a. Whole brain weight (if half brain, multiply grams (9999 = unknown) weight by two) NPWBRWT b. Does the value in Question 9a represent 1 Fresh 2 Fixed 8 Not applicable fresh or fixed weight? (CHECK ONE) NPWBRF c. Severity of gross findings Not Missing/ (CHECK ONE BOX PER ROW) None Mild Moderate Severe assessed unknown 1. Cerebral cortex atrophy NPGRCCA 0 1 2 3 8 9 Lobar atrophy (significant frontal and/or 2. 0 1 Yes 8 9 temporal atrophy) NPGRLA 3. Hippocampus atrophy NPGRHA 0 1 2 3 8 9 4. Substantia nigra hypopigmentation NPGRSNH 1 2 3 8 9 5. L. ceruleus hypopigmentation NPGRLCH 0 1 2 3 8 9 6. Atherosclerosis (of the circle of Willis) NPAVAS 1 2 3 8 9 Copyright© 2006, 2008, 2014 University of Washington. Created and published by the Neuropathology Steering ommittee of the ADC Program and the National Alzheimer’s Coordinating Center (Walter A. Kukull, PhD, Director). All rights reserved. This publication was funded by the National Institutes of Health through the National Institute on Aging (Cooperative Agreement U01 AG016976). -

Identification of Genetic Modifiers in Hereditary Spastic Paraplegias Due to SPAST/SPG4 Mutations Livia Parodi
Identification of genetic modifiers in Hereditary Spastic Paraplegias due to SPAST/SPG4 mutations Livia Parodi To cite this version: Livia Parodi. Identification of genetic modifiers in Hereditary Spastic Paraplegias due to SPAST/SPG4 mutations. Human health and pathology. Sorbonne Université, 2019. English. NNT : 2019SORUS317. tel-03141229 HAL Id: tel-03141229 https://tel.archives-ouvertes.fr/tel-03141229 Submitted on 15 Feb 2021 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Sorbonne Université Institut du Cerveau et de la Moelle Épinière École Doctorale Cerveau-Cognition-Comportement Thèse de doctorat en Neurosciences Identification of genetic modifiers in Hereditary Spastic Paraplegias due to SPAST/SPG4 mutations Soutenue le 9 octobre 2019 par Livia Parodi Membres du jury : Pr Bruno Stankoff Président Pr Lesley Jones Rapporteur Dr Susanne de Bot Rapporteur Pr Christel Depienne Examinateur Pr Cyril Goizet Examinateur Pr Alexandra Durr Directeur de thèse Table of contents Abbreviations _________________________________________________________ -

And Α-Synuclein Pathology in a Case of Hereditary Spastic Paraplegia SPG7 with an Ala510val Mutation
Int. J. Mol. Sci. 2015, 16, 25050-25066; doi:10.3390/ijms161025050 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Article Abnormal Paraplegin Expression in Swollen Neurites, τ- and α-Synuclein Pathology in a Case of Hereditary Spastic Paraplegia SPG7 with an Ala510Val Mutation Dietmar R. Thal 1,2,*, Stephan Züchner 3,4, Stephan Gierer 5, Claudia Schulte 6,7, Ludger Schöls 6,7, Rebecca Schüle 3,6,7,† and Matthis Synofzik 5,6,†,* 1 Laboratory of Neuropathology—Institute of Pathology, Center of Clinical Research, University of Ulm, Helmholtzstraße 8/1, D-89081 Ulm, Germany 2 Department of Neuroscience, Katholieke Universiteit Leuven, B-3000 Leuven, Belgium 3 Dr. John T. Macdonald Foundation Department of Human Genetics University of Miami Miller School of Medicine, Miami, FL 33136, USA; E-Mails: [email protected] (S.Z.); [email protected] (R.S.) 4 John P. Hussman Institute for Human Genomics, University of Miami Miller School of Medicine, Miami, FL 33136, USA 5 Outpatient Praxis for Neurology, D-89407 Dillingen, Germany; E-Mail: [email protected] 6 Department of Neurodegenerative Diseases, Hertie-Institute for Clinical Brain Research, Hoppe-Seyler-Strasse 3, University of Tübingen, 72077 Tübingen, Germany; E-Mails: [email protected] (C.S.); [email protected] (L.S.) 7 German Research Center for Neurodegenerative Diseases (DZNE), University of Tübingen, 72076 Tuebingen, Germany † These authors contributed equally to this work. * Authors to whom correspondence should be addressed; E-Mails: [email protected] (D.R.T.); [email protected] (M.S.); Tel.: +32-16-3-44047 (D.R.T); +49-7071-298-2060 (M.S.); Fax: +32-16-3-36548 (D.R.T); +49-7071-2925-0001 (M.S.). -

Alzheimer Disease and Hereditary Spastic Paraplegia Hans Zempel1,3* and Eva-Maria Mandelkow1,2,3*
Zempel and Mandelkow Molecular Neurodegeneration (2015) 10:68 DOI 10.1186/s13024-015-0064-1 REVIEW Open Access Tau missorting and spastin-induced microtubule disruption in neurodegeneration: Alzheimer Disease and Hereditary Spastic Paraplegia Hans Zempel1,3* and Eva-Maria Mandelkow1,2,3* Abstract In Alzheimer Disease (AD), the mechanistic connection of the two major pathological hallmarks, namely deposition of Amyloid-beta (Aβ) in the form of extracellular plaques, and the pathological changes of the intracellular protein Tau (such as phosphorylation, missorting, aggregation), is not well understood. Genetic evidence from AD and Down Syndrome (Trisomy 21), and animal models thereof, suggests that aberrant production of Aβ is upstream of Tau aggregation, but also points to Tau as a critical effector in the pathological process. Yet, the cascade of events leading from increased levels of Aβ to Tau-dependent toxicity remains a matter of debate. Using primary neurons exposed to oligomeric forms of Aβ, we have found that Tau becomes mislocalized (missorted) into the somatodendritic compartment. Missorting of Tau correlates with loss of microtubules and downstream consequences such as loss of mature spines, loss of synaptic activity, and mislocalization of mitochondria. In this cascade, missorting of Tau induces mislocalization of TTLL6 (Tubulin-Tyrosine-Ligase-Like 6) into the dendrites. TTLL6 induces polyglutamylation of microtubules, which acts as a trigger for spastin mediated severing of dendritic microtubules. Loss of microtubules makes cells unable to maintain transport of mitochondria, which in turn results in synaptic dysfunction and loss of mature spines. These pathological changes are absent in TauKO derived primary neurons. Thus, Tau mediated mislocalization of TTLL6 and spastin activation reveals a pathological gain of function for Tau and spastin in this cellular model system of AD. -

No Metagenomic Evidence of Causative Viral Pathogens in Postencephalitic Parkinsonism Following Encephalitis Lethargica
microorganisms Communication No Metagenomic Evidence of Causative Viral Pathogens in Postencephalitic Parkinsonism Following Encephalitis Lethargica Dániel Cadar 1 , Kurt A. Jellinger 2, Peter Riederer 3, Sabrina Strobel 4, Camelia-Maria Monoranu 4 and Dennis Tappe 1,* 1 Bernhard Nocht Institute for Tropical Medicine, 20359 Hamburg, Germany; [email protected] 2 Institute of Clinical Neurobiology, 1090 Vienna, Austria; [email protected] 3 Center of Mental Health, Department of Psychiatry, Psychosomatics and Psychotherapy, University Hospital of Würzburg, 97080 Würzburg, Germany; [email protected] 4 Department of Neuropathology, Institute for Pathology, University of Würzburg, 97080 Würzburg, Germany; [email protected] (S.S.); [email protected] (C.-M.M.) * Correspondence: [email protected] Abstract: Postencephalitic parkinsonism (PEP) is a disease of unknown etiology and pathophysiol- ogy following encephalitis lethargica (EL), an acute-onset polioencephalitis of cryptic cause in the 1920s. PEP is a tauopathy with multisystem neuronal loss and gliosis, clinically characterized by bradykinesia, rigidity, rest tremor, and oculogyric crises. Though a viral cause of EL is likely, past polymerase chain reaction-based investigations in the etiology of both PEP and EL were negative. PEP might be caused directly by an unknown viral pathogen or the consequence of a post-infectious im- munopathology. The development of metagenomic next-generation sequencing in conjunction with Citation: Cadar, D.; Jellinger, K.A.; bioinformatic techniques has generated a broad-range tool for the detection of unknown pathogens Riederer, P.; Strobel, S.; Monoranu, C.-M.; Tappe, D. No Metagenomic in the recent past. Retrospective identification and characterization of pathogens responsible for past Evidence of Causative Viral infectious diseases can be successfully performed with formalin-fixed paraffin-embedded (FFPE) Pathogens in Postencephalitic tissue samples. -

Novel Therapeutic Targets and Biomarkers for the Treatment Of
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 12 June 2020 doi:10.20944/preprints202006.0147.v1 Novel Therapeutic Targets and Biomarkers for the Treatment of Progressive Supranuclear Palsy Imogen F C Tyer, Alison M Hill* *corresponding author, [email protected], Geoffrey Pope Building, University of Exeter , Stocker Road, Exeter, EX4 4QD, UK. Imogen F C Tyer: [email protected], ORCID ID: 0000-0001-8393-7023 Alison M Hill: [email protected], ORCID ID: 0000-0001-8084-3048 Abstract Progressive supranuclear palsy (PSP) is a sporadic parkinsonism tauopathy characterised by the deposition of aggregations of abnormal, hyperphosphorylated four-repeat tau (4R-tau). A revised clinical diagnostic criterion for PSP allows early presentations for the full spectrum of clinical phenotypes to be recognised enabling doctors to make a more accurate diagnosis. The major genetic risk factor for sporadic PSP is a common variant in the gene encoding microtubule-associated protein tau (MAPT). Research into the biochemical and pathological pathways of tau is vital to improve the chances of developing an effective diagnostic biomarker to monitor tau pathogenesis. Neuroimaging biomarkers, such as tau PET ligands, are proving the most successful tool in providing a differential diagnosis between neurodegenerative disorders. There are currently no effective treatments for PSP, however tau-directed therapies in the last five years have rapidly advanced. Latest tau therapies are proposed to have disease-modifying effects by reducing toxic aggregations of tau through manipulating tau gene expression. After encouraging results from long awaited trials, additional funding is being injected into this field and with new results expected, this proves an exciting area for scientific discovery. -

Tau Protein and Tauopathy (PDF)
94 TAU PROTEIN AND TAUOPATHY MAKOTO HIGUCHI JOHN Q. TROJANOWSKI VIRGINIA M.-Y. LEE TAU-POSITIVE FILAMENTOUS LESIONS IN neurites are frequently associated with amyloid plaques to NEURODEGENERATIVE DISEASES form neuritic plaques. Both amyloid plaques and neurofibrillary lesions are con- Neurofibrillary Lesions of Alzheimer’s sidered to play independent and/or interrelated roles in the Disease Brains mechanisms that underlie the onset and relentless progres- Although the mechanisms underlying the onset and pro- sion of brain degeneration in AD. Indeed, serveral studies gression of Alzheimer’s disease (AD) have not been fully have shown that NFTs correlate with the severity of demen- elucidated, the two diagnostic neuropathologies in the AD tia in AD, as do losses of synapses and neurons (10–13). brain (i.e., amyloid plaques and neurofibrillary lesions) (1, Although there is a poor correlation between these param- 2) have been implicated mechanistically in the degeneration eters and the concentration or distribution of amyloid de- of the AD brain, and they are considered to be plausible posits (11,13), this could reflect the turnover of these le- targets for the discovery of potential therapeutic agents to sions. Furthermore, it has been reported that a small treat this common dementing disorder. AD is a genotypi- population of AD patients show abundant NFTs but very cally and phenotypically heterogeneous disease. In spite of few amyloid plaques (14), which may signify that there is this genetic heterogeneity, abundant amyloid plaques and a causal relationship between the accumulation of NFTs neurofibrillary lesions, including neurofibrillary tangles and the clinical manifestations of AD. (NFTs), neuropil threads, and plaque neurites are observed Despite heterogeneity in the AD phenotype, the progres- consistently in all forms of AD, and both plaques and tan- sive accumulation of NFTs follows a stereotypical pattern gles are required to establish a definite diagnosis of AD in as described by Braak and Braak (15), who defined six neu- a patient with dementia. -

Unclassified Four-Repeat Tauopathy Associated with Familial
Nakano et al. acta neuropathol commun (2020) 8:148 https://doi.org/10.1186/s40478-020-01025-1 CASE REPORT Open Access Unclassifed four-repeat tauopathy associated with familial parkinsonism and progressive respiratory failure Masayoshi Nakano1†, Yuichi Riku2,6†, Kenya Nishioka3, Masato Hasegawa4, Yukihiko Washimi1, Yutaka Arahata1, Akinori Takeda1, Kentaro Horibe1, Akiko Yamaoka1, Keisuke Suzuki1, Masashi Tsujimoto1, Yuanzhe Li3, Hiroyo Yoshino5, Nobutaka Hattori3,5, Akio Akagi2, Hiroaki Miyahara2, Yasushi Iwasaki2 and Mari Yoshida2* Abstract We describe an autopsied patient with familial parkinsonism and unclassifed four repeat-tau (4R-tau) aggregation. She presented with bradykinesia, truncal dystonia, and mild amnesia at the age of 61 and then exhibited body weight loss (15 kg over 8 months), sleep disturbances, and progressive respiratory failure with CO 2 narcosis. She died of res- piratory failure at the age of 62, 14 months after disease onset. Her brother also showed parkinsonism at the age of 58 and suddenly died 6 months later. Postmortem examination revealed 4R-tau aggregation, which was characterized by neuronal globose-type tangles or pretangles, bush-like or miscellaneous astrocytic inclusions, and coiled bodies. The temporal tip, the striatum, the substantia nigra, the tegmentum of the midbrain, the medullary reticular formation, and the spinal cord were severely involved with tau aggregation. Argyrophilic grains and ballooned neurons were also found in the medial temporal structures, however, extensions of the 4R-aggregations in the case were clearly broader than those of the argyrophilic grains. Western blot analysis of sarkosyl-insoluble fractions from brain lysates revealed prominent bands of tau at both 33 kDa and 37 kDa. -

Disease-Related Phenotypes in a Drosophila Model of Hereditary Spastic Paraplegia Are Ameliorated by Treatment with Vinblastine
Disease-related phenotypes in a Drosophila model of hereditary spastic paraplegia are ameliorated by treatment with vinblastine Genny Orso, … , Mel Feany, Andrea Daga J Clin Invest. 2005;115(11):3026-3034. https://doi.org/10.1172/JCI24694. Research Article Neuroscience Hereditary spastic paraplegias (HSPs) are a group of neurodegenerative diseases characterized by progressive weakness and spasticity of the lower limbs. Dominant mutations in the human SPG4 gene, encoding spastin, are responsible for the most frequent form of HSP. Spastin is an ATPase that binds microtubules and localizes to the spindle pole and distal axon in mammalian cell lines. Furthermore, its Drosophila homolog, Drosophila spastin (Dspastin), has been recently shown to regulate microtubule stability and synaptic function at the Drosophila larval neuromuscular junction. Here we report the generation of a spastin-linked HSP animal model and show that in Drosophila, neural knockdown of Dspastin and, conversely, neural overexpression of Dspastin containing a conserved pathogenic mutation both recapitulate some phenotypic aspects of the human disease, including adult onset, locomotor impairment, and neurodegeneration. At the subcellular level, neuronal expression of both Dspastin RNA interference and mutant Dspastin cause an excessive stabilization of microtubules in the neuromuscular junction synapse. In addition, we provide evidence that administration of the microtubule targeting drug vinblastine significantly attenuates these phenotypes in vivo. Our findings demonstrate that loss of spastin function elicits HSP-like phenotypes in Drosophila, provide novel insights into the molecular mechanism of spastin mutations, and raise the possibility that therapy with Vinca alkaloids may be efficacious in spastin-associated HSP and other disorders related to microtubule dysfunction.