Microglia Implicated in Tauopathy in the Striatum of Neurodegenerative Disease Patients from Genotype to Phenotype
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lewy Bodies in the Amygdala Increase of ␣-Synuclein Aggregates in Neurodegenerative Diseases with Tau-Based Inclusions
ORIGINAL CONTRIBUTION Lewy Bodies in the Amygdala Increase of ␣-Synuclein Aggregates in Neurodegenerative Diseases With Tau-Based Inclusions Anca Popescu, MD; Carol F. Lippa, MD; Virginia M.-Y. Lee, PhD; John Q. Trojanowski, MD, PhD Background: Increased attention has been given to Results: Lewy bodies were often abundant in classic Pick ␣-synuclein aggregation in nonsynucleinopathies be- disease, argyrophilic grain disease, Alzheimer disease, and cause ␣-synuclein–containing Lewy bodies (LBs) influ- dementia with LBs but not in cases with amygdala de- ence symptoms. However, the spectrum of disorders in generation lacking tau-based inclusions, control cases, which secondary inclusions are likely to occur has not preclinical disease carriers, or degenerative diseases lack- been defined. Amygdala neurons commonly develop large ing pathologic involvement of the amygdala. The ex- numbers of secondary LBs, making it a practical region posed ␣-synuclein epitopes were similar in all cases con- for studying this phenomenon. taining LBs. Objective: To characterize the spectrum of diseases as- Conclusions: Abnormal ␣-synuclein aggregation in the sociated with LB formation in the amygdala of neurode- amygdala is disease selective, but not restricted to dis- generative disease and control cases. orders of ␣-synuclein and -amyloid. Our data are com- patible with the notion that tau aggregates predispose neu- Design: An autopsy series of 101 neurodegenerative dis- ease and 34 aged control cases. Using immunohisto- rons to develop secondary LBs. chemistry studies, we examined the amygdala for ␣-synuclein aggregates. Arch Neurol. 2004;61:1915-1919 GGREGATION OF ␣-SY- of these subjects.7-9 It is unknown whether nuclein has a primary this curious finding is restricted to AD, or pathogenic role in spo- whether it is a more universal phenom- radic and familial autoso- enon. -

Pathologic Thr175 Tau Phosphorylation in CTE and CTE with ALS
Published Ahead of Print on January 3, 2018 as 10.1212/WNL.0000000000004899 ARTICLE OPEN ACCESS Pathologic Thr175 tau phosphorylation in CTE and CTE with ALS Alexander J. Moszczynski, PhD, Wendy Strong, BSc, Kathy Xu, MSc, Ann McKee, MD, Arthur Brown, PhD, Correspondence and Michael J. Strong, MD Dr. M.J. Strong [email protected] Neurology® 2018;90:e1-8. doi:10.1212/WNL.0000000000004899 Abstract Objective To investigate whether chronic traumatic encephalopathy (CTE) and CTE with amyotrophic lateral sclerosis (CTE-ALS) exhibit features previously observed in other tauopathies of pathologic phosphorylation of microtubule-associated protein tau at Thr175 (pThr175 tau) and Thr231 (pThr231 tau), and glycogen synthase kinase–3β (GSK3β) activation, and whether these pathologic features are a consequence of traumatic brain injury (TBI). Methods Tau isoform expression was assayed by western blot in 6 stage III CTE cases. We also used immunohistochemistry to analyze 5 cases each of CTE, CTE-ALS, and 5 controls for ex- pression of activated GSK3β, pThr175 tau, pThr231 tau, and oligomerized tau within spinal cord tissue and hippocampus. Using a rat model of moderate TBI, we assessed tau pathology and phospho-GSK3β expression at 3 months postinjury. Results CTE and CTE-ALS are characterized by the presence of all 6 tau isoforms in both soluble and insoluble tau isolates. Activated GSK3β, pThr175 tau, pThr231 tau, and oligomerized tau protein expression was observed in hippocampal neurons and spinal motor neurons. We observed tau neuronal pathology (fibrillar inclusions and axonal damage) and increased levels of pThr175 tau and activated GSK3β in moderate TBI rats. Conclusions Pathologic phosphorylation of tau at Thr175 and Thr231 and activation of GSK3β are features of the tauopathy of CTE and CTE-ALS. -

Immune Effector Mechanisms and Designer Vaccines Stewart Sell Wadsworth Center, New York State Department of Health, Empire State Plaza, Albany, NY, USA
EXPERT REVIEW OF VACCINES https://doi.org/10.1080/14760584.2019.1674144 REVIEW How vaccines work: immune effector mechanisms and designer vaccines Stewart Sell Wadsworth Center, New York State Department of Health, Empire State Plaza, Albany, NY, USA ABSTRACT ARTICLE HISTORY Introduction: Three major advances have led to increase in length and quality of human life: Received 6 June 2019 increased food production, improved sanitation and induction of specific adaptive immune Accepted 25 September 2019 responses to infectious agents (vaccination). Which has had the most impact is subject to debate. KEYWORDS The number and variety of infections agents and the mechanisms that they have evolved to allow Vaccines; immune effector them to colonize humans remained mysterious and confusing until the last 50 years. Since then mechanisms; toxin science has developed complex and largely successful ways to immunize against many of these neutralization; receptor infections. blockade; anaphylactic Areas covered: Six specific immune defense mechanisms have been identified. neutralization, cytolytic, reactions; antibody- immune complex, anaphylactic, T-cytotoxicity, and delayed hypersensitivity. The role of each of these mediated cytolysis; immune immune effector mechanisms in immune responses induced by vaccination against specific infectious complex reactions; T-cell- mediated cytotoxicity; agents is the subject of this review. delayed hypersensitivity Expertopinion: In the past development of specific vaccines for infections agents was largely by trial and error. With an understanding of the natural history of an infection and the effective immune response to it, one can select the method of vaccination that will elicit the appropriate immune effector mechanisms (designer vaccines). These may act to prevent infection (prevention) or eliminate an established on ongoing infection (therapeutic). -

Investigation of Anti-Iglon5-Induced Neurodegenerative Changes in Human Neurons
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.27.269795; this version posted August 28, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Manuscript BioRxiv Investigation of anti-IgLON5-induced neurodegenerative changes in human neurons Mattias Gamre1,2, Matias Ryding1,2, Mette Scheller Nissen1,2,3, Anna Christine Nilsson4, Morten Meyer1,2,5, Morten Blaabjerg1,2,3,5 1Neurobiological Research, Institute of Molecular Medicine, University of Southern Denmark, Odense, Denmark. 2Department of Neurology, Odense University Hospital, Odense, Odense, Denmark 3Department of Clinical Research, Odense University Hospital, Odense, Denmark 4Department of Clinical Immunology, Odense University Hospital, Odense, Denmark 5BRIDGE – Brain Research Inter-Disciplinary Guided Excellence, Department of Clinical Research, University of Southern Denmark, Odense, Denmark Number of pages: 12 Number of figures: 4 Keywords: IgLON5, Autoimmune encephalitis, neurodegeneration, inflammation, Tau Corresponding author Professor Morten Blaabjerg, MD, PhD Department of Neurology Odense University Hospital J.B. Winsløws Vej 4 5000 Odense C Denmark Phone: (+45) 6541 2457 E-mail: [email protected] Page 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.27.269795; this version posted August 28, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. -

When DLB, PD, and PSP Masquerade As MSA an Autopsy Study of 134 Patients
When DLB, PD, and PSP masquerade as MSA An autopsy study of 134 patients Shunsuke Koga, MD ABSTRACT Naoya Aoki, MD Objective: To determine ways to improve diagnostic accuracy of multiple system atrophy (MSA), Ryan J. Uitti, MD we assessed the diagnostic process in patients who came to autopsy with antemortem diagnosis Jay A. van Gerpen, MD of MSA by comparing clinical and pathologic features between those who proved to have MSA William P. Cheshire, MD and those who did not. We focus on likely explanations for misdiagnosis. Keith A. Josephs, MD Methods: This is a retrospective review of 134 consecutive patients with an antemortem clinical Zbigniew K. Wszolek, diagnosis of MSA who came to autopsy with neuropathologic evaluation of the brain. Of the 134 MD patients, 125 had adequate medical records for review. Clinical and pathologic features were J. William Langston, MD compared between patients with autopsy-confirmed MSA and those with other pathologic diag- Dennis W. Dickson, MD noses, including dementia with Lewy bodies (DLB), Parkinson disease (PD), and progressive supra- nuclear palsy (PSP). Correspondence to Results: Of the 134 patients with clinically diagnosed MSA, 83 (62%) had the correct diagnosis Dr. Dickson: at autopsy. Pathologically confirmed DLB was the most common misdiagnosis, followed by PSP [email protected] and PD. Despite meeting pathologic criteria for intermediate to high likelihood of DLB, several pa- tients with DLB did not have dementia and none had significant Alzheimer-type pathology. Auto- nomic failure was the leading cause of misdiagnosis in DLB and PD, and cerebellar ataxia was the leading cause of misdiagnosis in PSP. -

Lewy Body Diseases and Multiple System Atrophy As ␣-Synucleinopathies
Molecular Psychiatry (1998) 3, 462–465 1998 Stockton Press All rights reserved 1359–4184/98 $12.00 GUEST EDITORIAL Lewy body diseases and multiple system atrophy as ␣-synucleinopathies Parkinson’s disease and dementia with Lewy bodies synuclein are the first known genetic causes of Parkin- are among the most common neurodegenerative dis- son’s disease. They are located in the amino-terminal eases. They share the Lewy body and the Lewy neurite half of ␣-synuclein, which consists of seven imperfect as their defining neuropathological characteristics. repeats of 11 amino acids each, with the consensus Originally described in 1912 as a light-microscopic sequence KTKEGV (Figure 1). It has been suggested entity, the Lewy body was shown to be made of abnor- that ␣-synuclein may bind through these repeats to mal filaments in the 1960s. Over the past year, the bio- membranes rich in acidic phospholipids.3 chemical nature of the Lewy body filament has been This work raised the question whether ␣-synuclein revealed. is a component of Lewy bodies and Lewy neurites of A large number of different proteins has been idiopathic Parkinson’s disease and of dementia with reported to be present in Lewy bodies and Lewy neur- Lewy bodies. Using well-characterised anti-␣-synuc- ites by immunohistochemical methods. However, these lein antibodies, Spillantini et al showed strong staining findings do not permit us to distinguish between of both Lewy bodies and Lewy neurites in idiopathic intrinsic Lewy body components and normal cellular Parkinson’s disease and dementia with Lewy bodies.4 constituents that get merely trapped in the filaments They also reported the lack of staining of these patho- that make up the Lewy body. -

An Autopsy Case of Progressive Supranuclear Palsy with Incidental
Letters Discussion | This pilot study successfully explored the effect size 3. Korte J-M, Kaila T, Saari KM. Systemic bioavailability and cardiopulmonary of timolol eyedrops on migraine headaches. Several partici- effects of 0.5% timolol eyedrops. Graefes Arch Clin Exp Ophthalmol. 2002;240 (6):430-435. pants responded extremely well to the timolol. Further re- 4. Migliazzo CV, Hagan JC III. Beta blocker eyedrops for treatment of acute search is needed to determine what patient factors might pre- migraine. Mo Med. 2014;111(4):283-288. dict responsiveness to timolol. 5. Chiam PJT. Topical beta-blocker treatment for migraine. Int Ophthalmol. 2012; 32(1):85-88. Limitations. Study limitations include a small sample size, a 6. Headache Classification Committee of the International Headache Society. lack of investigator masking, and an imperfect placebo, as The international classification of headache disorders, 3rd edition (beta artificial tears tend to cause less of a burning sensation than version). https://www.ichd-3.org/wp-content/uploads/2016/08/International -Headache-Classification-III-ICHD-III-2013-Beta-1.pdf. Accessed June 1, 2016. timolol. With a half-life of 4 hours, timolol ophthalmic is unlikely to have had an association with repeated head- aches or beyond the 3-day washout period. Four 50-μL drops of timolol, 0.5%, represent 1 mg of timolol, which An Autopsy Case of Progressive Supranuclear compares with an oral prophylactic dosage of 10 to 30 mg of Palsy With Incidental ATXN2 Expansion timolol daily. Future research should aim for a target enroll- A case of multiple system atrophy with predominant parkin- ment of more than 86 participants and explore optimal dos- sonism (MSA-P) with ATXN2 (OMIM 601517) expansion was ing regimens. -
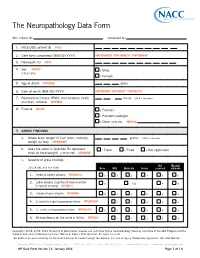
The Neuropathology Data Form
The Neuropathology Data Form ADC subject ID: Completed by: 1. MDS/UDS patient ID PTID 2. Date form completed (MM/DD/ YYYY) NPFORMMO / NPFORMDY / NPFORMYR 3. Neuropath ID NPID 4. Sex NPSEX 1 Male (CHECK ONE) 2 Female 5. Age at death NPDAGE years 6. Date of death (MM/ DD/ YYYY) NPDODMO / NPDODDY / NPDODYR 7. Postmortem interval (PMI): time between death . hours (99.9 = unknown) and brain removal NPPMIH 8. Fixative NPFIX 1 Formalin 2 Paraformaldehyde 7 Other (SPECIFY): NPFIXX 9. GROSS FINDINGS a. Whole brain weight (if half brain, multiply grams (9999 = unknown) weight by two) NPWBRWT b. Does the value in Question 9a represent 1 Fresh 2 Fixed 8 Not applicable fresh or fixed weight? (CHECK ONE) NPWBRF c. Severity of gross findings Not Missing/ (CHECK ONE BOX PER ROW) None Mild Moderate Severe assessed unknown 1. Cerebral cortex atrophy NPGRCCA 0 1 2 3 8 9 Lobar atrophy (significant frontal and/or 2. 0 1 Yes 8 9 temporal atrophy) NPGRLA 3. Hippocampus atrophy NPGRHA 0 1 2 3 8 9 4. Substantia nigra hypopigmentation NPGRSNH 1 2 3 8 9 5. L. ceruleus hypopigmentation NPGRLCH 0 1 2 3 8 9 6. Atherosclerosis (of the circle of Willis) NPAVAS 1 2 3 8 9 Copyright© 2006, 2008, 2014 University of Washington. Created and published by the Neuropathology Steering ommittee of the ADC Program and the National Alzheimer’s Coordinating Center (Walter A. Kukull, PhD, Director). All rights reserved. This publication was funded by the National Institutes of Health through the National Institute on Aging (Cooperative Agreement U01 AG016976). -

Identification of Genetic Modifiers in Hereditary Spastic Paraplegias Due to SPAST/SPG4 Mutations Livia Parodi
Identification of genetic modifiers in Hereditary Spastic Paraplegias due to SPAST/SPG4 mutations Livia Parodi To cite this version: Livia Parodi. Identification of genetic modifiers in Hereditary Spastic Paraplegias due to SPAST/SPG4 mutations. Human health and pathology. Sorbonne Université, 2019. English. NNT : 2019SORUS317. tel-03141229 HAL Id: tel-03141229 https://tel.archives-ouvertes.fr/tel-03141229 Submitted on 15 Feb 2021 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Sorbonne Université Institut du Cerveau et de la Moelle Épinière École Doctorale Cerveau-Cognition-Comportement Thèse de doctorat en Neurosciences Identification of genetic modifiers in Hereditary Spastic Paraplegias due to SPAST/SPG4 mutations Soutenue le 9 octobre 2019 par Livia Parodi Membres du jury : Pr Bruno Stankoff Président Pr Lesley Jones Rapporteur Dr Susanne de Bot Rapporteur Pr Christel Depienne Examinateur Pr Cyril Goizet Examinateur Pr Alexandra Durr Directeur de thèse Table of contents Abbreviations _________________________________________________________ -

And Α-Synuclein Pathology in a Case of Hereditary Spastic Paraplegia SPG7 with an Ala510val Mutation
Int. J. Mol. Sci. 2015, 16, 25050-25066; doi:10.3390/ijms161025050 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Article Abnormal Paraplegin Expression in Swollen Neurites, τ- and α-Synuclein Pathology in a Case of Hereditary Spastic Paraplegia SPG7 with an Ala510Val Mutation Dietmar R. Thal 1,2,*, Stephan Züchner 3,4, Stephan Gierer 5, Claudia Schulte 6,7, Ludger Schöls 6,7, Rebecca Schüle 3,6,7,† and Matthis Synofzik 5,6,†,* 1 Laboratory of Neuropathology—Institute of Pathology, Center of Clinical Research, University of Ulm, Helmholtzstraße 8/1, D-89081 Ulm, Germany 2 Department of Neuroscience, Katholieke Universiteit Leuven, B-3000 Leuven, Belgium 3 Dr. John T. Macdonald Foundation Department of Human Genetics University of Miami Miller School of Medicine, Miami, FL 33136, USA; E-Mails: [email protected] (S.Z.); [email protected] (R.S.) 4 John P. Hussman Institute for Human Genomics, University of Miami Miller School of Medicine, Miami, FL 33136, USA 5 Outpatient Praxis for Neurology, D-89407 Dillingen, Germany; E-Mail: [email protected] 6 Department of Neurodegenerative Diseases, Hertie-Institute for Clinical Brain Research, Hoppe-Seyler-Strasse 3, University of Tübingen, 72077 Tübingen, Germany; E-Mails: [email protected] (C.S.); [email protected] (L.S.) 7 German Research Center for Neurodegenerative Diseases (DZNE), University of Tübingen, 72076 Tuebingen, Germany † These authors contributed equally to this work. * Authors to whom correspondence should be addressed; E-Mails: [email protected] (D.R.T.); [email protected] (M.S.); Tel.: +32-16-3-44047 (D.R.T); +49-7071-298-2060 (M.S.); Fax: +32-16-3-36548 (D.R.T); +49-7071-2925-0001 (M.S.). -

Alzheimer Disease and Hereditary Spastic Paraplegia Hans Zempel1,3* and Eva-Maria Mandelkow1,2,3*
Zempel and Mandelkow Molecular Neurodegeneration (2015) 10:68 DOI 10.1186/s13024-015-0064-1 REVIEW Open Access Tau missorting and spastin-induced microtubule disruption in neurodegeneration: Alzheimer Disease and Hereditary Spastic Paraplegia Hans Zempel1,3* and Eva-Maria Mandelkow1,2,3* Abstract In Alzheimer Disease (AD), the mechanistic connection of the two major pathological hallmarks, namely deposition of Amyloid-beta (Aβ) in the form of extracellular plaques, and the pathological changes of the intracellular protein Tau (such as phosphorylation, missorting, aggregation), is not well understood. Genetic evidence from AD and Down Syndrome (Trisomy 21), and animal models thereof, suggests that aberrant production of Aβ is upstream of Tau aggregation, but also points to Tau as a critical effector in the pathological process. Yet, the cascade of events leading from increased levels of Aβ to Tau-dependent toxicity remains a matter of debate. Using primary neurons exposed to oligomeric forms of Aβ, we have found that Tau becomes mislocalized (missorted) into the somatodendritic compartment. Missorting of Tau correlates with loss of microtubules and downstream consequences such as loss of mature spines, loss of synaptic activity, and mislocalization of mitochondria. In this cascade, missorting of Tau induces mislocalization of TTLL6 (Tubulin-Tyrosine-Ligase-Like 6) into the dendrites. TTLL6 induces polyglutamylation of microtubules, which acts as a trigger for spastin mediated severing of dendritic microtubules. Loss of microtubules makes cells unable to maintain transport of mitochondria, which in turn results in synaptic dysfunction and loss of mature spines. These pathological changes are absent in TauKO derived primary neurons. Thus, Tau mediated mislocalization of TTLL6 and spastin activation reveals a pathological gain of function for Tau and spastin in this cellular model system of AD. -

No Metagenomic Evidence of Causative Viral Pathogens in Postencephalitic Parkinsonism Following Encephalitis Lethargica
microorganisms Communication No Metagenomic Evidence of Causative Viral Pathogens in Postencephalitic Parkinsonism Following Encephalitis Lethargica Dániel Cadar 1 , Kurt A. Jellinger 2, Peter Riederer 3, Sabrina Strobel 4, Camelia-Maria Monoranu 4 and Dennis Tappe 1,* 1 Bernhard Nocht Institute for Tropical Medicine, 20359 Hamburg, Germany; [email protected] 2 Institute of Clinical Neurobiology, 1090 Vienna, Austria; [email protected] 3 Center of Mental Health, Department of Psychiatry, Psychosomatics and Psychotherapy, University Hospital of Würzburg, 97080 Würzburg, Germany; [email protected] 4 Department of Neuropathology, Institute for Pathology, University of Würzburg, 97080 Würzburg, Germany; [email protected] (S.S.); [email protected] (C.-M.M.) * Correspondence: [email protected] Abstract: Postencephalitic parkinsonism (PEP) is a disease of unknown etiology and pathophysiol- ogy following encephalitis lethargica (EL), an acute-onset polioencephalitis of cryptic cause in the 1920s. PEP is a tauopathy with multisystem neuronal loss and gliosis, clinically characterized by bradykinesia, rigidity, rest tremor, and oculogyric crises. Though a viral cause of EL is likely, past polymerase chain reaction-based investigations in the etiology of both PEP and EL were negative. PEP might be caused directly by an unknown viral pathogen or the consequence of a post-infectious im- munopathology. The development of metagenomic next-generation sequencing in conjunction with Citation: Cadar, D.; Jellinger, K.A.; bioinformatic techniques has generated a broad-range tool for the detection of unknown pathogens Riederer, P.; Strobel, S.; Monoranu, C.-M.; Tappe, D. No Metagenomic in the recent past. Retrospective identification and characterization of pathogens responsible for past Evidence of Causative Viral infectious diseases can be successfully performed with formalin-fixed paraffin-embedded (FFPE) Pathogens in Postencephalitic tissue samples.