Co-Morbidity of Progressive Supranuclear
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thalamohippocampal Atrophy in Focal Epilepsy of Unknown Cause at the Time of Diagnosis
medRxiv preprint doi: https://doi.org/10.1101/2020.07.24.20159368; this version posted July 25, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-ND 4.0 International license . Thalamohippocampal atrophy in focal epilepsy of unknown cause at the time of diagnosis Nicola J. Leek1, Barbara A. K. Kreilkamp1,2, Mollie Neason1, Christophe de Bezenac1, Besa Ziso2, Samia Elkommos3, Kumar Das2, Anthony G. Marson1,2, Simon S. Keller1,2* 1Department of Pharmacology and Therapeutics, Institute of Systems, Molecular and Integrative Biology, University of Liverpool, UK 2The Walton Centre NHS Foundation Trust, Liverpool, UK 3St George’s University Hospitals NHS Foundation Trust, London, UK *Corresponding author Dr Simon Keller Clinical Sciences Centre Aintree University Hospital Lower Lane Liverpool L9 7LJ [email protected] Keywords: Newly diagnosed epilepsy, focal epilepsy, thalamus, hippocampus, treatment outcome NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. 1 medRxiv preprint doi: https://doi.org/10.1101/2020.07.24.20159368; this version posted July 25, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-ND 4.0 International license . Abstract Background: Patients with chronic focal epilepsy may have atrophy of brain structures important for the generation and maintenance of seizures. -

Pathologic Thr175 Tau Phosphorylation in CTE and CTE with ALS
Published Ahead of Print on January 3, 2018 as 10.1212/WNL.0000000000004899 ARTICLE OPEN ACCESS Pathologic Thr175 tau phosphorylation in CTE and CTE with ALS Alexander J. Moszczynski, PhD, Wendy Strong, BSc, Kathy Xu, MSc, Ann McKee, MD, Arthur Brown, PhD, Correspondence and Michael J. Strong, MD Dr. M.J. Strong [email protected] Neurology® 2018;90:e1-8. doi:10.1212/WNL.0000000000004899 Abstract Objective To investigate whether chronic traumatic encephalopathy (CTE) and CTE with amyotrophic lateral sclerosis (CTE-ALS) exhibit features previously observed in other tauopathies of pathologic phosphorylation of microtubule-associated protein tau at Thr175 (pThr175 tau) and Thr231 (pThr231 tau), and glycogen synthase kinase–3β (GSK3β) activation, and whether these pathologic features are a consequence of traumatic brain injury (TBI). Methods Tau isoform expression was assayed by western blot in 6 stage III CTE cases. We also used immunohistochemistry to analyze 5 cases each of CTE, CTE-ALS, and 5 controls for ex- pression of activated GSK3β, pThr175 tau, pThr231 tau, and oligomerized tau within spinal cord tissue and hippocampus. Using a rat model of moderate TBI, we assessed tau pathology and phospho-GSK3β expression at 3 months postinjury. Results CTE and CTE-ALS are characterized by the presence of all 6 tau isoforms in both soluble and insoluble tau isolates. Activated GSK3β, pThr175 tau, pThr231 tau, and oligomerized tau protein expression was observed in hippocampal neurons and spinal motor neurons. We observed tau neuronal pathology (fibrillar inclusions and axonal damage) and increased levels of pThr175 tau and activated GSK3β in moderate TBI rats. Conclusions Pathologic phosphorylation of tau at Thr175 and Thr231 and activation of GSK3β are features of the tauopathy of CTE and CTE-ALS. -

Immune Effector Mechanisms and Designer Vaccines Stewart Sell Wadsworth Center, New York State Department of Health, Empire State Plaza, Albany, NY, USA
EXPERT REVIEW OF VACCINES https://doi.org/10.1080/14760584.2019.1674144 REVIEW How vaccines work: immune effector mechanisms and designer vaccines Stewart Sell Wadsworth Center, New York State Department of Health, Empire State Plaza, Albany, NY, USA ABSTRACT ARTICLE HISTORY Introduction: Three major advances have led to increase in length and quality of human life: Received 6 June 2019 increased food production, improved sanitation and induction of specific adaptive immune Accepted 25 September 2019 responses to infectious agents (vaccination). Which has had the most impact is subject to debate. KEYWORDS The number and variety of infections agents and the mechanisms that they have evolved to allow Vaccines; immune effector them to colonize humans remained mysterious and confusing until the last 50 years. Since then mechanisms; toxin science has developed complex and largely successful ways to immunize against many of these neutralization; receptor infections. blockade; anaphylactic Areas covered: Six specific immune defense mechanisms have been identified. neutralization, cytolytic, reactions; antibody- immune complex, anaphylactic, T-cytotoxicity, and delayed hypersensitivity. The role of each of these mediated cytolysis; immune immune effector mechanisms in immune responses induced by vaccination against specific infectious complex reactions; T-cell- mediated cytotoxicity; agents is the subject of this review. delayed hypersensitivity Expertopinion: In the past development of specific vaccines for infections agents was largely by trial and error. With an understanding of the natural history of an infection and the effective immune response to it, one can select the method of vaccination that will elicit the appropriate immune effector mechanisms (designer vaccines). These may act to prevent infection (prevention) or eliminate an established on ongoing infection (therapeutic). -

Investigation of Anti-Iglon5-Induced Neurodegenerative Changes in Human Neurons
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.27.269795; this version posted August 28, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Manuscript BioRxiv Investigation of anti-IgLON5-induced neurodegenerative changes in human neurons Mattias Gamre1,2, Matias Ryding1,2, Mette Scheller Nissen1,2,3, Anna Christine Nilsson4, Morten Meyer1,2,5, Morten Blaabjerg1,2,3,5 1Neurobiological Research, Institute of Molecular Medicine, University of Southern Denmark, Odense, Denmark. 2Department of Neurology, Odense University Hospital, Odense, Odense, Denmark 3Department of Clinical Research, Odense University Hospital, Odense, Denmark 4Department of Clinical Immunology, Odense University Hospital, Odense, Denmark 5BRIDGE – Brain Research Inter-Disciplinary Guided Excellence, Department of Clinical Research, University of Southern Denmark, Odense, Denmark Number of pages: 12 Number of figures: 4 Keywords: IgLON5, Autoimmune encephalitis, neurodegeneration, inflammation, Tau Corresponding author Professor Morten Blaabjerg, MD, PhD Department of Neurology Odense University Hospital J.B. Winsløws Vej 4 5000 Odense C Denmark Phone: (+45) 6541 2457 E-mail: [email protected] Page 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.27.269795; this version posted August 28, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. -

Neuropathological Studies of Patients with Possible Non-Herpetic Acute Limbic Encephalitis and So-Called Acute Juvenile Female Non-Herpetic Encephalitis
□ ORIGINAL ARTICLE □ Neuropathological Studies of Patients with Possible Non-Herpetic Acute Limbic Encephalitis and So-called Acute Juvenile Female Non-Herpetic Encephalitis Koichi Okamoto 1, Tsuneo Yamazaki 1, Haruhiko Banno 2,GenSobue2, Mari Yoshida 3 and Masamitsu Takatama 4 Abstract Objective This study was to clarify the neuropathological findings of non-herpetic acute limbic encephalitis (NHALE) and so-called acute juvenile female non-herpetic encephalitis (AJFNHE). Methods We examined three rare autopsied cases consisting of probable one NHALE and two AJFNHLE. For comparison, we also studied 10 autopsied cases of hippocampal sclerosis mainly caused by anoxia. Results In NHALE, neuronal loss with gliosis and microglia/macrophage infiltrations were mainly seen in the CA1 areas in the hippocampus. However, there were no apparent anoxic neuronal changes in the remain- ing neurons in the CA1, and astrocyte proliferations and microglia/macrophage infiltrations were also ob- served in the claustrum, while these were mildly present in the basal ganglia. In AJFNHE, pathological find- ings differed from those of NHALE with regard of the absence of limited pathology in the limbic system, microglia/macrophages widely infiltrated the brain including the hippocampal areas and mild lymphocytic in- filtrations were observed in the subarachnoid spaces as well as in the parenchyma. Conclusions The pathomechanism of NHALE and AJFNHE is obscure and autoimmune theory is pro- posed, however we must collect and examine many autopsied cases in order to clarify the pathomechanism. Key words: non-herpetic acute limbic encephalitis, acute juvenile female non-herpetic encephalitis, hip- pocampal sclerosis (DOI: 10.2169/internalmedicine.47.0547) (7, 8, 10, 11). -

Control of Epileptic Seizures by the Basal Ganglia: Clinical and Experimental Approaches Feddersen Berend
Control of epileptic seizures by the basal ganglia: clinical and experimental approaches Feddersen Berend To cite this version: Feddersen Berend. Control of epileptic seizures by the basal ganglia: clinical and experimental ap- proaches. Neurons and Cognition [q-bio.NC]. Université Joseph-Fourier - Grenoble I, 2009. English. tel-00413972 HAL Id: tel-00413972 https://tel.archives-ouvertes.fr/tel-00413972 Submitted on 7 Sep 2009 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Ecole Doctorale Chimie et Sciences du Vivant UNIVERSITE JOSEPH FOURIER GRENOBLE Thèse Neuroscience - Neurobiologie Berend Feddersen Control of epileptic seizures by the basal ganglia: clinical and experimental approaches Soutenue publiquement le: 10.07.2009 Membres du jury : Franck Semah (Rapporteur 1) Stephane Charpier (Rapporteur 2) Philippe Kahane Soheyl Noachtar Antoine Depaulis (Directeur de thèse) Colin Deransart 1 ACKNOWLEDGEMENTS Many fantastic people were inolved in this thesis, whom I want to thank deeply for all their help and support. I want to thank my supervisors Soheyl Noachtar, Antoine Depaulis and Colin Deransart for all their help and fruitfull discussions in every kind of situation. Sohyel Nochtar teached me in a perfect structured manner clinical epileptology and gave me always all the support I needed, especially for my stay in Grenoble. -

Alterations of Hippocampal Acetylcholinesterase in Human
Alterations of H~ppocampal Acetylcholmesterase in Human Temporal bbe Epilepsy Robert C. Green, MD,X Howard W. Blume, MD, PhD,? Seth B. Kupferschmid, MS," and M-Marsel Mesulam, MD" Hippocampal sclerosis is the most common pathological finding associated with human temporal lobe epilepsy. His- tochemical study with acetylcholinesterase (AChE) staining was used to investigate 7 surgically resected temporal lobes with hippocampal sclerosis from patients with temporal lobe epilepsy. In all 7 specimens, an abnormal but consistent pattern of staining was noted. In the hilum of the dentate gyrus, AChE-rich polymorphic cells were relatively preserved in comparison to the pyramidal neurons. In Ammon's horn, AChE fibers were lost in regions corresponding to the pyramidal cell dropout. AChE fibers were also lost along the inner portion of the molecular layer of the dentate gyrus, yet they were preserved within the outer portions of the molecular layer. These findings provide additional evidence for the relative selectivity of hippocampal pathology in human temporal lobe epilepsy. Green RC, Blume HW, Kupferschmid SB, Mesulam M-M. Alterations of hippocampal acetylcholinesterasein human temporal lobe epilepsy. Ann Neurol 1989;26:347-351 A common form of human epilepsy is partial epilepsy and the resulting reorganization of neural connectivity of temporolimbic origin (TLE). Surgical resection of could contribute to the complex behavioral alterations the anterior temporal lobe is commonly used to treat observed in some patients with TLE Ell]. TLE patients whose seizures are intractable to anticon- The morphological alterations in hippocampal scle- vulsant medication 11-31. The resected tissue some- rosis have been described in great detail. -

An Autopsy Case of Progressive Supranuclear Palsy with Incidental
Letters Discussion | This pilot study successfully explored the effect size 3. Korte J-M, Kaila T, Saari KM. Systemic bioavailability and cardiopulmonary of timolol eyedrops on migraine headaches. Several partici- effects of 0.5% timolol eyedrops. Graefes Arch Clin Exp Ophthalmol. 2002;240 (6):430-435. pants responded extremely well to the timolol. Further re- 4. Migliazzo CV, Hagan JC III. Beta blocker eyedrops for treatment of acute search is needed to determine what patient factors might pre- migraine. Mo Med. 2014;111(4):283-288. dict responsiveness to timolol. 5. Chiam PJT. Topical beta-blocker treatment for migraine. Int Ophthalmol. 2012; 32(1):85-88. Limitations. Study limitations include a small sample size, a 6. Headache Classification Committee of the International Headache Society. lack of investigator masking, and an imperfect placebo, as The international classification of headache disorders, 3rd edition (beta artificial tears tend to cause less of a burning sensation than version). https://www.ichd-3.org/wp-content/uploads/2016/08/International -Headache-Classification-III-ICHD-III-2013-Beta-1.pdf. Accessed June 1, 2016. timolol. With a half-life of 4 hours, timolol ophthalmic is unlikely to have had an association with repeated head- aches or beyond the 3-day washout period. Four 50-μL drops of timolol, 0.5%, represent 1 mg of timolol, which An Autopsy Case of Progressive Supranuclear compares with an oral prophylactic dosage of 10 to 30 mg of Palsy With Incidental ATXN2 Expansion timolol daily. Future research should aim for a target enroll- A case of multiple system atrophy with predominant parkin- ment of more than 86 participants and explore optimal dos- sonism (MSA-P) with ATXN2 (OMIM 601517) expansion was ing regimens. -

Hippocampal Sclerosis: Causes and Prevention
193 Hippocampal Sclerosis: Causes and Prevention Matthew Charles Walker, FRCP, PhD1 1 Department of Clinical and Experimental Epilepsy, UCL Institute of Address for correspondence Matthew Charles Walker, FRCP, PhD, Neurology, University College London, London, United Kingdom Department of Clinical and Experimental Epilepsy, UCL Institute of Neurology, University College London, Queen Square, London WC1N Semin Neurol 2015;35:193–200. 3BG, United Kingdom (e-mail: [email protected]). Abstract Hippocampal sclerosis is the commonest cause of drug-resistant epilepsy in adults, and is associated with alterations to structures and networks beyond the hippocampus. In addition to being a cause of epilepsy, the hippocampus is vulnerable to damage from seizure activity. In particular, prolonged seizures (status epilepticus) can result in hippocampal sclerosis. The hippocampus is also vulnerable to other insults including traumatic brain injury, and inflammation. Hippocampal sclerosis can occur in associa- tion with other brain lesions; the prevailing view is that it is probably a secondary consequence. In such instances, successful surgical treatment usually involves the resection of both the lesion and the involved hippocampus. Experimental data have pointed to numerous neuroprotective strategies to prevent hippocampal sclerosis. Initial neuroprotective strategies aimed at glutamate receptors may be effective, but later, metabolic pathways, apoptosis, reactive oxygen species, and inflammation are involved, perhaps necessitating the use of interventions aimed at Keywords multiple targets. ► hippocampal sclerosis Some of the therapies that we use to treat status epilepticus may neuroprotect. ► status epileptics However, prevention of neuronal death does not necessarily prevent the later develop- ► epilepsy ment of epilepsy or cognitive deficits. Perhaps, the most important intervention is the ► neuroprotection early, aggressive treatment of seizure activity, and the prevention of prolonged seizures. -
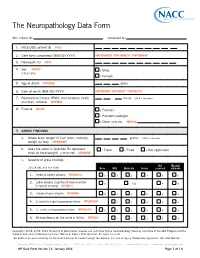
The Neuropathology Data Form
The Neuropathology Data Form ADC subject ID: Completed by: 1. MDS/UDS patient ID PTID 2. Date form completed (MM/DD/ YYYY) NPFORMMO / NPFORMDY / NPFORMYR 3. Neuropath ID NPID 4. Sex NPSEX 1 Male (CHECK ONE) 2 Female 5. Age at death NPDAGE years 6. Date of death (MM/ DD/ YYYY) NPDODMO / NPDODDY / NPDODYR 7. Postmortem interval (PMI): time between death . hours (99.9 = unknown) and brain removal NPPMIH 8. Fixative NPFIX 1 Formalin 2 Paraformaldehyde 7 Other (SPECIFY): NPFIXX 9. GROSS FINDINGS a. Whole brain weight (if half brain, multiply grams (9999 = unknown) weight by two) NPWBRWT b. Does the value in Question 9a represent 1 Fresh 2 Fixed 8 Not applicable fresh or fixed weight? (CHECK ONE) NPWBRF c. Severity of gross findings Not Missing/ (CHECK ONE BOX PER ROW) None Mild Moderate Severe assessed unknown 1. Cerebral cortex atrophy NPGRCCA 0 1 2 3 8 9 Lobar atrophy (significant frontal and/or 2. 0 1 Yes 8 9 temporal atrophy) NPGRLA 3. Hippocampus atrophy NPGRHA 0 1 2 3 8 9 4. Substantia nigra hypopigmentation NPGRSNH 1 2 3 8 9 5. L. ceruleus hypopigmentation NPGRLCH 0 1 2 3 8 9 6. Atherosclerosis (of the circle of Willis) NPAVAS 1 2 3 8 9 Copyright© 2006, 2008, 2014 University of Washington. Created and published by the Neuropathology Steering ommittee of the ADC Program and the National Alzheimer’s Coordinating Center (Walter A. Kukull, PhD, Director). All rights reserved. This publication was funded by the National Institutes of Health through the National Institute on Aging (Cooperative Agreement U01 AG016976). -

Identification of Genetic Modifiers in Hereditary Spastic Paraplegias Due to SPAST/SPG4 Mutations Livia Parodi
Identification of genetic modifiers in Hereditary Spastic Paraplegias due to SPAST/SPG4 mutations Livia Parodi To cite this version: Livia Parodi. Identification of genetic modifiers in Hereditary Spastic Paraplegias due to SPAST/SPG4 mutations. Human health and pathology. Sorbonne Université, 2019. English. NNT : 2019SORUS317. tel-03141229 HAL Id: tel-03141229 https://tel.archives-ouvertes.fr/tel-03141229 Submitted on 15 Feb 2021 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Sorbonne Université Institut du Cerveau et de la Moelle Épinière École Doctorale Cerveau-Cognition-Comportement Thèse de doctorat en Neurosciences Identification of genetic modifiers in Hereditary Spastic Paraplegias due to SPAST/SPG4 mutations Soutenue le 9 octobre 2019 par Livia Parodi Membres du jury : Pr Bruno Stankoff Président Pr Lesley Jones Rapporteur Dr Susanne de Bot Rapporteur Pr Christel Depienne Examinateur Pr Cyril Goizet Examinateur Pr Alexandra Durr Directeur de thèse Table of contents Abbreviations _________________________________________________________ -

And Α-Synuclein Pathology in a Case of Hereditary Spastic Paraplegia SPG7 with an Ala510val Mutation
Int. J. Mol. Sci. 2015, 16, 25050-25066; doi:10.3390/ijms161025050 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Article Abnormal Paraplegin Expression in Swollen Neurites, τ- and α-Synuclein Pathology in a Case of Hereditary Spastic Paraplegia SPG7 with an Ala510Val Mutation Dietmar R. Thal 1,2,*, Stephan Züchner 3,4, Stephan Gierer 5, Claudia Schulte 6,7, Ludger Schöls 6,7, Rebecca Schüle 3,6,7,† and Matthis Synofzik 5,6,†,* 1 Laboratory of Neuropathology—Institute of Pathology, Center of Clinical Research, University of Ulm, Helmholtzstraße 8/1, D-89081 Ulm, Germany 2 Department of Neuroscience, Katholieke Universiteit Leuven, B-3000 Leuven, Belgium 3 Dr. John T. Macdonald Foundation Department of Human Genetics University of Miami Miller School of Medicine, Miami, FL 33136, USA; E-Mails: [email protected] (S.Z.); [email protected] (R.S.) 4 John P. Hussman Institute for Human Genomics, University of Miami Miller School of Medicine, Miami, FL 33136, USA 5 Outpatient Praxis for Neurology, D-89407 Dillingen, Germany; E-Mail: [email protected] 6 Department of Neurodegenerative Diseases, Hertie-Institute for Clinical Brain Research, Hoppe-Seyler-Strasse 3, University of Tübingen, 72077 Tübingen, Germany; E-Mails: [email protected] (C.S.); [email protected] (L.S.) 7 German Research Center for Neurodegenerative Diseases (DZNE), University of Tübingen, 72076 Tuebingen, Germany † These authors contributed equally to this work. * Authors to whom correspondence should be addressed; E-Mails: [email protected] (D.R.T.); [email protected] (M.S.); Tel.: +32-16-3-44047 (D.R.T); +49-7071-298-2060 (M.S.); Fax: +32-16-3-36548 (D.R.T); +49-7071-2925-0001 (M.S.).