Characterization of Call Prioritization Time in a Medical Priority Dispatch
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

EMS Industry Trends | Cyber Liability | Employment Law Legislation
EMS Industry Trends | Cyber Liability | Employment Law Legislation S UMMER 2014 2014 Stars of Life Recipients | Annual Convention Plans Find out why others have trusted the Multi-Grip since 1989. The Multi-Grip was designed by a fire-fighter in 1989. Today this effective CID is used across the US as well as in other countries. It comes in three sizes: adult, child and pediatric. This is a complete system for your head immobilization needs. Its design makes it a universal head immobilizer appropriate for a variety of situations. Based on a truss system, the Multi-Grip maintains superior strength, and any patient movement will tighten the straps to create the ultimate immobilization. It’s simple and it works. Home of the Tank Boss Portable O2 Cylinder Lift Manufacturing Find out why others have trusted the Multi-Grip since 1989. The Multi-Grip was designed by a fire-fighter in 1989. Today this effective CID is used across the US as well as in other countries. It comes in three sizes: adult, child and pediatric. This is a complete system for your head immobilization needs. Its design makes it a universal head immobilizer appropriate for a variety of situations. Based on a truss system, the Multi-Grip maintains superior strength, and any patient movement will tighten the straps to create the ultimate immobilization. It’s simple and it works. Home of the Tank Boss Portable O2 Cylinder Lift Manufacturing S UMMER 2014 CAA Vision Assure delivery of excellent pre-hospital care to the people of California by promoting recognized industry best practices. -

Evidence-Based Performance Measures for Emergency Medical Services Systems:Amodel for Expanded Ems Benchmarking Astatement Developed by the 2007 Consortium U.S
SPECIAL CONTRIBUTIONS EVIDENCE-BASED PERFORMANCE MEASURES FOR EMERGENCY MEDICAL SERVICES SYSTEMS:AMODEL FOR EXPANDED EMS BENCHMARKING ASTATEMENT DEVELOPED BY THE 2007 CONSORTIUM U.S. METROPOLITAN MUNICIPALITIES’ EMS MEDICAL DIRECTORS (APPENDIX) J. Brent Myers, MD, MPH, Corey M. Slovis, MD, Marc Eckstein, MD, MPH, Jeffrey M. Goodloe, MD, S. Marshal Isaacs, MD, James R. Loflin, MD, C. Crawford Mechem, MD, Neal J. Richmond, MD, Paul E. Pepe, MD, MPH ABSTRACT INTRODUCTION There are few evidence-based measures of emergency medi- Evidence-based clinical measures of emergency med- cal services (EMS) system performance. In many jurisdictions, ical services (EMS) system performance have been response-time intervals for advanced life support units and few in number, largely due to the limited quantity resuscitation rates for victims of cardiac arrest are the pri- and quality of research committed to the prehospital mary measures of EMS system performance. The association arena.1−4 Although there is a 9-1-1 call for EMS of the former with patient outcomes is not supported explic- response every other second in the United States, itly by the medical literature, while the latter focuses on a very and despite the fact that survival from various acute small proportion of the EMS patient population and thus does not represent a sufficiently broad selection of patients. While illnesses and injuries are determined in that prehos- For personal use only. these metrics have their place in performance measurement, pital setting, evidence for out-of-hospital emergency 1−3 a more robust method to measure and benchmark EMS per- care procedures are clearly lacking. -

EMCC Workshop Literature October, 2013 a Compilation of Evidence‐Based and Best Practice Literature on Emergency Medical Services
Contra Costa Emergency Medical Services EMS System Modernization Study conducted by Fitch and Associates EMCC Workshop Literature October, 2013 A compilation of evidence‐based and best practice literature on Emergency Medical Services ADESCRIPTIVE STUDY OF THE “LIFT-ASSIST”CALL David C. Cone, MD, John Ahern, Christopher H. Lee, MD, MS, Dorothy Baker, PhD, Terrence Murphy, PhD, Sandy Bogucki, MD, PhD ABSTRACT evaluation. Key words: emergency medical services; geri- atrics; accidental falls Introduction. Responses for “lift assists” (LAs) are common in many emergency medical services (EMS) systems, and PREHOSPITAL EMERGENCY CARE 2013;17:51–56 result when a person dials 9-1-1 because of an inability to get up, is subsequently determined to be uninjured, and NTRODUCTION is not transported for further medical attention. Although I LAs often involve recurrent calls and are generally not reim- When elderly or disabled persons fall or are unable bursable, little is known of their operational effects on EMS to move from an undesirable position to a preferred systems. We hypothesized that LAs present an opportunity one, they may call 9-1-1 for assistance. Often there is for earlier treatment of subtle-onset medical conditions and no perceived injury or illness, so these individuals do injury prevention interventions in a population at high risk not want medical treatment or transport to the hospi- for falls. Objectives. To quantify LA calls in one community, describe EMS returns to the same address within 30 days tal. They simply want responders to physically help following an index LA call, and characterize utilization of them back to a bed, chair, or wheelchair. -
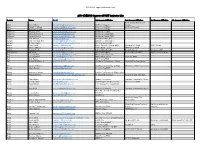
2018 KYEMSC Approved PAHT Instructor List
2017 PAHT Approved Instructor List 2018 KYEMSC Approved PAHT Instructor List County Name Email 1st Agency Affiliation 2nd Agency Affiliation 3rd Agency Affiliation 4th Agency Affiliation Adair County Ambulance Adair Donald Hare [email protected] Air Evac Lifeteam Service Adair Joseph C Wheet [email protected] Adair County EMS Air Evac Lifeteam Adair Thomas P Gaskin [email protected] Adair County EMS Anderson Amanda Short [email protected] Anderson Co EMS Anderson Amanda Womack [email protected] Anderson County EMS Anderson Susan Johnson [email protected] Anderson County EMS Ballard Jack Glisson [email protected] Ballard County EMS Ballard James P. Garrett II [email protected] Ballard Co. Ambulance Ballard Michael Clarke [email protected] Mercy Regional EMS Barren Kevin Jandt [email protected] Barren Metcalfe County EMS Glasgow Fire Dept SFRT Area4 Barren Ronnie Stinson [email protected] Park City Fire Dept SFRT Area 4 064 Barren Sammy Stotts [email protected] Barren Metcalfe EMS KCTCS Area 4 Green Co. EMS Barren/Allen Bill Milan [email protected] Allen County EMS Barren-Metcalfe EMS WKU Kemsa program Bell Dan Sanders [email protected] Middlesboro Fire Dept. Bell Gregory Fultz [email protected] SECC Middlesboro Claiborne EMS Bell Josh Peters [email protected] Bell County EMS Bell Robert M Wilson Jr [email protected] Southeast Community College Pineville Fire Department Bell Steven Robinson [email protected] Southeast Community College Middlesboro Fire Department Boone Adam Begley [email protected] Florence Fire/EMS Boone Anthony Scheben [email protected] Hebron Fire Protection District #106 Boone Benjamin Riley [email protected]; [email protected] St. -
How Data & Technology Are Revolutionizing Patient Care
MAY2015 How data & technology are revolutionizing patient care An exclusive editorial supplement to JEMS, sponsored by ZOLL, FirstWatch, ImageTrend and Physio-Control Inc. Advancing Care with Data-driven Solutions COORDINATING FIRST RESPONSE DELIVERING THE GOLD STANDARD FROM DISPATCH TO PATIENT CARE IN MONITORING AND TREATMENT RescueNet® Dispatch, Navigator, and Road Safety RescueNet ePCR, EMS Mobile Health X Series® Monitor/Defibrillator AutoPulse® and X Series Monitor/Defibrillator CONNECTING PROVIDERS IMPROVING BUSINESS PROCESS TO EXPEDITE CARE TO DRIVE EFFICIENCY EMS Mobile Health RescueNet Billing, Resource Planner, and Crew Scheduler RescueNet 12-Lead RescueNet FireRMS and Insight Analytics Learn more at www.zoll.com/realtimedata © 2013 ZOLL Medical Corporation. All rights reserved. AutoPulse, RescueNet, X Series and ZOLL are trademarks or registered trademarks of ZOLL Medical Corporation in the United States and/or other countries. All other trademarks are the property of their respective owners. Zoll_JEMSsupp_1505 1 3/24/15 8:37 AM •contents• •introduction• 2 By Greg Mears, MD The Star Trek Tricorder In some way, each of us grew up with Star Trek—the original TV Still a vision of the not-so-distant future series, The Next Generation or the current prequels. We marveled at By Alan Craig the ability to “beam me up” using the transporter, or using the medi- cal tricorder to diagnose the ill. Star Trek creator Gene Roddenberry’s 6 imagination and vision raised everyone’s awareness of the value of Next Generation 9-1-1 technology—for EMS it raised expectations of how easy it should be I texted 9-1-1 & was resuscitated to use and integrate into our everyday lives. -

EMS Directory- Teis
Kentucky Licensure EMS Directory- TEIs Service Name Service Service Service Service Service Service Service City Service Service Service Service Service Service Service License Permit Level Phone Fax Street 1 Street 2 County State Postal Shipping Shipping Shipping Shipping Number Code Street 1 Street 2 County Postal Code Service Classification: EMS-TEI 1 Louisville Gas and Electric TEI-308 EDUCATIONAL 502- 502-364- 220 West Main LOUISVILLE JEFFERSON KY 40202 220 West Main JEFFERSON 40214 TEI INSTITUTION 627- 8330 Street Street 6118 Service Classification: EMS-TEI 2 ADAIR CO. AMBULANCE TEI-254 EDUCATIONAL 270- 270-384- 906 Columbia Adair KY 42728 PO BOX 549 Adair 42728 SERVICE TEI INSTITUTION 384- 5533 WESTLAKE 4706 DRIVE APPALACHIAN FIRST TEI-238 EDUCATIONAL 606- 606-353- 1477 POND Stone Pike KY 41567 1477 POND Pike 41567 RESPONSE EMERGENCY INSTITUTION 237- 9835 CREEK ROAD CREEK ROAD SERVICES TEI 5100 BAPTIST HEALTH TEI-029 EDUCATIONAL 270- 270-575- 2535 PADUCAH MCCRACKEN KY 42001 2535 MCCRACKEN 42001 OCCUPATIONAL MEDICINE INSTITUTION 575- 0418 BROADWAY BROADWAY TEI 3001 Campbell County Fire TEI-153 EDUCATIONAL 859- 859-635- 6844 FOUR Melbourne Campbell KY 41059 6844 FOUR Campbell 41059 District #1 TEI INSTITUTION 635- 0260 MILE ROAD MILE ROAD 9255 CITY OF PIKEVILLE FIRE & TEI-269 EDUCATIONAL 606- 606-437- 104 Chloe RD Pikeville Pike KY 41501 104 ChLoe RD Pike 41501 EMS TEI INSTITUTION 437- 5126 5120 CLINTON HICKMAN CO. TEI-264 EDUCATIONAL 270- 270-653- 324 James H Clinton Hickman KY 42031 PO BOX 83 Hickman 42031 AMBULANCE SERVICE TEI -

2019 Recognition Winners
2019 Recognition Winners The American Heart Association proudly recognizes the following EMS provider organizations that serve and/or jointly serve their community. Thank you for applying the most up-to-date evidence-based treatment guidelines to improve patient care and outcomes in the community you serve. STATE CITY AGENCY NAME 2019 AWARD Alabama Mobile City of Mobile Fire-Rescue Dept. Silver Plus Alabama Huntsville Huntsville Emergency Medical Services Inc. Gold Plus Medstar EMS Alabama Summerdale Team Members: Silver Medstar Air Care Alabama Tuscaloosa NorthStar EMS Gold Plus Air Methods Corporation, Pac-West Arizona Native Air, Arizona Mesa Gold Plus Life Net, TriState CareFlight Arizona Mesa Air Methods, Inc. Mercy Air Silver Plus Arizona Anthem Daisy Mountain Fire and Medical Gold Plus Arizona Glendale Glendale Fire Department Gold Plus Arizona Surprise Surprise Fire-Medical Department Gold Plus Williamson Valley-Bagdad Fire District Arizona Prescott Team Members: Silver Plus Lifeline Ambulance- Prescott Arkansas Forrest City Air-Evac Lifeteam Base 42 Forrest City AR Gold Plus Arkansas Bella Vista Bella Vista Fire/EMS Gold Plus Arkansas El Dorado ProMed Ambulance Bronze Plus Arkansas Marked Tree Riverside Ambulance INC Gold Arkansas Rogers Rogers Fire Department Bronze Plus 1 STATE CITY AGENCY NAME 2019 AWARD Arkansas Siloam Springs Siloam Springs Fire Department Gold Plus Arkansas Springdale Springdale Fire Department. Silver Plus Arkansas Fayetteville WCRAA- Central EMS Gold Plus California Santa Rosa American Medical Response -

911 Emergency Communication Nurse Triage Reduces EMS Patient
ORIGINAL RESEARCH 911 Emergency Communication Nurse Triage Reduces EMS Patient Costs and Directs Patients to High-Satisfaction Alternative Point of Care Isabel Gardett, PhD1; Greg Scott, MBA1; Jeff Clawson, MD1; Kristen Miller2; Neal Richmond, MD2; Comilla Sasson, MD3; Mat Zavadsky, MS4; Mark Rector1; Andrew Wilcox5; Chris Olola, PhD1 1. International Academies of Emergency ABSTRACT Dispatch (IAED), Salt Lake City, Utah, USA. Introduction: Recent estimates indicate that more than half of all Emergency Depart- 2. Louisville Metro EMS, Louisville, ment (ED) visits could be avoided, reducing patient costs and increasing satisfaction Kentucky, USA. with care. Since 911 is increasingly the Àrst point of contact for many patients enter- 3. University of Colorado, Denver, Colorado, USA. ing the health care system—even those with non-emergency conditions—one poten- 4. MedStar EMS-Mobile Health, Ft. tial approach to decreasing emergency costs and ED overcrowding is to reinvent the Worth, Texas, USA. 911 dispatch center as a clearinghouse for directing patients to alternative care pro- 5. Salt Lake City Fire Department, Salt viders. This study presents a cost avoidance analysis of two 911 dispatch centers that Lake City, Utah, USA. implemented such a service, the Emergency Communication Nurse System (ECNS). Correspondence: Objectives: The primary objectives were to determine the amount of cost avoid- Chris Olola, PhD ance realized by payers using the ECNS to send patients to alternative Ànal points International Academies of Emergency of care, and to identify the amount saved by transporting patients by alternative Dispatch 110 S Regent Street means an ambulance. The secondary objective was to quantify patients’ satisfaction Salt Lake City, UT 84070 with the service through analysis of patient follow-up survey data. -

Emergency Services 2017 Year End Report
Emergency Services 2017 Year End Report EDWARD J. MEIMAN III DIRECTOR Table of Contents THE REPORT 3 A Note from Our Director 16 Public Information 4 Executive Summary 17 Special Events 5 Who We Are 18 LEPC 6-7 Emergency Management 19-30 Appendix 8 LENSAlert & Smart911 9 Active Shooter 10 MetroSafe 11 Communication Technology Services 12-13 Emergency Medical Services 14 CPR Center 15 MetroCall 311 A Note from Our Director Dear Colleagues, Partners and Community Members, This Year End Report contains the highlights from another successful year for Emergency Services. Our services continue to be in high demand – we took over 1.4 million calls in MetroSafe, responded to over 125,000 Emergency Medical Services calls for service and handled nearly 200,000 citizen concerns in MetroCall 311 . While maintaining high functioning, day-to-day operations, we also implemented new initiatives and technologies that will help us provide better service to our citizens. One thing I would like to highlight is the expansion of LENSAlert (Louisville Emergency Notification System) to now include Smart911. Through one seamless sign up process, residents are able to elect to receive emergency notifications on their cell phones and provide information to 911 operators and first responders by completing a safety profile. These core features of our LENSAlert system will help enhance the personal safety of everyone who signs up. Signing up (goo.gl/ZYG3LL) only takes a few minutes, and it could save your life! I am proud of the continued planning and preparation our agency, as well as many other agencies at the local, state and federal levels, completed in 2017. -
Annual Report | 2018
MOVING EMS FORWARD ANNUAL REPORT | 2018 KY BOA UC R T n D mu ity N m & O E o c t F K e y c k h c n E u i S M t c a n E E e l C R k I G c o V E l em R N le st E C ge sy S Y L MEDICA kyems.com | #kyemsforward IN THIS REPORT 1 WELCOME 2 OUR MISSION 3 EMS FAST FACTS 4 MEET OUR TEAM 21-38 A CLOSER LOOK AT THE DATA 5-6 MEET OUR BOARD 22 KENTUCKY AGENCIES 7 BOARD ACCOMPLISHMENTS 23 TRAINING & EDUCATIONAL 8-12 MEET OUR COMMITTEES INSTITUTIONS 13-16 OUR ACCOMPLISHMENTS 24 KENTUCKY EDUCATORS 17 MISSION: LIFELINE 25 KENTUCKY PROVIDERS 18 AMBULANCE BLOCK GRANT 26-30 KENTUCKY INCIDENTS 19 NIOSH PILOT STUDY 31 INCIDENT DESTINATIONS 20 EMS VEHICLES 32 GROUND VS AIR MED TRANSPORTS 33 NALOXONE ADMINISTRATIONS 34 HIGHWAY SAFETY INCIDENTS 35 CARDIAC ARREST INCIDENTS 36 COMMUNITY PARAMEDICINE 37 STATEWIDE EMPLOYEE ATTRITION 38 PATIENT COMPLAINTS 39 CURRENT BOARD PROJECTS Connect with KBEMS: kyems.com KyBoardEMS KBEMS 118 James Court | Suite 50 | Lexington, KY 40505 | 859.256.3565 W E L C O M E Twenty-four hours a day, seven days a week, Emergency Medical Service Responders in our Commonwealth are delivering exceptional pre-hospital emergency medical care. What we do in Emergency Medical Services is important. EMS is a necessary service that is vital for our community and the nation. EMTs and paramedics are the healthcare safety net for all of us. -

Acls Policy for Residents
2021-2022 RESIDENT POLICIES AND PROCEDURES UNIVERSITY OF LOUISVILLE OFFICE OF GRADUATE MEDICAL EDUCATION Contents Page I ACLS Policy 3 II Accommodations for Residents with Disability Policy 4 III Campus Health Services Office a. Services Provided 5 b. Immunization Requirements and Policy 6 c. Exposure to Bloodborne Pathogens 7 d. Mental Health Services 8 IV Change of Service Dates 9 V Compliance with Teaching Physician Regulations Policy 10 VI Delinquent Medical Records 11 VII Disaster Policy 12-13 VIII Drug Free School Notice 14 IX Due Process a. Academic Probation 15 b. Grievance Procedure 16 X Resident Work Hours Policy and Procedures 17-21 XI Evaluation, Probation, and Termination Policy 22 XII Email Accounts 23 XIII Fringe Benefits 24-26 XIV HIPPA 27-28 XV House Staff Council 29 XVI Impaired Residents/Substance Abuse Policy 30 XVII International Residents 31 XVIII Leave Time a. Leave of Absence Policy 32-34 b. Leave Request Form 35 c. Vacation Leave 36-37 XIX Malpractice Coverage 38 1 XX Medical Licensure Policy 39-40 XXI Moonlighting Policy 41-42 XXII MedHub 43 XXIII Away Rotations 44-46 XXIV Pay Schedule and Paychecks 47 XXV Program Closure Policy and Procedure 48-49 XXVI Restrictive Covenants Policy 50 XXVII Sexual Harassment Policy 51 XXVIII Student Mistreatment Policy 52-53 XXIX Student Pregnancy Accommodation Policy 54-57 XXX Supervision Policy 58-59 XXXI Training Sites 60-63 XXXII Transition of Care and Handoff Policy 64-66 XXXIII Vendor Policy 67-69 XXXIV Weather Policy 70 XXXV Worker’s Compensation 71-72 Published by: Office of Graduate Medical Education University of Louisville School of Medicine 323 E. -

Fleet Repair Charges February 2010 Fleet Repair Charges Table of Contents
Emergency Medical Services Fleet Repair Charges February 2010 Fleet Repair Charges Table of Contents Transmittal Letter ............................................................................................................ 2 Introduction ..................................................................................................................... 2 Scope ............................................................................................................................... 3 Opinion ........................................................................................................................... 3 Corrective Action Plan .................................................................................................... 4 Internal Control Rating ................................................................................................... 5 Background ..................................................................................................................... 6 Summary of Audit Results .............................................................................................. 6 Observations and Recommendations .............................................................................. 8 #1 – General Administration ........................................................................................... 9 Emergency Medical Services Corrective Action Plan ........................................................................ 10 Fire Department Corrective Action Plan ............................................................................................