Immunochip SNP Array Identifies Novel Genetic Variants
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Wiskott-Aldrich Syndrome: the Actin Cytoskeleton and Immune Cell Function
Disease Markers 29 (2010) 157–175 157 DOI 10.3233/DMA-2010-0735 IOS Press The Wiskott-Aldrich syndrome: The actin cytoskeleton and immune cell function Michael P. Blundella, Austen Wortha,b, Gerben Boumaa and Adrian J. Thrashera,b,∗ aMolecular Immunology Unit, UCL Institute of Child Health, London, UK bDepartment of Immunology, Great Ormond Street Hospital NHS Trust, Great Ormond Street, London, UK Abstract. Wiskott-Aldrich syndrome (WAS) is a rare X-linked recessive primary immunodeficiency characterised by immune dysregulation, microthrombocytopaenia, eczema and lymphoid malignancies. Mutations in the WAS gene can lead to distinct syndrome variations which largely, although not exclusively, depend upon the mutation. Premature termination and deletions abrogate Wiskott-Aldrich syndrome protein (WASp) expression and lead to severe disease (WAS). Missense mutations usually result in reduced protein expression and the phenotypically milder X-linked thrombocytopenia (XLT) or attenuated WAS [1–3]. More recently however novel activating mutations have been described that give rise to X-linked neutropenia (XLN), a third syndrome defined by neutropenia with variable myelodysplasia [4–6]. WASP is key in transducing signals from the cell surface to the actin cytoskeleton, and a lack of WASp results in cytoskeletal defects that compromise multiple aspects of normal cellular activity including proliferation, phagocytosis, immune synapse formation, adhesion and directed migration. Keywords: Wiskott-Aldrich syndrome, actin polymerization, lymphocytes, -

Fungal Infections from Human and Animal Contact
Journal of Patient-Centered Research and Reviews Volume 4 Issue 2 Article 4 4-25-2017 Fungal Infections From Human and Animal Contact Dennis J. Baumgardner Follow this and additional works at: https://aurora.org/jpcrr Part of the Bacterial Infections and Mycoses Commons, Infectious Disease Commons, and the Skin and Connective Tissue Diseases Commons Recommended Citation Baumgardner DJ. Fungal infections from human and animal contact. J Patient Cent Res Rev. 2017;4:78-89. doi: 10.17294/2330-0698.1418 Published quarterly by Midwest-based health system Advocate Aurora Health and indexed in PubMed Central, the Journal of Patient-Centered Research and Reviews (JPCRR) is an open access, peer-reviewed medical journal focused on disseminating scholarly works devoted to improving patient-centered care practices, health outcomes, and the patient experience. REVIEW Fungal Infections From Human and Animal Contact Dennis J. Baumgardner, MD Aurora University of Wisconsin Medical Group, Aurora Health Care, Milwaukee, WI; Department of Family Medicine and Community Health, University of Wisconsin School of Medicine and Public Health, Madison, WI; Center for Urban Population Health, Milwaukee, WI Abstract Fungal infections in humans resulting from human or animal contact are relatively uncommon, but they include a significant proportion of dermatophyte infections. Some of the most commonly encountered diseases of the integument are dermatomycoses. Human or animal contact may be the source of all types of tinea infections, occasional candidal infections, and some other types of superficial or deep fungal infections. This narrative review focuses on the epidemiology, clinical features, diagnosis and treatment of anthropophilic dermatophyte infections primarily found in North America. -

HCST (NM 001007469) Human Recombinant Protein Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for TP319253 HCST (NM_001007469) Human Recombinant Protein Product data: Product Type: Recombinant Proteins Description: Recombinant protein of human hematopoietic cell signal transducer (HCST), transcript variant 2 Species: Human Expression Host: HEK293T Tag: C-Myc/DDK Predicted MW: 7.3 kDa Concentration: >50 ug/mL as determined by microplate BCA method Purity: > 80% as determined by SDS-PAGE and Coomassie blue staining Buffer: 25 mM Tris.HCl, pH 7.3, 100 mM glycine, 10% glycerol Preparation: Recombinant protein was captured through anti-DDK affinity column followed by conventional chromatography steps. Storage: Store at -80°C. Stability: Stable for 12 months from the date of receipt of the product under proper storage and handling conditions. Avoid repeated freeze-thaw cycles. RefSeq: NP_001007470 Locus ID: 10870 UniProt ID: Q9UBK5 RefSeq Size: 521 Cytogenetics: 19q13.12 RefSeq ORF: 279 Synonyms: DAP10; KAP10; PIK3AP This product is to be used for laboratory only. Not for diagnostic or therapeutic use. View online » ©2021 OriGene Technologies, Inc., 9620 Medical Center Drive, Ste 200, Rockville, MD 20850, US 1 / 2 HCST (NM_001007469) Human Recombinant Protein – TP319253 Summary: This gene encodes a transmembrane signaling adaptor that contains a YxxM motif in its cytoplasmic domain. The encoded protein may form part of the immune recognition receptor complex with the C-type lectin-like receptor NKG2D. As part of this receptor complex, this protein may activate phosphatidylinositol 3-kinase dependent signaling pathways through its intracytoplasmic YxxM motif. -

Candida Auris
microorganisms Review Candida auris: Epidemiology, Diagnosis, Pathogenesis, Antifungal Susceptibility, and Infection Control Measures to Combat the Spread of Infections in Healthcare Facilities Suhail Ahmad * and Wadha Alfouzan Department of Microbiology, Faculty of Medicine, Kuwait University, P.O. Box 24923, Safat 13110, Kuwait; [email protected] * Correspondence: [email protected]; Tel.: +965-2463-6503 Abstract: Candida auris, a recently recognized, often multidrug-resistant yeast, has become a sig- nificant fungal pathogen due to its ability to cause invasive infections and outbreaks in healthcare facilities which have been difficult to control and treat. The extraordinary abilities of C. auris to easily contaminate the environment around colonized patients and persist for long periods have recently re- sulted in major outbreaks in many countries. C. auris resists elimination by robust cleaning and other decontamination procedures, likely due to the formation of ‘dry’ biofilms. Susceptible hospitalized patients, particularly those with multiple comorbidities in intensive care settings, acquire C. auris rather easily from close contact with C. auris-infected patients, their environment, or the equipment used on colonized patients, often with fatal consequences. This review highlights the lessons learned from recent studies on the epidemiology, diagnosis, pathogenesis, susceptibility, and molecular basis of resistance to antifungal drugs and infection control measures to combat the spread of C. auris Citation: Ahmad, S.; Alfouzan, W. Candida auris: Epidemiology, infections in healthcare facilities. Particular emphasis is given to interventions aiming to prevent new Diagnosis, Pathogenesis, Antifungal infections in healthcare facilities, including the screening of susceptible patients for colonization; the Susceptibility, and Infection Control cleaning and decontamination of the environment, equipment, and colonized patients; and successful Measures to Combat the Spread of approaches to identify and treat infected patients, particularly during outbreaks. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Transcriptional Control of Tissue-Resident Memory T Cell Generation
Transcriptional control of tissue-resident memory T cell generation Filip Cvetkovski Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Graduate School of Arts and Sciences COLUMBIA UNIVERSITY 2019 © 2019 Filip Cvetkovski All rights reserved ABSTRACT Transcriptional control of tissue-resident memory T cell generation Filip Cvetkovski Tissue-resident memory T cells (TRM) are a non-circulating subset of memory that are maintained at sites of pathogen entry and mediate optimal protection against reinfection. Lung TRM can be generated in response to respiratory infection or vaccination, however, the molecular pathways involved in CD4+TRM establishment have not been defined. Here, we performed transcriptional profiling of influenza-specific lung CD4+TRM following influenza infection to identify pathways implicated in CD4+TRM generation and homeostasis. Lung CD4+TRM displayed a unique transcriptional profile distinct from spleen memory, including up-regulation of a gene network induced by the transcription factor IRF4, a known regulator of effector T cell differentiation. In addition, the gene expression profile of lung CD4+TRM was enriched in gene sets previously described in tissue-resident regulatory T cells. Up-regulation of immunomodulatory molecules such as CTLA-4, PD-1, and ICOS, suggested a potential regulatory role for CD4+TRM in tissues. Using loss-of-function genetic experiments in mice, we demonstrate that IRF4 is required for the generation of lung-localized pathogen-specific effector CD4+T cells during acute influenza infection. Influenza-specific IRF4−/− T cells failed to fully express CD44, and maintained high levels of CD62L compared to wild type, suggesting a defect in complete differentiation into lung-tropic effector T cells. -

Redefining the Specificity of Phosphoinositide-Binding by Human
bioRxiv preprint doi: https://doi.org/10.1101/2020.06.20.163253; this version posted June 21, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. Redefining the specificity of phosphoinositide-binding by human PH domain-containing proteins Nilmani Singh1†, Adriana Reyes-Ordoñez1†, Michael A. Compagnone1, Jesus F. Moreno Castillo1, Benjamin J. Leslie2, Taekjip Ha2,3,4,5, Jie Chen1* 1Department of Cell & Developmental Biology, University of Illinois at Urbana-Champaign, Urbana, IL 61801; 2Department of Biophysics and Biophysical Chemistry, Johns Hopkins University School of Medicine, Baltimore, MD 21205; 3Department of Biophysics, Johns Hopkins University, Baltimore, MD 21218; 4Department of Biomedical Engineering, Johns Hopkins University, Baltimore, MD 21205; 5Howard Hughes Medical Institute, Baltimore, MD 21205, USA †These authors contributed equally to this work. *Correspondence: [email protected]. bioRxiv preprint doi: https://doi.org/10.1101/2020.06.20.163253; this version posted June 21, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. ABSTRACT Pleckstrin homology (PH) domains are presumed to bind phosphoinositides (PIPs), but specific interaction with and regulation by PIPs for most PH domain-containing proteins are unclear. Here we employed a single-molecule pulldown assay to study interactions of lipid vesicles with full-length proteins in mammalian whole cell lysates. -

CD29 Identifies IFN-Γ–Producing Human CD8+ T Cells With
+ CD29 identifies IFN-γ–producing human CD8 T cells with an increased cytotoxic potential Benoît P. Nicoleta,b, Aurélie Guislaina,b, Floris P. J. van Alphenc, Raquel Gomez-Eerlandd, Ton N. M. Schumacherd, Maartje van den Biggelaarc,e, and Monika C. Wolkersa,b,1 aDepartment of Hematopoiesis, Sanquin Research, 1066 CX Amsterdam, The Netherlands; bLandsteiner Laboratory, Oncode Institute, Amsterdam University Medical Center, University of Amsterdam, 1105 AZ Amsterdam, The Netherlands; cDepartment of Research Facilities, Sanquin Research, 1066 CX Amsterdam, The Netherlands; dDivision of Molecular Oncology and Immunology, Oncode Institute, The Netherlands Cancer Institute, 1066 CX Amsterdam, The Netherlands; and eDepartment of Molecular and Cellular Haemostasis, Sanquin Research, 1066 CX Amsterdam, The Netherlands Edited by Anjana Rao, La Jolla Institute for Allergy and Immunology, La Jolla, CA, and approved February 12, 2020 (received for review August 12, 2019) Cytotoxic CD8+ T cells can effectively kill target cells by producing therefore developed a protocol that allowed for efficient iso- cytokines, chemokines, and granzymes. Expression of these effector lation of RNA and protein from fluorescence-activated cell molecules is however highly divergent, and tools that identify and sorting (FACS)-sorted fixed T cells after intracellular cytokine + preselect CD8 T cells with a cytotoxic expression profile are lacking. staining. With this top-down approach, we performed an un- + Human CD8 T cells can be divided into IFN-γ– and IL-2–producing biased RNA-sequencing (RNA-seq) and mass spectrometry cells. Unbiased transcriptomics and proteomics analysis on cytokine- γ– – + + (MS) analyses on IFN- and IL-2 producing primary human producing fixed CD8 T cells revealed that IL-2 cells produce helper + + + CD8 Tcells. -
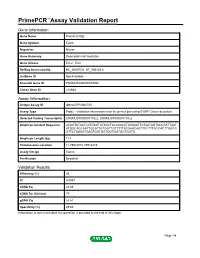
Primepcr™Assay Validation Report
PrimePCR™Assay Validation Report Gene Information Gene Name Protein EVI2B Gene Symbol Evi2b Organism Mouse Gene Summary Description Not Available Gene Aliases Evi-2, Evi2 RefSeq Accession No. NC_000077.6, NT_096135.6 UniGene ID Not Available Ensembl Gene ID ENSMUSG00000093938 Entrez Gene ID 216984 Assay Information Unique Assay ID qMmuCEP0062720 Assay Type Probe - Validation information is for the primer pair using SYBR® Green detection Detected Coding Transcript(s) ENSMUST00000179322, ENSMUST00000170422 Amplicon Context Sequence ACAGTATAATCATGAGTATAGCTACCAACATAGAAATTATAATAGTACCGATTAAT ATGGCAGCAATTGCATTGTGGTTGTTTTTATGAGCAGTTCCTTTGCCACTTGGTG GTTCTGAAGTGAGTGGTGGTGGTGGTGGTGGTG Amplicon Length (bp) 114 Chromosome Location 11:79516072-79516215 Assay Design Exonic Purification Desalted Validation Results Efficiency (%) 95 R2 0.9997 cDNA Cq 22.69 cDNA Tm (Celsius) 79 gDNA Cq 24.61 Specificity (%) 49.93 Information to assist with data interpretation is provided at the end of this report. Page 1/4 PrimePCR™Assay Validation Report Evi2b, Mouse Amplification Plot Amplification of cDNA generated from 25 ng of universal reference RNA Melt Peak Melt curve analysis of above amplification Standard Curve Standard curve generated using 20 million copies of template diluted 10-fold to 20 copies Page 2/4 PrimePCR™Assay Validation Report Products used to generate validation data Real-Time PCR Instrument CFX384 Real-Time PCR Detection System Reverse Transcription Reagent iScript™ Advanced cDNA Synthesis Kit for RT-qPCR Real-Time PCR Supermix SsoAdvanced™ SYBR® Green Supermix Experimental Sample qPCR Mouse Reference Total RNA Data Interpretation Unique Assay ID This is a unique identifier that can be used to identify the assay in the literature and online. Detected Coding Transcript(s) This is a list of the Ensembl transcript ID(s) that this assay will detect. -

Genetic Correlations Reveal the Shared Genetic Architecture of Transcription in Human Peripheral Blood
Hemani, G. (2017). Genetic correlations reveal the shared genetic architecture of transcription in human peripheral blood. Nature Communications, 8, [483]. https://doi.org/10.1038/s41467-017-00473- z Publisher's PDF, also known as Version of record License (if available): CC BY Link to published version (if available): 10.1038/s41467-017-00473-z Link to publication record in Explore Bristol Research PDF-document This is the final published version of the article (version of record). It first appeared online via Nature Publishing Group at https://www.nature.com/articles/s41467-017-00473-z . Please refer to any applicable terms of use of the publisher. University of Bristol - Explore Bristol Research General rights This document is made available in accordance with publisher policies. Please cite only the published version using the reference above. Full terms of use are available: http://www.bristol.ac.uk/red/research-policy/pure/user-guides/ebr-terms/ ARTICLE DOI: 10.1038/s41467-017-00473-z OPEN Genetic correlations reveal the shared genetic architecture of transcription in human peripheral blood Samuel W. Lukowski 1, Luke R. Lloyd-Jones1,2, Alexander Holloway2, Holger Kirsten3,4, Gibran Hemani 5,6, Jian Yang 1,2, Kerrin Small 7, Jing Zhao8, Andres Metspalu9, Emmanouil T. Dermitzakis10, Greg Gibson 8, Timothy D. Spector7, Joachim Thiery4,11, Markus Scholz 3,4, Grant W. Montgomery1,12, Tonu Esko 9, Peter M. Visscher 1,2 & Joseph E. Powell1,2 Transcript co-expression is regulated by a combination of shared genetic and environmental factors. Here, we estimate the proportion of co-expression that is due to shared genetic variance. -

1A Multiple Sclerosis Treatment
The Pharmacogenomics Journal (2012) 12, 134–146 & 2012 Macmillan Publishers Limited. All rights reserved 1470-269X/12 www.nature.com/tpj ORIGINAL ARTICLE Network analysis of transcriptional regulation in response to intramuscular interferon-b-1a multiple sclerosis treatment M Hecker1,2, RH Goertsches2,3, Interferon-b (IFN-b) is one of the major drugs for multiple sclerosis (MS) 3 2 treatment. The purpose of this study was to characterize the transcriptional C Fatum , D Koczan , effects induced by intramuscular IFN-b-1a therapy in patients with relapsing– 2 1 H-J Thiesen , R Guthke remitting form of MS. By using Affymetrix DNA microarrays, we obtained and UK Zettl3 genome-wide expression profiles of peripheral blood mononuclear cells of 24 MS patients within the first 4 weeks of IFN-b administration. We identified 1Leibniz Institute for Natural Product Research 121 genes that were significantly up- or downregulated compared with and Infection Biology—Hans-Knoell-Institute, baseline, with stronger changed expression at 1 week after start of therapy. Jena, Germany; 2University of Rostock, Institute of Immunology, Rostock, Germany and Eleven transcription factor-binding sites (TFBS) are overrepresented in the 3University of Rostock, Department of Neurology, regulatory regions of these genes, including those of IFN regulatory factors Rostock, Germany and NF-kB. We then applied TFBS-integrating least angle regression, a novel integrative algorithm for deriving gene regulatory networks from gene Correspondence: M Hecker, Leibniz Institute for Natural Product expression data and TFBS information, to reconstruct the underlying network Research and Infection Biology—Hans-Knoell- of molecular interactions. An NF-kB-centered sub-network of genes was Institute, Beutenbergstr. -

CALIFORNIA STATE UNIVERSITY, NORTHRIDGE Bioinformatic
CALIFORNIA STATE UNIVERSITY, NORTHRIDGE Bioinformatic Comparison of the EVI2A Promoter and Coding Regions A thesis submitted in partial fulfillment of the requirements for the degree of Master of Science in Biology By Max Weinstein May 2020 The thesis of Max Weinstein is approved: Professor Rheem D. Medh Date Professor Virginia Oberholzer Vandergon Date Professor Cindy Malone, Chair Date California State University Northridge ii Table of Contents Signature Page ii List of Figures v Abstract vi Introduction 1 Ecotropic Viral Integration Site 2A, a Gene within a Gene 7 Materials and Methods 11 PCR and Cloning of Recombinant Plasmid 11 Transformation and Cell Culture 13 Generation of Deletion Constructs 15 Transfection and Luciferase Assay 16 Identification of Transcription Factor Binding Sites 17 Determination of Region for Analysis 17 Multiple Sequence Alignment (MSA) 17 Model Testing 18 Tree Construction 18 Promoter and CDS Conserved Motif Search 19 Results and Discussion 20 Choice of Species for Analysis 20 Mapping of Potential Transcription Factor Binding Sites 20 Confirmation of Plasmid Generation through Gel Electrophoresis 21 Analysis of Deletion Constructs by Transient Transfection 22 EVI2A Coding DNA Sequence Phylogenetics 23 EVI2A Promoter Phylogenetics 23 EVI2A Conserved Leucine Zipper 25 iii EVI2A Conserved Casein kinase II phosphorylation site 26 EVI2A Conserved Sox-5 Binding Site 26 EVI2A Conserved HLF Binding Site 27 EVI2A Conserved cREL Binding Site 28 EVI2A Conserved CREB Binding Site 28 Summary 29 Appendix: Figures 30 Literature Cited 44 iv List of Figures Figure 1. EVI2A is nested within the gene NF1 30 Figure 2 Putative Transcriptions Start Site 31 Figure 3. Gel Electrophoresis of pGC Blue cloned, Restriction Digested Plasmid 32 Figure 4.