MRI Patterns of Shoulder Denervation: a Way to Make It Easy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Extended Insertion of Teres Minor Muscle: a Rare Case Report
Eur J Anat, 16 (3): 224-225 (2012) CASE REPORT Extended insertion of teres minor muscle: a rare case report Monica Jain, Lovesh Shukla, Dalbir Kaur Maharaja Agrasen Medical College, Agroha-125047, Hisar, Haryana, India SUMMARY upwards and laterally, and gets inserted on the lowest of the three impressions on the greater Teres minor is one of the muscles of the shoul- tubercle of the humerus and fuses with the der joint along with subscapularis, supraspina- capsule of the shoulder joint along with other tus and infraspinatus forming rotator cuff. muscles forming the rotator cuff. It is inner- Variations of teres minor are relatively uncom- vated by the posterior branch of the axillary mon. A unique and extended insertion of this nerve. It stabilizes the humerus by holding muscle is being reported in the present case. the humeral head in the glenoid cavity of the Knowledge of the anatomy of this muscle is scapula, a and causes lateral rotation of the important to avoid injury to the axillary nerve arm (Johnson, 2008). Variations of teres and posterior circumflex humeral vessels while minor are relatively uncommon and have been surgically approaching the shoulder joint and occasionally reported by various authors inserting portals of the arthroscope in a poste- (Bergman et al., 2006). rior approach to the shoulder joint. Key words: Teres minor – Rotator cuff – CASE REPORT Shoulder joint – Capsule of shoulder joint – Humerus – Surgical neck of humerus During routine dissection of the shoulder region of upper limb of an approximately 50 year-old male cadaver for undergraduate teach- INTRODUCTION ing and training, a unique and extended inser- tion of the teres minor muscle was found on the Teres minor is a one of the short scapular right side. -

M1 – Muscled Arm
M1 – Muscled Arm See diagram on next page 1. tendinous junction 38. brachial artery 2. dorsal interosseous muscles of hand 39. humerus 3. radial nerve 40. lateral epicondyle of humerus 4. radial artery 41. tendon of flexor carpi radialis muscle 5. extensor retinaculum 42. median nerve 6. abductor pollicis brevis muscle 43. flexor retinaculum 7. extensor carpi radialis brevis muscle 44. tendon of palmaris longus muscle 8. extensor carpi radialis longus muscle 45. common palmar digital nerves of 9. brachioradialis muscle median nerve 10. brachialis muscle 46. flexor pollicis brevis muscle 11. deltoid muscle 47. adductor pollicis muscle 12. supraspinatus muscle 48. lumbrical muscles of hand 13. scapular spine 49. tendon of flexor digitorium 14. trapezius muscle superficialis muscle 15. infraspinatus muscle 50. superficial transverse metacarpal 16. latissimus dorsi muscle ligament 17. teres major muscle 51. common palmar digital arteries 18. teres minor muscle 52. digital synovial sheath 19. triangular space 53. tendon of flexor digitorum profundus 20. long head of triceps brachii muscle muscle 21. lateral head of triceps brachii muscle 54. annular part of fibrous tendon 22. tendon of triceps brachii muscle sheaths 23. ulnar nerve 55. proper palmar digital nerves of ulnar 24. anconeus muscle nerve 25. medial epicondyle of humerus 56. cruciform part of fibrous tendon 26. olecranon process of ulna sheaths 27. flexor carpi ulnaris muscle 57. superficial palmar arch 28. extensor digitorum muscle of hand 58. abductor digiti minimi muscle of hand 29. extensor carpi ulnaris muscle 59. opponens digiti minimi muscle of 30. tendon of extensor digitorium muscle hand of hand 60. superficial branch of ulnar nerve 31. -
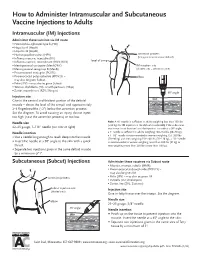
How to Administer Intramuscular and Subcutaneous Vaccines to Adults
How to Administer Intramuscular and Subcutaneous Vaccine Injections to Adults Intramuscular (IM) Injections Administer these vaccines via IM route • Haemophilus influenzae type b (Hib) • Hepatitis A (HepA) • Hepatitis B (HepB) • Human papillomavirus (HPV) acromion process (bony prominence above deltoid) • Influenza vaccine, injectable (IIV) • level of armpit • Influenza vaccine, recombinant (RIV3; RIV4) • Meningococcal conjugate (MenACWY) IM injection site • Meningococcal serogroup B (MenB) (shaded area = deltoid muscle) • Pneumococcal conjugate (PCV13) • Pneumococcal polysaccharide (PPSV23) – elbow may also be given Subcut • Polio (IPV) – may also be given Subcut • Tetanus, diphtheria (Td), or with pertussis (Tdap) • Zoster, recombinant (RZV; Shingrix) 90° angle Injection site skin Give in the central and thickest portion of the deltoid muscle – above the level of the armpit and approximately subcutaneous tissue 2–3 fingerbreadths (~2") below the acromion process. See the diagram. To avoid causing an injury, do not inject muscle too high (near the acromion process) or too low. Needle size Note: A ⅝" needle is sufficient in adults weighing less than 130 lbs (<60 kg) for IM injection in the deltoid muscle only if the subcutane- 22–25 gauge, 1–1½" needle (see note at right) ous tissue is not bunched and the injection is made at a 90° angle; Needle insertion a 1" needle is sufficient in adults weighing 130–152 lbs (60–70 kg); a 1–1½" needle is recommended in women weighing 153–200 lbs • Use a needle long enough to reach deep into the muscle. (70–90 kg) and men weighing 153–260 lbs (70–118 kg); a 1½" needle • Insert the needle at a 90° angle to the skin with a quick is recommended in women weighing more than 200 lbs (91 kg) or thrust. -

Anatomy, Shoulder and Upper Limb, Shoulder Muscles
Eovaldi BJ, Varacallo M. Anatomy, Shoulder and Upper Limb, Shoulder Muscles. [Updated 2018 Dec 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534836/ Anatomy, Shoulder and Upper Limb, Shoulder Muscles Authors Benjamin J. Eovaldi1; Matthew Varacallo2. Affilations 1 University of Tennessee HSC 2 Department of Orthopaedic Surgery, University of Kentucky School of Medicine Last Update: December 3, 2018. Introduction The shoulder joint (glenohumeral joint) is a ball and socket joint with the most extensive range of motion in the human body. The muscles of the shoulder dynamically function in performing a wide range of motion, specifically the rotator cuff muscles which function to move the shoulder and arm as well as provide structural integrity to the shoulder joint. The different movements of the shoulder are: abduction, adduction, flexion, extension, internal rotation, and external rotation.[1] The central bony structure of the shoulder is the scapula. All the muscles of the shoulder joint interact with the scapula. At the lateral aspect of the scapula is the articular surface of the glenohumeral joint, the glenoid cavity. The glenoid cavity is peripherally surrounded and reinforced by the glenoid labrum, shoulder joint capsule, supporting ligaments, and the myotendinous attachments of the rotator cuff muscles. The muscles of the shoulder play a critical role in providing stability to the shoulder joint. The primary muscle group that supports the shoulder joint is the rotator cuff muscles. The four rotator cuff muscles include:[2] • Supraspinatus • Infraspinatus • Teres minor • Subscapularis. Structure and Function The upper extremity is attached to the appendicular skeleton by way of the sternoclavicular joint. -
What Causes Infraspinatus Pain and How Can I Treat It?
visited 9/9/2020 9/9/2020 Infraspinatus Pain Causes, Symptoms, and Treatments SUBSCRIBE What Causes Infraspinatus Pain and How Can I Treat It? Medically reviewed by Deborah Weatherspoon, Ph.D., R.N., CRNA — Written by Erica Hersh on January 15, 2020 Causes and symptoms Trigger points and referred pain Diagnosis Treatment Outlook Summary The infraspinatus is one of four muscles that make up the rotator cuff, which helps your arm and shoulder move and stay stable. Your infraspinatus is in the back of your shoulder. It attaches the top of your humerus (the top bone in your arm) to your shoulder, and it helps you rotate your arm to the side. Pain in the infraspinatus is most likely caused by repetitive motion involving the shoulder. Swimmers, tennis players, painters, and carpenters get it more frequently. It also becomes more likely as you get older. There are several potential causes of infraspinatus pain. Some are serious, but none are life threatening. ADVERTISEMENT ADVERTISEMENT Infraspinatus muscle pain causes https://www.healthline.com/health/infraspinatus-pain 1/15 visited 9/9/2020 9/9/2020 Infraspinatus Pain Causes, Symptoms, and Treatments Sometimes, infraspinatus pain is due to minor strains or wear and tear. In these cases, rest will likely relieve the pain. But your pain may also be caused by an injury or more serious conditions. Infraspinatus tear There are two types of infraspinatus tears: A partial tear will damage the tendon, but it doesn’t go all the way through. It’s usually caused by repetitive stress or normal aging. A complete, or full-thickness, tear severs the infraspinatus from the bone. -

Kinematics Based Physical Modelling and Experimental Analysis of The
INGENIERÍA E INVESTIGACIÓN VOL. 37 N.° 3, DECEMBER - 2017 (115-123) DOI: http://dx.doi.org/10.15446/ing.investig.v37n3.63144 Kinematics based physical modelling and experimental analysis of the shoulder joint complex Modelo físico basado en cinemática y análisis experimental del complejo articular del hombro Diego Almeida-Galárraga1, Antonio Ros-Felip2, Virginia Álvarez-Sánchez3, Fernando Marco-Martinez4, and Laura Serrano-Mateo5 ABSTRACT The purpose of this work is to develop an experimental physical model of the shoulder joint complex. The aim of this research is to validate the model built and identify the forces on specified positions of this joint. The shoulder musculoskeletal structures have been replicated to evaluate the forces to which muscle fibres are subjected in different equilibrium positions: 60º flexion, 60º abduction and 30º abduction and flexion. The physical model represents, quite accurately, the shoulder complex. It has 12 real degrees of freedom, which allows motions such as abduction, flexion, adduction and extension and to calculate the resultant forces of the represented muscles. The built physical model is versatile and easily manipulated and represents, above all, a model for teaching applications on anatomy and shoulder joint complex biomechanics. Moreover, it is a valid research tool on muscle actions related to abduction, adduction, flexion, extension, internal and external rotation motions or combination among them. Keywords: Physical model, shoulder joint, experimental technique, tensions analysis, biomechanics, kinetics, cinematic. RESUMEN Este trabajo consiste en desarrollar un modelo físico experimental del complejo articular del hombro. El objetivo en esta investigación es validar el modelo construido e identificar las fuerzas en posiciones específicas de esta articulación. -

Arterial Supply to the Rotator Cuff Muscles
Int. J. Morphol., 32(1):136-140, 2014. Arterial Supply to the Rotator Cuff Muscles Suministro Arterial de los Músculos del Manguito Rotador N. Naidoo*; L. Lazarus*; B. Z. De Gama*; N. O. Ajayi* & K. S. Satyapal* NAIDOO, N.; LAZARUS, L.; DE GAMA, B. Z.; AJAYI, N. O. & SATYAPAL, K. S. Arterial supply to the rotator cuff muscles.Int. J. Morphol., 32(1):136-140, 2014. SUMMARY: The arterial supply to the rotator cuff muscles is generally provided by the subscapular, circumflex scapular, posterior circumflex humeral and suprascapular arteries. This study involved the bilateral dissection of the scapulohumeral region of 31 adult and 19 fetal cadaveric specimens. The subscapularis muscle was supplied by the subscapular, suprascapular and circumflex scapular arteries. The supraspinatus and infraspinatus muscles were supplied by the suprascapular artery. The infraspinatus and teres minor muscles were found to be supplied by the circumflex scapular artery. In addition to the branches of these parent arteries, the rotator cuff muscles were found to be supplied by the dorsal scapular, lateral thoracic, thoracodorsal and posterior circumflex humeral arteries. The variations in the arterial supply to the rotator cuff muscles recorded in this study are unique and were not described in the literature reviewed. Due to the increased frequency of operative procedures in the scapulohumeral region, the knowledge of variations in the arterial supply to the rotator cuff muscles may be of practical importance to surgeons and radiologists. KEY WORDS: Arterial supply; Variations; Rotator cuff muscles; Parent arteries. INTRODUCTION (Abrassart et al.). In addition, the muscular parts of infraspinatus and teres minor muscles were supplied by the circumflex scapular artery while the tendinous parts of these The rotator cuff is a musculotendionous cuff formed muscles received branches from the posterior circumflex by the fusion of the tendons of four muscles – viz. -

Electrodiagnosis of Brachial Plexopathies and Proximal Upper Extremity Neuropathies
Electrodiagnosis of Brachial Plexopathies and Proximal Upper Extremity Neuropathies Zachary Simmons, MD* KEYWORDS Brachial plexus Brachial plexopathy Axillary nerve Musculocutaneous nerve Suprascapular nerve Nerve conduction studies Electromyography KEY POINTS The brachial plexus provides all motor and sensory innervation of the upper extremity. The plexus is usually derived from the C5 through T1 anterior primary rami, which divide in various ways to form the upper, middle, and lower trunks; the lateral, posterior, and medial cords; and multiple terminal branches. Traction is the most common cause of brachial plexopathy, although compression, lacer- ations, ischemia, neoplasms, radiation, thoracic outlet syndrome, and neuralgic amyotro- phy may all produce brachial plexus lesions. Upper extremity mononeuropathies affecting the musculocutaneous, axillary, and supra- scapular motor nerves and the medial and lateral antebrachial cutaneous sensory nerves often occur in the context of more widespread brachial plexus damage, often from trauma or neuralgic amyotrophy but may occur in isolation. Extensive electrodiagnostic testing often is needed to properly localize lesions of the brachial plexus, frequently requiring testing of sensory nerves, which are not commonly used in the assessment of other types of lesions. INTRODUCTION Few anatomic structures are as daunting to medical students, residents, and prac- ticing physicians as the brachial plexus. Yet, detailed understanding of brachial plexus anatomy is central to electrodiagnosis because of the plexus’ role in supplying all motor and sensory innervation of the upper extremity and shoulder girdle. There also are several proximal upper extremity nerves, derived from the brachial plexus, Conflicts of Interest: None. Neuromuscular Program and ALS Center, Penn State Hershey Medical Center, Penn State College of Medicine, PA, USA * Department of Neurology, Penn State Hershey Medical Center, EC 037 30 Hope Drive, PO Box 859, Hershey, PA 17033. -

Upper Extremities
Relationships The pectoralis minor muscle is positioned posterior (deep) to the pectoralis major muscle. The thoracoacromial artery passes medial to the pectoralis minor muscle. The lateral thoracic artery is positioned lateral to the pectoralis minor muscle. The axillary artery passes posterior (deep) to the pectoralis minor muscle. The anterior circumflex humeral artery passes directly anterior to the humerus (surgical neck). The posterior circumflex humeral artery passes directly medial and posterior to the humerus (surgical neck). The cords of the brachial plexus pass posterior (deep) to the pectoralis minor muscle. The cords of the brachial plexus are positioned lateral, posterior and medial to the axillary artery. The ulnar nerve passes posterior to the medial epicondyle of the humerus. The long thoracic nerve is positioned directly lateral to the serratus anterior muscle. The axillary nerve passes medial and posterior to the humerus (surgical neck). The subscapularis muscle (tendon) passes anterior to the head of the humerus (glenohumeral joint). The brachial artery is positioned medial to the humerus (shaft). The profunda brachii artery passes posterior to the shaft of the humerus. The superior ulnar collateral artery passes posterior to the medial epicondyle of the humerus. The axillary nerve passes lateral to the long head of the triceps muscle (traverses the quadrangular space). The axillary nerve passes directly posterior to the humerus (surgical neck). The posterior circumflex humeral artery passes directly medial and posterior to the humerus (surgical neck). The posterior circumflex humeral artery passes lateral to the long head of the triceps muscle (traverses the quadrangular space). The infraspinatus muscle (tendon) passes posterior to the head and surgical neck of the humerus (glenohumeral joint). -

Chapter 5 the Shoulder Joint
The Shoulder Joint • Shoulder joint is attached to axial skeleton via the clavicle at SC joint • Scapula movement usually occurs with movement of humerus Chapter 5 – Humeral flexion & abduction require scapula The Shoulder Joint elevation, rotation upward, & abduction – Humeral adduction & extension results in scapula depression, rotation downward, & adduction Manual of Structural Kinesiology – Scapula abduction occurs with humeral internal R.T. Floyd, EdD, ATC, CSCS rotation & horizontal adduction – Scapula adduction occurs with humeral external rotation & horizontal abduction © McGraw-Hill Higher Education. All rights reserved. 5-1 © McGraw-Hill Higher Education. All rights reserved. 5-2 The Shoulder Joint Bones • Wide range of motion of the shoulder joint in • Scapula, clavicle, & humerus serve as many different planes requires a significant attachments for shoulder joint muscles amount of laxity – Scapular landmarks • Common to have instability problems • supraspinatus fossa – Rotator cuff impingement • infraspinatus fossa – Subluxations & dislocations • subscapular fossa • spine of the scapula • The price of mobility is reduced stability • glenoid cavity • The more mobile a joint is, the less stable it • coracoid process is & the more stable it is, the less mobile • acromion process • inferior angle © McGraw-Hill Higher Education. All rights reserved. 5-3 © McGraw-Hill Higher Education. All rights reserved. From Seeley RR, Stephens TD, Tate P: Anatomy and physiology , ed 7, 5-4 New York, 2006, McGraw-Hill Bones Bones • Scapula, clavicle, & humerus serve as • Key bony landmarks attachments for shoulder joint muscles – Acromion process – Humeral landmarks – Glenoid fossa • Head – Lateral border • Greater tubercle – Inferior angle • Lesser tubercle – Medial border • Intertubercular groove • Deltoid tuberosity – Superior angle – Spine of the scapula © McGraw-Hill Higher Education. -
Isolated Loss of Active External Rotation: a Distinct Entity and Results of L'episcopo Tendon Transfer
J Shoulder Elbow Surg (2018) 27, 499–509 www.elsevier.com/locate/ymse Isolated loss of active external rotation: a distinct entity and results of L’Episcopo tendon transfer Pascal Boileau,MDa,*, Mohammed Baba,MDb, Walter B. McClelland Jr, MDc, Charles-Édouard Thélu,MDd, Christophe Trojani, MD, PhDa, Nicolas Bronsard, MD, PhDa aInstitut Universitaire Locomoteur et Sport (iULS), Hôpital Pasteur 2, University of Nice Sophia Antipolis (UNSA), Nice, France bSydney Adventist Hospital, Wahroonga, NSW, Australia cPeachtree Orthopaedic Clinic, Atlanta, GA, USA dHôpital Privé Métropole, Lille, France Background: The purpose of this study was to characterize a subgroup of cuff-deficient patients with iso- lated loss of active external rotation (ILER) but preserved active elevation and to evaluate the outcomes of the L’Episcopo procedure to restore horizontal muscle balance. Methods: During a 10-year period, 26 patients (14 men, 12 women) were identified with ILER in the setting of massive irreparable posterosuperior cuff tears. A modified L’Episcopo tendon transfer was per- formed to restore active external rotation and to improve shoulder function. The mean age at surgery was 64.5 years (29-83 years). Patients were evaluated with a mean follow-up of 52 months (range, 24-104 months). Results: Preoperatively, despite maintained active elevation (average of 161°), ILER patients com- plained about loss of spatial control of the arm and difficulties with activities of daily living. On computed tomography scan or magnetic resonance imaging, there was severe fatty infiltration of infraspinatus and absent or atrophic teres minor. After L’Episcopo transfer, 84% of patients were satisfied. The gain in active external rotation was +26° in arm at the side and +18.5° in 90° abduction. -

Changes in Infraspinatus Cross-Sectional Area and Echo Intensity in Relation to Scapular Dyskinesis and Overhead Training Volume in Collegiate Volleyball Players
CHANGES IN INFRASPINATUS CROSS-SECTIONAL AREA AND ECHO INTENSITY IN RELATION TO SCAPULAR DYSKINESIS AND OVERHEAD TRAINING VOLUME IN COLLEGIATE VOLLEYBALL PLAYERS Kimberly Chase A thesis submitted to the faculty at the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Masters of Arts in the Department of Exercise & Sport Science (Athletic Training) in the College of Arts & Sciences. Chapel Hill 2016 Approved by: D. Padua T. Blackburn L. Stanley i © 2016 Kimberly Chase ALL RIGHTS RESERVED ii ABSTRACT Kimberly Chase: Changes in Infraspinatus Cross-Sectional Area and Echo Intensity in Relation to Scapular Dyskinesis and Overhead Training Volume in Collegiate Volleyball Players (Under the Direction of Darin Padua) During the pre-season injury risk in volleyball is highest at 6.1 injuries/1000 exposures. Injury to the posterior shoulder, specifically the infraspinatus, has been attributed to repetitive eccentric loading. The high volume of overhead activity in the collegiate volleyball player has been identified is a risk factor for upper extremity injury. Cross sectional area and echo intensity of the infraspinatus muscle were assessed using diagnostic ultrasound to measure muscle damage. Visual observation of scapular dyskinesis was completed at baseline and 24 hours following the pre-season training period to assess changes due to pre-season training volume. Correlations between cross sectional area, echo intensity, scapular dyskinesis, and swing count were also examined to assess relationships between these variables. Acceptable reliability was established for all measurements. This study found no significant outcomes in cross sectional area or echo intensity, in the severity of scapular dyskinesis, or in relationships between the variables of interest.