Neurotization to Innervate the Deltoid and Biceps: 3 Cases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Monday: Back, Biceps, Forearms, Traps & Abs Wednesday
THE TOOLS YOU NEED TO BUILD THE BODY YOU WANT® Store Workouts Diet Plans Expert Guides Videos Tools BULLDOZER TRAINING 3 DAY WORKOUT SPLIT 3 day Bulldozer Training muscle building split. Combines rest-pause sets with progressive Main Goal: Build Muscle Time Per Workout: 30-45 Mins resistance. Workouts are shorter but more Training Level: Intermediate Equipment: Barbell, Bodyweight, intense. Program Duration: 8 Weeks Dumbbells, EZ Bar, Machines Link to Workout: https://www.muscleandstrength.com/ Days Per Week: 3 Days Author: Steve Shaw workouts/bulldozer-training-3-day-workout-split Monday: Back, Biceps, Forearms, Traps & Abs Exercise Mini Sets Rep Goal Rest Deadlift: Perform as many rest-paused singles as you (safely) can within 10 Mins. Use a weight you could easily perform a 10 rep set with. Rest as needed. When you can perform 15 reps, add weight the next time you deadlift. Barbell Row 5 25 30 / 30 / 45 / 45 Wide Grip Pull Up 5 35 30 / 30 / 30 / 30 Standing Dumbbell Curl 4 25 30 / 30 / 30 EZ Bar Preacher Curl 4 25 30 / 30 / 30 Seated Barbell Wrist Curl 4 35 30 / 30 / 30 Barbell Shrug 5 35 30 / 30 / 30 / 30 Preferred Abs Exercise(s): I recommend using at least one weighted exercise (e.g. Weighted Sit Ups or Cable Crunches). Rest Periods: 30 / 30 / 45 / 45 notates rest periods between each set. Take 30 Secs after the 1st set, 30 Secs after the 2nd set, 45 Secs after the 3rd set, etc. After the final set, rest, and move on to the next exercise. -

M1 – Muscled Arm
M1 – Muscled Arm See diagram on next page 1. tendinous junction 38. brachial artery 2. dorsal interosseous muscles of hand 39. humerus 3. radial nerve 40. lateral epicondyle of humerus 4. radial artery 41. tendon of flexor carpi radialis muscle 5. extensor retinaculum 42. median nerve 6. abductor pollicis brevis muscle 43. flexor retinaculum 7. extensor carpi radialis brevis muscle 44. tendon of palmaris longus muscle 8. extensor carpi radialis longus muscle 45. common palmar digital nerves of 9. brachioradialis muscle median nerve 10. brachialis muscle 46. flexor pollicis brevis muscle 11. deltoid muscle 47. adductor pollicis muscle 12. supraspinatus muscle 48. lumbrical muscles of hand 13. scapular spine 49. tendon of flexor digitorium 14. trapezius muscle superficialis muscle 15. infraspinatus muscle 50. superficial transverse metacarpal 16. latissimus dorsi muscle ligament 17. teres major muscle 51. common palmar digital arteries 18. teres minor muscle 52. digital synovial sheath 19. triangular space 53. tendon of flexor digitorum profundus 20. long head of triceps brachii muscle muscle 21. lateral head of triceps brachii muscle 54. annular part of fibrous tendon 22. tendon of triceps brachii muscle sheaths 23. ulnar nerve 55. proper palmar digital nerves of ulnar 24. anconeus muscle nerve 25. medial epicondyle of humerus 56. cruciform part of fibrous tendon 26. olecranon process of ulna sheaths 27. flexor carpi ulnaris muscle 57. superficial palmar arch 28. extensor digitorum muscle of hand 58. abductor digiti minimi muscle of hand 29. extensor carpi ulnaris muscle 59. opponens digiti minimi muscle of 30. tendon of extensor digitorium muscle hand of hand 60. superficial branch of ulnar nerve 31. -
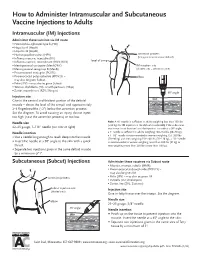
How to Administer Intramuscular and Subcutaneous Vaccines to Adults
How to Administer Intramuscular and Subcutaneous Vaccine Injections to Adults Intramuscular (IM) Injections Administer these vaccines via IM route • Haemophilus influenzae type b (Hib) • Hepatitis A (HepA) • Hepatitis B (HepB) • Human papillomavirus (HPV) acromion process (bony prominence above deltoid) • Influenza vaccine, injectable (IIV) • level of armpit • Influenza vaccine, recombinant (RIV3; RIV4) • Meningococcal conjugate (MenACWY) IM injection site • Meningococcal serogroup B (MenB) (shaded area = deltoid muscle) • Pneumococcal conjugate (PCV13) • Pneumococcal polysaccharide (PPSV23) – elbow may also be given Subcut • Polio (IPV) – may also be given Subcut • Tetanus, diphtheria (Td), or with pertussis (Tdap) • Zoster, recombinant (RZV; Shingrix) 90° angle Injection site skin Give in the central and thickest portion of the deltoid muscle – above the level of the armpit and approximately subcutaneous tissue 2–3 fingerbreadths (~2") below the acromion process. See the diagram. To avoid causing an injury, do not inject muscle too high (near the acromion process) or too low. Needle size Note: A ⅝" needle is sufficient in adults weighing less than 130 lbs (<60 kg) for IM injection in the deltoid muscle only if the subcutane- 22–25 gauge, 1–1½" needle (see note at right) ous tissue is not bunched and the injection is made at a 90° angle; Needle insertion a 1" needle is sufficient in adults weighing 130–152 lbs (60–70 kg); a 1–1½" needle is recommended in women weighing 153–200 lbs • Use a needle long enough to reach deep into the muscle. (70–90 kg) and men weighing 153–260 lbs (70–118 kg); a 1½" needle • Insert the needle at a 90° angle to the skin with a quick is recommended in women weighing more than 200 lbs (91 kg) or thrust. -

MRI Patterns of Shoulder Denervation: a Way to Make It Easy
MRI Patterns Of Shoulder Denervation: A Way To Make It Easy Poster No.: C-2059 Congress: ECR 2018 Type: Educational Exhibit Authors: E. Rossetto1, P. Schvartzman2, V. N. Alarcon2, M. E. Scherer2, D. M. Cecchi3, F. M. Olivera Plata4; 1Buenos Aires, Capital Federal/ AR, 2Buenos Aires/AR, 3Capital Federal, Buenos Aires/AR, 4Ciudad Autonoma de Buenos Aires/AR Keywords: Musculoskeletal joint, Musculoskeletal soft tissue, Neuroradiology peripheral nerve, MR, Education, eLearning, Edema, Inflammation, Education and training DOI: 10.1594/ecr2018/C-2059 Any information contained in this pdf file is automatically generated from digital material submitted to EPOS by third parties in the form of scientific presentations. References to any names, marks, products, or services of third parties or hypertext links to third- party sites or information are provided solely as a convenience to you and do not in any way constitute or imply ECR's endorsement, sponsorship or recommendation of the third party, information, product or service. ECR is not responsible for the content of these pages and does not make any representations regarding the content or accuracy of material in this file. As per copyright regulations, any unauthorised use of the material or parts thereof as well as commercial reproduction or multiple distribution by any traditional or electronically based reproduction/publication method ist strictly prohibited. You agree to defend, indemnify, and hold ECR harmless from and against any and all claims, damages, costs, and expenses, including attorneys' fees, arising from or related to your use of these pages. Please note: Links to movies, ppt slideshows and any other multimedia files are not available in the pdf version of presentations. -

Kinematics Based Physical Modelling and Experimental Analysis of The
INGENIERÍA E INVESTIGACIÓN VOL. 37 N.° 3, DECEMBER - 2017 (115-123) DOI: http://dx.doi.org/10.15446/ing.investig.v37n3.63144 Kinematics based physical modelling and experimental analysis of the shoulder joint complex Modelo físico basado en cinemática y análisis experimental del complejo articular del hombro Diego Almeida-Galárraga1, Antonio Ros-Felip2, Virginia Álvarez-Sánchez3, Fernando Marco-Martinez4, and Laura Serrano-Mateo5 ABSTRACT The purpose of this work is to develop an experimental physical model of the shoulder joint complex. The aim of this research is to validate the model built and identify the forces on specified positions of this joint. The shoulder musculoskeletal structures have been replicated to evaluate the forces to which muscle fibres are subjected in different equilibrium positions: 60º flexion, 60º abduction and 30º abduction and flexion. The physical model represents, quite accurately, the shoulder complex. It has 12 real degrees of freedom, which allows motions such as abduction, flexion, adduction and extension and to calculate the resultant forces of the represented muscles. The built physical model is versatile and easily manipulated and represents, above all, a model for teaching applications on anatomy and shoulder joint complex biomechanics. Moreover, it is a valid research tool on muscle actions related to abduction, adduction, flexion, extension, internal and external rotation motions or combination among them. Keywords: Physical model, shoulder joint, experimental technique, tensions analysis, biomechanics, kinetics, cinematic. RESUMEN Este trabajo consiste en desarrollar un modelo físico experimental del complejo articular del hombro. El objetivo en esta investigación es validar el modelo construido e identificar las fuerzas en posiciones específicas de esta articulación. -

Pronator Teres Tear at the Myotendinous Junction in the Recreational Golfer: a Case Report
International Journal of Orthopaedics Online Submissions: http: //www.ghrnet.org/index.php/ijo Int. J. of Orth. 2021 April 28; 8(2): 1457-1462 doi: 10.17554/j.issn.2311-5106.2021.08.405 ISSN 2311-5106 (Print), ISSN 2313-1462 (Online) CASE REPORT Pronator Teres Tear at the Myotendinous Junction in the Recreational Golfer: A Case Report Alvarho J. Guzman1, BA; Stewart A. Bryant1, MD; Shane M. Rayos Del Sol1, BS, MS; Brandon Gardner1, MD, PhD; Moyukh O. Chakrabarti1, MBBS; Patrick J. McGahan1, MD; James L. Chen1, MD 1 Department of Orthopedic Surgery, Advanced Orthopedics & was expected to make a complete return to pre-injury level athletic Sports Medicine, San Francisco, CA, the United States. activity with conservative management. With this article, we consider biceps rupture on the differential diagnoses associated with pronator Conflict-of-interest statement: The author(s) declare(s) that there teres musculotendinous injuries, emphasize the significance of club is no conflict of interest regarding the publication of this paper. type in relation to golfing injuries, and propose a potential pronator teres rupture non-operative rehabilitation protocol. Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external Key words: Pronator teres; Golf; Biceps; Ecchymosis; Rehabilitation reviewers. It is distributed in accordance with the Creative Com- protocol mons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non- © 2021 The Author(s). Published by ACT Publishing Group Ltd. All commercially, and license their derivative works on different terms, rights reserved. -

Workout Plan Pdf
WORKOUT PLAN PDF 17 INCHES – ARMS TRAINING PROGRAM 17 INCHES is a 10 weeks Arm training program to build size of Biceps & Triceps. This will help to gain 1-2 inches arms size and 8-10 pounds of muscle mass in 10 weeks. Follow the exact workout & nutrition plan for the proper results. GURU MANN – Nutritionist & Advanced Fitness Professional United States Guru Mann Fitness Inc. WORKOUT SPLIT OPTION 1 OPTION 2 MONDAY STRENGTH – BICEPS/TRICEPS ------ TUESDAY ------ STRENGTH – BICEPS/TRICEPS WEDNESDAY ------ ------ THURSDAY ENDURANCE – BICEPS/TRICEPS ------ FRIDAY ------ ENDURANCE – BICEPS/TRICEPS SATURDAY ------ ------ SUNDAY REST REST Combine it with other workout plan STRENGTH EXERCISES SETS REPS ALTERNATE EXERCISES 0 WARM UP DB CURL OR EMPLY BARBELL 2-3 15-20 --------- TRICEPS PUSHDOWN 1 SUPER SET 1A. EZ BARBELL CURL 3 8-7-6 STRAIGHT BAR CURL 1B. HAMMER CURL 2 SUPER SET 2A. BARBELL PREACHER CURL 3 8-7-6 DB PREACHER CURL 2B. DB CON. CURL 3 SUPER SET 3A. ROPE CURL 3 8-7-6 CLOSE GRIP BAR 3B. ROPE OVERHEAD EXT. CURL 4 SUPER SET 4A. SKULL CRUSHER 3 8-7-6 ---------- 4B. DB KICKBACK 5 SUPER SET 5A. DB OVERHEAD EXT. 3 8-7-6 5B. WEIGHTED CLOSE GRIP ---------- INCLINE PUSHUP 6 SUPER SET 6A. WRIST CURL (PALM UP) 3 8-7-6 WRIST CURL (PALM 6B. STANDING WRIST CURL FACING DOWN) REST IS 2-3 MIN IN BETWEEN THE SET. THERE IS NO REST IN-BETWEEN THE SUPER SET. ENDURANCE EXERCISES SETS REPS ALTERNATE EXERCISES 0 WARM UP DB CURL OR EMPLY BARBELL 3 15-20 --------- TRICEPS PUSHDOWN 1 SUPER SET 1A. -

Anatomy, Biomechanics, Physiology, Diagnosis and Treatment of Teres
ANATOMY, BIOMECHANICS, PHYSIOLOGY, DIAGNOSIS AND TREATMENT OF TERES MAJOR STRAINS IN THE CANINE Laurie Edge-Hughes, BScPT, CAFCI, CCRT Four Leg Rehabilitation Therapy & The Canine Fitness Centre Ltd, Calgary, AB, Canada The Canadian Horse and Animal Physical Rehabilitation Assn. The Animal Rehab Institute, Loxahatchee, Florida, USA BACKGROUND The canine shoulder apparatus is unique as compared to other canine joints and also when compared to the human shoulder. When compared to the hind limb it is interesting to note that the front limb has no boney attachment to the axial skeleton in that there is no clavicle in the canine. This factor alone means that muscular strength and co-ordination is of utmost importance to full functioning of the front limb. When compared to the human shoulder, one obvious difference is that the shoulder joint is a weight bearing joint. The orientation of the canine scapula and humerus is vertical and the weight distribution is 60 to 65 % on the front legs and 40 – 35% on the hind legs. Essentially dogs are like ‘front wheel drive vehicles’, designed to propel themselves forward by primarily ‘pulling’ from the front end. This is why identification and treatment of front limb muscle injuries is critically important for athletic or just high energy dogs who are most prone to injuring shoulder muscles. The teres major muscle is one that is commonly strained, often unidentified and hence not as effectively treated as it could be in the active canine patient. ANATOMY The teres major muscle originates from the caudal angle and caudal edge of the scapula and inserts into the eminence on the proximal 1/3 of the medial surface of the humerus. -

Anatomical Study of Pronator Teres Muscle Innervation and Clinical Significance in Nerve Transfer
Int. J. Morphol., 36(4):1500-1508, 2018. Anatomical Study of Pronator Teres Muscle Innervation and Clinical Significance in Nerve Transfer Estudio Anatómico de la Inervación del Músculo Pronador Redondo y Significado Clínico en la Transferencia Nerviosa Edie Benedito Caetano1; Luiz Angelo Vieira1; José João Sabongi Neto2; Maurício Benedito Ferreira Caetano2; Rodrigo Guerra Sabongi3; Luca Martinez4; Kelson Koiti Ogata4 & Eduardo Baldy de Sousa Boni4 CAETANO, E. B.; VIEIRA, L A.; SABONGI NETO, J. J. ; CAETANO, M. B. F.; SABONGI, R. G.; MARTINEZ, L.; OGATA, K. K. & BONI, E. B. S. Anatomical study of pronator teres muscle innervation and clinical significance in nerve transfer. Int. J. Morphol., 36(4):1500-1508, 2018. SUMMARY: The anatomical relationship of the median nerve and its innervation pattern are variable and may have direct implications in surgical procedures such as distal nerve transfers. The objective of this study was to evaluate the anatomical variations of pronator teres muscle (PTM) innervation and its clinical significance in nerve transfers. Data were collected regarding the number of median nerve branches, site of their origin, contribution with branches of other muscles and the possibility of transferring expendable branches of PTM to the anterior interosseous nerve (AIN) and radial nerve. The most common origin of the branches was proximal to the humeral intercondylar line. The presence of only one PTM branch was identified in 9 limbs, in which 6 was exclusive for this muscle. The majority of specimens presented more than one branch to the PTM, with two branches in 19, although only 6 of these did not share branches with other muscles. -

Bernard F. Hearon, M.D. Protocol E4 Physical Or Occupational Therapy
Bernard F. Hearon, M.D. 2778 N. Webb Road Shoulder, Elbow, Wrist, Hand Wichita, KS 67226 and Arthroscopic Surgery Phone: 316-631-1600 www.drhearon.com Fax: 316-631-1675 Protocol E4 Physical or Occupational Therapy Protocol for Distal Biceps Tendon Repair or Reattachment Phase I: Protection Phase (weeks 0-6) GOALS: • Protect the distal biceps repair and allow tendon-to-bone healing. • Prevent upper extremity joint stiffness. • Allow passive flexion and active extension of the elbow within hinged orthosis. ANCILLARY MEASURES: • Use pain medications as needed. • Elbow and wrist are immobilized in long-arm posterior splint first week postop. • Long-arm hinged orthosis is applied by therapist at one week postop visit. During weeks 2-6, progressive elbow extension is permitted by adjusting the orthosis biweekly. Elbow extension is first blocked at 90 degrees, then 60 degrees, then 30 degrees and then full elbow extension is permitted. EXERCISES: • Finger and Wrist ROM: Active flexion and extension of the wrist and fingers on the operated side is encouraged. Gripping exercises (rubber ball squeezes) are allowed. • Shoulder Range of Motion: Begin progressive active shoulder range of motion in all planes. Repeat 3 times per day, 10 repetitions. • Passive Elbow Flexion : With the unoperated hand, passively bend the operated elbow up in flexion. Complete 10 repetitions, 5-6 times per day. • Active Elbow Extension: After the elbow has been passively flexed, then actively extend the operated elbow as far as the hinged brace will allow. Complete 10 repetitions, 5-6 times per day. • Forearm Pronation and Supination: Begin to actively rotate the forearm at 3 weeks postop. -

Rotator Cuff Repair with Biceps Tenotomy/Tenodesis
Brian Bjerke, MD Rotator Cuff Repair with Biceps Tenotomy/Tenodesis Post-Operative Protocol Phase I – Maximum Protection (Weeks 0 to 6): • Goals: o Reduce inflammation o Decrease pain o Postural education o PROM as instructed • Restrictions/Exercise Progression: o Sling for 6 weeks per Dr. Bjerke’s instructions ▪ Patients will be placed into an UltraSling post-operative (sling with the pillow) o Ice and modalities to reduce pain and inflammation o Cervical ROM and basic deep neck flexor activation (chin tucks) o Instruction on proper head, neck and shoulder alignment o Active hand and wrist ROM o Passive biceps x6 weeks (AAROM; no tenotomy or tenodesis) o Active shoulder retraction o Shoulder PROM progression ▪ No motion x2 weeks ▪ Passive flexion 0°-90° from weeks 2-4, then full ▪ External rotation 0°-30° from weeks 2-4, then full ▪ Avoid internal rotation (thumb up back) until 8 weeks post-op o Encourage walks and low intensity cardiovascular exercises to promote healing • Manual Intervention: o Soft tissue massage- global shoulder and CT junction o Scar tissue mobilization when incisions are healed o Graded GH mobilizations o ST mobilizations Phase II – Progressive Stretching and Active ROM (Weeks 6 to 8): • Goals: 1 o Discontinue sling as instructed o Postural education o Focus on posterior chain strengthening o Begin AROM o PROM/AAROM: ▪ Flexion 150°+ ▪ 30°-50° ER @ 0 abduction ▪ 45°-70° ER at 70-90 abduction ▪ • Exercise Progression: o Progress to full range of motion flexion and external rotation as tolerated ▪ Use a combination of wand, pulleys, wall walks or table slides to ensure compliance. -

Biceps Tendon Tear at the Shoulder-Orthoinfo
Biceps Tendon Tear at the Shoulder Tendons attach muscles to bones. Your biceps tendons attach the biceps muscle to bones in the shoulder and in the elbow. If you tear the biceps tendon at the shoulder, you may lose some strength in your arm and have pain when you forcefully turn your arm from palm down to palm up. Many people can still function with a biceps tendon tear, and only need simple treatments to relieve symptoms. If symptoms cannot be relieved by nonsurgical treatments, or if a patient requires complete recovery of strength, surgery to repair the torn tendor may be required. Anatomy Your shoulder is a ball-and-socket joint made up of three bones: your upper arm bone (humerus), your shoulder blade (scapula), and your collarbone (clavicle). The head of your upper arm bone fits into a rounded socket in your shoulder blade. This socket is called the glenoid. A combination of muscles and tendons keeps your arm bone centered in your shoulder socket. These tissues are called the rotator cuff. They cover the head of your upper arm bone and attach it to your shoulder blade. The upper end of the biceps muscle has two tendons that attach it to bones in the shoulder. The long head attaches to the top of the shoulder socket (glenoid). The short head attaches to a bump on the shoulder blade called the coracoid process. There are two attachments of the biceps tendon at the shoulder joint. Description Biceps tendon tears can be either partial or complete. Partial tears. Many tears do not completely sever the tendon.