Responding to COVID-19: Health Sector Preparedness, Response and Lessons Learnt
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nepali Times Welcomes Feedback
#304 30 June - 6 July 2006 16 pages Rs 30 Explosive legacy There may be a ceasefire but not a week goes by without children and women dying from bombs scattered across Nepal. On 25 June, the anti-landmine group Geneva Call organised a seminar in Kathmandu that brought together Maoists and the victims of their bombs. On the podium was socket bomb victim 13-year-old Ashok Thapa Magar, sitting next to Maoist leaders Ailman and Ekraj Bhandari (pictured, right). After hearing Ashok’s mother relate how her son was wounded, the audience bombarded the Maoists with questions. Used to getting their way with the gun, the comrades have not yet learnt to engage in public debate. Their response was: war is not a picnic, people are killed and injured. After we attain victory, there will be no more violence, etc. But these answers didn't seem to satisfy Ashok’s mother about why her son had to suffer. Weekly Internet Poll # 304 Q... Do you think the seven party alliance has given in too much to Maoist demands? Total votes: 5,236 Weekly Internet Poll # 305. To vote go to: www.nepalitimes.com Q... Which among these is your favourite team in the 2006 Football World Cup? KIRAN PANDAY Parallel government Everywhere we look, we see double olitical transitions are a for bids resolution rejecting it. aparliamentary proclamations time of confusion. But the The government has a police This is a direct challenge to between 7-16 June to demote the P post-uprising interregnum force, the Maoists have their militia the Maoists and their strategy to king, delink him from the army is looking more and more bizarre. -

Reacting to Donald Trump's Challenge
centro studi per i popoli extra-europei “cesare bonacossa” - università di pavia The Journal of the Italian think tank on Asia founded by Giorgio Borsa in 1989 Vol. XXIX / 2018 Reacting to Donald Trump’s Challenge Edited by Michelguglielmo Torri Nicola Mocci viella centro studi per i popoli extra-europei “cesare bonacossa” - università di pavia ASIA MAIOR The Journal of the Italian think tank on Asia founded by Giorgio Borsa in 1989 Vol. XXIX / 2018 Reacting to Donald Trump’s Challenge Edited by Michelguglielmo Torri and Nicola Mocci viella Asia Maior. The Journal of the Italian Think Tank on Asia founded by Giorgio Borsa in 1989. Copyright © 2019 - Viella s.r.l. & Associazione Asia Maior ISBN 978-88-3313-241-9 (Paper) ISBN 978-88-3313-242-6 (Online) ISSN 2385-2526 (Paper) ISSN 2612-6680 (Online) Annual journal - Vol. XXIX, 2018 This journal is published jointly by the think tank Asia Maior (Associazione Asia Maior) & CSPE - Centro Studi per i Popoli extra-europei «Cesare Bonacossa», University of Pavia Asia Maior. The Journal of the Italian Think Tank on Asia founded by Giorgio Borsa in 1989 is an open-access journal, whose issues and single articles can be freely downloaded from the think tank webpage: www.asiamaior.org. Paper version Italy € 50.00 Abroad € 65.00 Subscription [email protected] www.viella.it Editorial board Editor-in-chief (direttore responsabile): Michelguglielmo Torri, University of Turin. Co-editor: Nicola Mocci, University of Sassari. associate editors: Axel Berkofsky, University of Pavia; Diego Maiorano, National University of Singapore, ISAS - Institute of South Asian Studies; Nicola Mocci, University of Sassari; Giulio Pugliese, King’s College London; Michelguglielmo Torri, University of Turin; Elena Valdameri, Swiss Federal Institute of Technology - ETh Zurich; Pierluigi Valsecchi, University of Pavia. -

Nepal's Future: in Whose Hands?
NEPAL’S FUTURE: IN WHOSE HANDS? Asia Report N°173 – 13 August 2009 TABLE OF CONTENTS EXECUTIVE SUMMARY AND RECOMMENDATIONS................................................. i I. INTRODUCTION: THE FRAYING PROCESS ........................................................... 1 II. THE COLLAPSE OF CONSENSUS............................................................................... 2 A. RIDING FOR A FALL......................................................................................................................3 B. OUTFLANKED AND OUTGUNNED..................................................................................................4 C. CONSTITUTIONAL COUP DE GRACE..............................................................................................5 D. ADIEU OR AU REVOIR?................................................................................................................6 III. THE QUESTION OF MAOIST INTENT ...................................................................... 7 A. MAOIST RULE: MORE RAGGED THAN RUTHLESS .........................................................................7 B. THE VIDEO NASTY.......................................................................................................................9 C. THE BEGINNING OF THE END OR THE END OF THE BEGINNING?..................................................11 IV. THE ARMY’S GROWING POLITICAL ROLE ........................................................ 13 A. WAR BY OTHER MEANS.............................................................................................................13 -

Download Publication
No. 43 Working Papers Working Negotiating Between Unequal Neighbours: India‘s Role in Nepal‘s Recent Constitution-Making Process Prakash Bhattarai December 2018 1 Negotiating Between Unequal Neighbours: India’s Role in Nepal’s Recent Constitution-Making Process1 Prakash Bhattarai ABSTRACT Nepal’s post-conflict constitution-making process has seen the involvement of many international actors. While studies on democracy promotion, to this day, mainly focus on Western “donors” and international organizations, this paper looks at the role played by India in the complicated process of moving from a peace agreement to the establishment of an inclusive, democratic constitution in Nepal. More specifically, it is analysed how a powerful neighbouring democracy (India) participated in what is essentially a domestic negotiation process (constitution-making) with a view to influencing the emerging demo- cratic regime. In terms of the issues on the negotiation table, the analysis shows that India, in pushing for an inclusive constitution, pursued the specific agenda of supporting the inclusion of the Madheshis, an ethnic group mostly living in Nepal’s Terai region. In terms of negotiation strategies, the paper identifies four different ways in which India tried to influence the constitution: high-level dialogue; economic blockade; international coalition building; and targeted support of domestic oppositional forces in Nepal. Com- prehensive as this negotiation strategy was, it only met with partial success. Parameters that limited India’s influence included the domestic strength and legitimacy of the official Nepali position (elite alignment; popular support) as well as scepticism concerning In- dia’s role in Nepal, which was reinforced by India’s overly partisan agenda. -

Nepal's Peace Agreement: Making It Work
NEPAL’S PEACE AGREEMENT: MAKING IT WORK Asia Report N°126 – 15 December 2006 TABLE OF CONTENTS EXECUTIVE SUMMARY AND RECOMMENDATIONS................................................. i I. INTRODUCTION .......................................................................................................... 1 II. APRIL AFTERMATH................................................................................................... 2 A. FROM POPULAR PROTEST TO PARLIAMENTARY SUPREMACY ................................................2 B. A FUNCTIONAL GOVERNMENT?..............................................................................................3 C. CONTESTED COUNTRY ...........................................................................................................5 III. THE TALKS ................................................................................................................... 6 A. A ROCKY START...................................................................................................................6 1. Eight-point agreement.................................................................................................6 2. Engaging the UN ........................................................................................................7 3. Mutual suspicion.........................................................................................................8 B. THE STICKING POINTS............................................................................................................8 1. Arms -

The Guards, Cooks, and Cleaners of the Afghan War: Migrant Contractors and the Cost of War
The Guards, Cooks, and Cleaners of the Afghan War: Migrant Contractors and the Cost of War Noah Coburn1 August 23, 2017 Three Years in an Afghan Prison For close to three years in an Afghan prison, Teer Magar, a Nepali laborer, spoke to almost no one.2 His only visitor was a French representative from the Red Cross, who occasionally managed to send some letters home to his wife in Nepal. The few words of Pashto he was able to pick up allowed for limited communication with his guards and fellow inmates, but mostly he kept to himself. During his trial, he had no Nepali translator, and it was difficult for him to plead his case or even understand the charges. It did not seem to bother the other prisoners, mostly Taliban, that he had worked as a contractor for an American construction firm. At one point early in his detention, a large bearded Talib had come to him and demanded that he convert to Islam, Teer recalled. Teer tried to explain to the prisoner that he respected all religions. He wasn’t sure if the Talib understood him, but after a short while, he was left alone. The prison was comfortable and clean by Afghan standards. Newly built by the British, it was one of dozens of structures built for the Afghan government by the international community during the war to house opposition force detainees. It seemed to Teer, however, that most were simply local farmers who had been inadvertently dragged into the conflict, perhaps found with guns in their homes when the Americans went out on raids. -

Compliment to Surya Thapa Siddhi B Ranjitkar
Compliment To Surya Thapa Siddhi B Ranjitkar One of the personalities of the regressive force Surya Bahadur Thapa ultimately died at 87 on Wednesday, April 15, 2015. He was cremated on April 17, 2015 with the full state honor. The government even shut down its business for the state employees to mourn the demise of one of the corrupt politicians. I want him to have a better and progressive life in another world, and be an honorable and respectable human soul there unlike what he had been in this mundane world. He had been a tool of the regressive force. He contributed to shove democracy in a trashcan and put the country in the reverse gear in 1960. He helped to reverse the political development in 1981 again lengthening the life of the corrupt panchayat system. He had earned the reputation of being one of the most corrupt politicians during the 55 years of his political life. Shame on the government and the politicians that gave so much of honor to and respect for the man that had become part of the force that put the majority of the Nepalese in misery, poverty and destitute, and put Nepal into the shameful status of one of the impoverished countries in the world map. If the corrupt politicians were to get so much of honor and respect even after death why the politicians would need to be sincere and honest to the people. Shame on the Nepalese politicians, such a corrupt politician was lionized. On Friday, April 17, 2015, the government of the Federal Democratic Republic of Nepal honored one of the most dishonest politicians of the Nepalese history on his untimely death. -

Nepali Times
www.nepalitimes.com #150 20 - 26 June 2003 16 pages Rs 25 Weekly Internet Poll # 90 Q. Who do you think is primarily responsible for the current state of the nation? One country, two systems Total votes:3,211 Weekly Internet Poll # 91. To vote go to: www.nepalitimes.com Q. If the election were to be held next week, who would you like to see as our next prime minister to lead the country ? MOHAN MAINALI Near Jumla, farmers use the ceasefire to ready terraces for paddy. MOHAN MAINALI two governments. team to conduct a vasectomy camp in firefights this week in Dang and Jajarkot. from JUMLA, KALIKOT and DOLPA ○○○○○ Welcome to ○○○○○○○○○○○○○○○ To be sure, the ceasefire has eased the their village. There have also been instances of Patan Museum Café ts not that the Maoists are lives of most people somewhat. Many It is better. We dont have to worry resistance: some refugee families in Opening from1030 – 1930 hrs everywhere, its just the government is from the outlying villages can now travel anymore about the possibility of getting Kalikot who were prevented from going Enjoy our new Cocktail & Snacks of the nowhere to be seen. relatively unhindered to the main bazar killed while gathering fodder, or fetching back to their villages pelted Maoists with Week from 1700 – 1930 hrs Except for the district headquarters of towns to collect subsidised rice. Some water, says one villager in Dolpa. Were stones at a recent rally. Paru Thapa in For reservations please call these three roadless mid-western districts, farmers have returned to their home just afraid the war may start again. -

Situation Update #59- Coronavirus Disease 2019 (COVID-19) WHO Country Office for Nepal Reporting Date: 25 - 31 May 2021
Situation Update #59- Coronavirus Disease 2019 (COVID-19) WHO Country Office for Nepal Reporting Date: 25 - 31 May 2021 HIGHLIGHTS* SITUATION OVERVIEW ● Of the total COVID-19 positive cases, 79.7% (447,446) of cases have recovered and 18.9% (106470) of cases NEPAL are active. ● Of the total active cases, 93.1% (99,132) of the active (Data as of 01 June 2021, 07:00:00 hours) cases are in home isolation; 6.9% (7,338) cases are 561,302 confirmed cases undergoing hospital/institutional isolation. While 7,386 deaths 1,492 (1.4%) patients require ICU admission, 424 3,057,424 RT-PCR tests (0.3%) of the ICU admitted patients require ventilator support. SOUTH-EAST ASIA REGION ● Forty eight districts have reported more than 500 (Data as of 30 May 2021) active cases. 31,605,221 confirmed cases ● Among the total new cases (40841) reported this 401,754 deaths week, 22.3% (9092) of the new cases are from Kathmandu district and 30.2% (12323) from GLOBAL Kathmandu valley (Kathmandu, Lalitpur and (Data as of 30 May 2021) Bhaktapur districts). 169,604,858 confirmed cases ● RT–PCR tests have been performed from 91 3,530,837 deaths designated COVID-19 laboratories across the country of which 55 are public and 36 are private laboratories. ● There have been 2,113,080 people who have received the 1st dose of COVID-19 Vaccine and 714,163 people have received 2nd dose of COVID-19 vaccine. *Data as of COVID-19 Update, MoHP, 31 May 2021 NEPAL EPIDEMIOLOGICAL SITUATION • As of 1 June 2021, T07:00:00 hours (week no. -
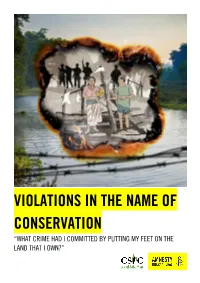
Violations in the Name of Conservation “What Crime Had I Committed by Putting My Feet on the Land That I Own?”
VIOLATIONS IN THE NAME OF CONSERVATION “WHAT CRIME HAD I COMMITTED BY PUTTING MY FEET ON THE LAND THAT I OWN?” Amnesty International is a movement of 10 million people which mobilizes the humanity in everyone and campaigns for change so we can all enjoy our human rights. Our vision is of a world where those in power keep their promises, respect international law and are held to account. We are independent of any government, political ideology, economic interest or religion and are funded mainly by our membership and individual donations. We believe that acting in solidarity and compassion with people everywhere can change our societies for the better. © Amnesty International 2021 Except where otherwise noted, content in this document is licensed under a Creative Commons Cover photo: Illustration by Colin Foo (attribution, non-commercial, no derivatives, international 4.0) licence. Photo: Chitwan National Park, Nepal. © Jacek Kadaj via Getty Images https://creativecommons.org/licenses/by-nc-nd/4.0/legalcode For more information please visit the permissions page on our website: www.amnesty.org Where material is attributed to a copyright owner other than Amnesty International this material is not subject to the Creative Commons licence. First published in 2021 by Amnesty International Ltd Peter Benenson House, 1 Easton Street London WC1X 0DW, UK Index: ASA 31/4536/2021 Original language: English amnesty.org CONTENTS 1. EXECUTIVE SUMMARY 5 1.1 PROTECTING ANIMALS, EVICTING PEOPLE 5 1.2 ANCESTRAL HOMELANDS HAVE BECOME NATIONAL PARKS 6 1.3 HUMAN RIGHTS VIOLATIONS BY THE NEPAL ARMY 6 1.4 EVICTION IS NOT THE ANSWER 6 1.5 CONSULTATIVE, DURABLE SOLUTIONS ARE A MUST 7 1.6 LIMITED POLITICAL WILL 8 2. -

Decisions of the High-Level Coordination Committee for the Prevention and Control of COVID-19 Meeting No
Unofficial translation Decisions of the High-Level Coordination Committee for the Prevention and Control of COVID-19 Meeting no. 12 24 March 2020 Time: 2.00 PM The High-Level Coordination Committee for the Prevention and Control of COVID-19 constituted by the Government of Nepal through its decision of 01 March 2020 under the convenorship of Deputy Prime Minister and Minister for Defence Hon. Mr. Ishwar Pokhrel has taken the following decisions: 1. As the Government of Nepal has been doing all possible for the protection of foreign nationals staying in Nepal during the present COVID-19 Pandemic, request all friendly countries through diplomatic channel for the protection and safety of Nepali nationals in the countries of their residence. Likewise, call upon all Nepali nationals abroad to stay in safety and composure in the countries wherever they are. Nepali diplomatic missions abroad shall inform about the decisions and steps taken by the Government of Nepal to Nepali nationals staying abroad through regular dissemination of information. 2. Allow entry for one time to Nepali nationals who had started their journey before the decision of the Government of Nepal on 22 March 2020 to restrict the movement through international border points effective from 6 a.m. of 24 March 2020 and have arrived at the border points through various land routes and are stranded. Concerned provincial governments and local levels shall arrange mandatory health screening and at put in quarantine for least 14 days for the persons entering Nepal this way. 3. Commence the testing of COVID-19 at the earliest from the laboratories of B.P. -

Nepal's Faltering Peace Process
NEPAL’S FALTERING PEACE PROCESS Asia Report Nº163 – 19 February 2009 TABLE OF CONTENTS EXECUTIVE SUMMARY AND RECOMMENDATIONS .................................................i I. INTRODUCTION .............................................................................................................1 II. CONSENSUS OR CONFLICT? ......................................................................................2 A. WHAT’S LEFT OF THE PEACE PROCESS?.......................................................................................2 B. THE MAOIST-LED GOVERNMENT: IN OFFICE BUT NOT IN POWER? ..............................................3 C. OLD NEPAL: ALIVE AND WELL....................................................................................................5 D. THE RISKS OF FAILURE................................................................................................................6 III. PEACE PARTNERS AT ODDS.......................................................................................8 A. THE MAOISTS: BRINGING ON THE REVOLUTION?.........................................................................8 B. UNCERTAIN COALITION PARTNERS..............................................................................................9 C. THE OPPOSITION: REINVIGORATED, BUT FOR WHAT? ................................................................11 1. The Nepali Congress................................................................................................................. 11 2. The smaller parties ...................................................................................................................