YEAR 1 STUDENT HANDOUT 2015 Contents: 1. Vital Signs 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2015 Korean Guidelines for Cardiopulmonary Resuscitation
Clin Exp Emerg Med 2016;3(S):S1-S9 http://dx.doi.org/10.15441/ceem.16.133 Supplementary Part 1. The update process and eISSN: 2383-4625 highlights: 2015 Korean Guidelines for Cardiopulmonary Resuscitation Sung Oh Hwang1, Sung Phil Chung2, Keun Jeong Song3, Hyun Kim1, Tae Ho Rho4, Kyu Nam Park5, Young-Min Kim5, June Dong Park6, Ai-Rhan Ellen Kim7, Hyuk Jun Yang8 Received: 16 February 2016 Revised: 19 March 2016 1 Department of Emergency Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea Accepted: 19 March 2016 2Department of Emergency Medicine, Yonsei University College of Medicine, Seoul, Korea 3Department of Emergency Medicine, Sungkyunkwan University College of Medicine, Seoul, Korea Correspondence to: Sung Oh Hwang 4Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea Department of Emergency Medicine, 5Department of Emergency Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea 6Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea Yonsei University Wonju College of 7Department of Pediatrics, University of Ulsan College of Medicine, Seoul, Korea Medicine, 20 Ilsan-ro, Wonju 26426, 8Department of Emergency Medicine, Gachon University College of Medicine, Incheon, Korea Korea E-mail: [email protected] THE BACKGROUND AND UPDATE PROCESS OF THE GUIDELINES FOR CARDIOPULMONARY RESUSCITATION 1. The background of the guidelines for cardiopulmonary resuscitation Cardiac arrest can occur inside medical institutions (in-hospital) -

Respiratory Monitoring System Using Thermistor
International Journal of Pure and Applied Mathematics Volume 119 No. 12 2018, 11567-11575 ISSN: 1314-3395 (on-line version) url: http://www.ijpam.eu Special Issue ijpam.eu RESPIRATORY MONITORING SYSTEM USING THERMISTOR 1Gagandeep kour , 2Mohammad Rouman ,Geetha.M3 1,2UG Students, 3Assistant Professor Department of Biomedical Engineering BIHER, BIST, Bharath University Chennai- 6000073. gagandeeplkour. [email protected] Abstract:- respiration is defined as the process of movement of oxygen from the outside air to the cells within tissues and the transport of carbon dioxide in the opposite direction. Respiration can be cellular as well as physiological. In cellular respiration an organism obtains energy in the form of ATP by oxidising nutrients and releasing waste products while as the physiological respiration is necessary to sustain cellular respiration and thus life. Physiological respiration involves ventilation of lungs alveoli with atmospheric air moved into and out of the lungs through inhalation and exhalation, otherwise known as breathing. This project helps to checks the breathing rate of a patient who is suffering from coma, trauma, strokes, seizures at easily accessible levels. The respiratory monitoring system helps to check the breathing rate of a patient with the help of an arduino based system. the main components of this machine are Arduino, thermistor, heart pulse rate sensor, LED, LCD, buzzer alarm, battery. The patient breathes through a mask in which thermistor is placed and then the machine measures the breathing rate. the arduino used here is Arduino UNO(ATmega328 P). Keywords: respiratory device, breathing, Arduino, heart pulse rate sensor, thermistor, alarm. contains 2.5-3.0 litres of air. -

Contents Contents by Condition
Contents Contents by Condition ..................ix Thomas' test .....................54 Foreword ...............................xv Tinel's sign ..........................55 Preface ............................xvi... Trendelenburg's sign ................... 56 Acknowledgements................... XVIII ... True leg length discrepancy (anatomic Authors ...........................xv111 leg length discrepancy) ............... 57 Expert Reviewers ..................... xix Ulnar deviation ...................... 58 Reviewers ..........................xix V-sign ............................. 59 Abbreviations ........................ xx Valgus deformity ..................... 60 Varus deformity ......................63 Chapter 1 Yergason's sign ...................... 65 Musculoskeletal Signs .... Anterior drawer test ...... ........2 Chapter 2 Apley's grind test ......................3 Respiratory Signs ........................71 Apley's scratch test ..................... 4 Apparent leg length inequality (functional Accessory muscle breathing ........................... 73 leg length) ......................... 5 Agonal respiration ......................................... 74 Apprehension test (crank test) .............6 Apneustic breathing (also apneusis) ................ 75 Apprehension-relocation test (Fowler's Apnoea ........................................................ 76 agn) .............................7 Asterixis ........................................................78 Bouchard's and Heberden's nodes ..........8 Asymmetrical chest expansion -

Cardiovascular Assessment
Cardiovascular Assessment A Home study Course Offered by Nurses Research Publications P.O. Box 480 Hayward CA 94543-0480 Office: 510-888-9070 Fax: 510-537-3434 No unauthorized duplication photocopying of this course is permitted Editor: Nurses Research 1 HOW TO USE THIS COURSE Thank you for choosing Nurses Research Publication home study for your continuing education. This course may be completed as rapidly as you desire. However there is a one-year maximum time limit. If you have downloaded this course from our website you will need to log back on to pay and complete your test. After you submit your test for grading you will be asked to complete a course evaluation and then your certificate of completion will appear on your screen for you to print and keep for your records. Satisfactory completion of the examination requires a passing score of at least 70%. No part of this course may be copied or circulated under copyright law. Instructions: 1. Read the course objectives. 2. Read and study the course. 3. Log back onto our website to pay and take the test. If you have already paid for the course you will be asked to login using the username and password you selected when you registered for the course. 4. When you are satisfied that the answers are correct click grade test. 5. Complete the evaluation. 6. Print your certificate of completion. If you have a procedural question or “nursing” question regarding the materials, call (510) 888-9070 for assistance. Only instructors or our director may answer a nursing question about the test. -

Cardiac Arrest Recognition and Telephone CPR by Emergency Medical Dispatchers
OriginalgOdRe Article Cardiac arrest recognition and telephone CPR by emergency medical dispatchers Mark Anthony Attard Biancardi, Peter Spiteri, Maria Pia Pace Abstract Results: The mean percentage recognition of Introduction: Emergency Medical Service out of hospital cardiac arrest by the Maltese EMDs (EMS) systems annually encounters about 275 000 was 67%. 28% of EMDs who recognized cardiac out-of-hospital cardiac arrest (OHCA) patients in arrest asked both questions regarding patient’s Europe and approximately 420,000 cases in the responsiveness and breathing whilst only 8% of United States.1 Survival rates have been reported to EMDs who did not recognize cardiac arrest asked be poor with approximately 10% survival to both questions. The mean percentage of telephone hospital discharge.2 The chance of surviving from assisted CPR was 58%. an OHCA is highly associated with Emergency Conclusion: When compared to other Medical Dispatchers’ (EMD) recognition of cardiac European countries, OHCA recognition by Maltese arrest, early bystander cardiopulmonary EMDs needs to improve. However, given that the resuscitation (CPR), and early defibrillation.3-6 local EMDs have no formal guidelines or Method: This study was a simulation based algorithms for their use during 112 calls, results are study. All emergency nurses who were eligible by encouraging to say the least especially in telephone training to answer 112 calls and activate the EMS assisted CPR. With education and simulation training, were included in this study. The simulations were these numbers should improve run by two experienced ED nurses who followed predefined scripts. The two key questions that the Key Words authors were after included ascertaining patient Emergency Medical Services, Emergency responsiveness and breathing status. -

Dive Medicine Aide-Memoire Lt(N) K Brett Reviewed by Lcol a Grodecki Diving Physics Physics
Dive Medicine Aide-Memoire Lt(N) K Brett Reviewed by LCol A Grodecki Diving Physics Physics • Air ~78% N2, ~21% O2, ~0.03% CO2 Atmospheric pressure Atmospheric Pressure Absolute Pressure Hydrostatic/ gauge Pressure Hydrostatic/ Gauge Pressure Conversions • Hydrostatic/ gauge pressure (P) = • 1 bar = 101 KPa = 0.987 atm = ~1 atm for every 10 msw/33fsw ~14.5 psi • Modification needed if diving at • 10 msw = 1 bar = 0.987 atm altitude • 33.07 fsw = 1 atm = 1.013 bar • Atmospheric P (1 atm at 0msw) • Absolute P (ata)= gauge P +1 atm • Absolute P = gauge P + • °F = (9/5 x °C) +32 atmospheric P • °C= 5/9 (°F – 32) • Water virtually incompressible – density remains ~same regardless • °R (rankine) = °F + 460 **absolute depth/pressure • K (Kelvin) = °C + 273 **absolute • Density salt water 1027 kg/m3 • Density fresh water 1000kg/m3 • Calculate depth from gauge pressure you divide press by 0.1027 (salt water) or 0.10000 (fresh water) Laws & Principles • All calculations require absolute units • Henry’s Law: (K, °R, ATA) • The amount of gas that will dissolve in a liquid is almost directly proportional to • Charles’ Law V1/T1 = V2/T2 the partial press of that gas, & inversely proportional to absolute temp • Guy-Lussac’s Law P1/T1 = P2/T2 • Partial Pressure (pp) – pressure • Boyle’s Law P1V1= P2V2 contributed by a single gas in a mix • General Gas Law (P1V1)/ T1 = (P2V2)/ T2 • To determine the partial pressure of a gas at any depth, we multiply the press (ata) • Archimedes' Principle x %of that gas Henry’s Law • Any object immersed in liquid is buoyed -

A Novel Ebola Virus VP40 Matrix Protein-Based Screening for Identification of Novel Candidate Medical Countermeasures
viruses Communication A Novel Ebola Virus VP40 Matrix Protein-Based Screening for Identification of Novel Candidate Medical Countermeasures Ryan P. Bennett 1,† , Courtney L. Finch 2,† , Elena N. Postnikova 2 , Ryan A. Stewart 1, Yingyun Cai 2 , Shuiqing Yu 2 , Janie Liang 2, Julie Dyall 2 , Jason D. Salter 1 , Harold C. Smith 1,* and Jens H. Kuhn 2,* 1 OyaGen, Inc., 77 Ridgeland Road, Rochester, NY 14623, USA; [email protected] (R.P.B.); [email protected] (R.A.S.); [email protected] (J.D.S.) 2 NIH/NIAID/DCR/Integrated Research Facility at Fort Detrick (IRF-Frederick), Frederick, MD 21702, USA; courtney.fi[email protected] (C.L.F.); [email protected] (E.N.P.); [email protected] (Y.C.); [email protected] (S.Y.); [email protected] (J.L.); [email protected] (J.D.) * Correspondence: [email protected] (H.C.S.); [email protected] (J.H.K.); Tel.: +1-585-697-4351 (H.C.S.); +1-301-631-7245 (J.H.K.) † These authors contributed equally to this work. Abstract: Filoviruses, such as Ebola virus and Marburg virus, are of significant human health concern. From 2013 to 2016, Ebola virus caused 11,323 fatalities in Western Africa. Since 2018, two Ebola virus disease outbreaks in the Democratic Republic of the Congo resulted in 2354 fatalities. Although there is progress in medical countermeasure (MCM) development (in particular, vaccines and antibody- based therapeutics), the need for efficacious small-molecule therapeutics remains unmet. Here we describe a novel high-throughput screening assay to identify inhibitors of Ebola virus VP40 matrix protein association with viral particle assembly sites on the interior of the host cell plasma membrane. -

Microbial Risk Assessment Guideline
EPA/100/J-12/001 USDA/FSIS/2012-001 MICROBIAL RISK ASSESSMENT GUIDELINE PATHOGENIC MICROORGANISMS WITH FOCUS ON FOOD AND WATER Prepared by the Interagency Microbiological Risk Assessment Guideline Workgroup July 2012 Microbial Risk Assessment Guideline Page ii DISCLAIMER This guideline document represents the current thinking of the workgroup on the topics addressed. It is not a regulation and does not confer any rights for or on any person and does not operate to bind USDA, EPA, any other federal agency, or the public. Further, this guideline is not intended to replace existing guidelines that are in use by agencies. The decision to apply methods and approaches in this guideline, either totally or in part, is left to the discretion of the individual department or agency. Mention of trade names or commercial products does not constitute endorsement or recommendation for use. Environmental Protection Agency (EPA) (2012). Microbial Risk Assessment Guideline: Pathogenic Microorganisms with Focus on Food and Water. EPA/100/J-12/001 Microbial Risk Assessment Guideline Page iii TABLE OF CONTENTS Disclaimer .......................................................................................................................... ii Interagency Workgroup Members ................................................................................ vii Preface ............................................................................................................................. viii Abbreviations .................................................................................................................. -
Module 10: Vital Signs
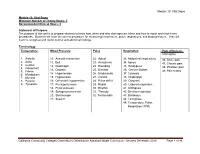
Module 10: Vital Signs Module 10: Vital Signs Minimum Number of Theory Hours: 3 Recommended Clinical Hours: 6 Statement of Purpose: The purpose of this unit is to prepare students to know how, when and why vital signs are taken and how to report and chart these procedures. Students will learn the correct procedure for measuring temperature, pulse, respirations, and blood pressure. They will learn to recognize and report normal and abnormal findings. Terminology: Temperature: Blood Pressure Pulse Respiration Pain (effects on Vital signs) 1. Afebrile 10. Aneroid manometer 22. Apical 33. Abdominal respirations 46. Acute pain 2. Axilla 11. Bell 23. Arrhythmia 34. Apnea 47. Chronic pain 3. Celsius 12. Diaphragm 24. Bounding 35. Bradypnea 4. Fahrenheit 48. Phantom pain 13. Diastolic 25. Brachial 36. Cheyne-Stokes 5. Febrile 49. Pain scales 6. Metabolism 14. Hypertension 26. Bradycardia 37. Cyanosis 7. Mucosa 15. Hypotension 27. Carotid 38. Diaphragm 8. Pyrexia 16. Orthostatic hypotension 28. Pulse deficit 39. Dyspnea 9. Tympanic 17. Pre-hypertension 29. Radial 40. Labored respiration 18. Pulse pressure 30. Rhythm 41. Orthopnea 19. Sphygmomanometer 31. Thready 42. Shallow respiration 20. Stethoscope 32. Tachycardia 43. Stertorous 21. Systolic 44. Tachypnea 45. Temperature, Pulse, Respiration (TPR) Patient, patient/resident, and client are synonymous terms Californiareferring to Community the person Colleges Chancellor’s Office Nurse Assistant Model Curriculum - Revised December 2018 Page 1 of 46 receiving care Module 10: Vital Signs Patient, resident, and client are synonymous terms referring to the person receiving care Performance Standards (Objectives): Upon completion of three (3) hours of class plus homework assignments and six (6) hours of clinical experience, the student will be able to: 1. -

Mod. 3 Vital Signs
Mod. 3 Vital Signs 1. What is most important to assess during secondary assessment? a. Airway b. Pulse c. Respiration d. Chief complaint 2. The first set of vital sign measurements obtained are often referred to as which of the following? a. Baseline vital signs b. Normal vital signs c. Standard vital signs d. None of the above 3. A patient with a pulse rate of 120 beats per minute is considered which of the following? a. Dyscardic b. Normocardic c. Tachycardic d. Bradycardic 4. Where do baseline vital signs fit into the sequence of patient assessment? a. Ongoing assessment b. At primary assessment c. At secondary assessment d. At the patient's side 5. In a conscious adult patient, which of the following pulses should be assessed initially? a. Brachial b. Radial c. Carotid d. Pedal 6. You are assessing a 55-year-old male complaining of chest pain and have determined that his radial pulse is barely palpable. You also determine that there were 20 pulsations over a span of 30 seconds. Based on this, how would you report this patient's pulse? a. Pulse 20, weak, and regular b. Pulse 20 and weak c. Pulse 40 and weak d. Pulse 40, weak, and irregular 7. Which of the following are the vital signs that need to be recorded? a. Pulse, respiration, skin color, skin temperature and condition b. Pulse, respiration, skin color, skin temperature and condition, pupils, blood pressure, and bowel sounds c. Pulse, respiration, skin color, skin temperature and condition, pupils, and blood pressure d. Pulse, respiration, skin color, skin temperature, pupils, and blood pressure 8. -

Terminal Sedation
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Doctoral Dissertations Graduate School 7-2011 Terminal Sedation Karen L Smith [email protected] Follow this and additional works at: https://trace.tennessee.edu/utk_graddiss Part of the Bioethics and Medical Ethics Commons Recommended Citation Smith, Karen L, "Terminal Sedation. " PhD diss., University of Tennessee, 2011. https://trace.tennessee.edu/utk_graddiss/1127 This Dissertation is brought to you for free and open access by the Graduate School at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Doctoral Dissertations by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. To the Graduate Council: I am submitting herewith a dissertation written by Karen L Smith entitled "Terminal Sedation." I have examined the final electronic copy of this dissertation for form and content and recommend that it be accepted in partial fulfillment of the equirr ements for the degree of Doctor of Philosophy, with a major in Philosophy. John Hardwig, Major Professor We have read this dissertation and recommend its acceptance: David Reidy, Glenn Grabor, Nan Gaylord Accepted for the Council: Carolyn R. Hodges Vice Provost and Dean of the Graduate School (Original signatures are on file with official studentecor r ds.) TERMINAL SEDATION A Dissertation Presented for the Doctor of Philosophy Degree The University of Tennessee, Knoxville Karen L. Smith August 2011 Copyright © 2011 by Karen L. Smith All rights reserved. ii ACKNOWLEDGEMENTS There are many people whom I ought to thank for their invaluable assistance to me in completing this dissertation. -

History & Physical Format
History & Physical Format SUBJECTIVE (History) Identification name, address, tel.#, DOB, informant, referring provider CC (chief complaint) list of symptoms & duration. reason for seeking care HPI (history of present illness) - PQRST Provocative/palliative - precipitating/relieving Quality/quantity - character Region - location/radiation Severity - constant/intermittent Timing - onset/frequency/duration PMH (past medical /surgical history) general health, weight loss, hepatitis, rheumatic fever, mono, flu, arthritis, Ca, gout, asthma/COPD, pneumonia, thyroid dx, blood dyscrasias, ASCVD, HTN, UTIs, DM, seizures, operations, injuries, PUD/GERD, hospitalizations, psych hx Allergies Meds (Rx & OTC) SH (social history) birthplace, residence, education, occupation, marital status, ETOH, smoking, drugs, etc., sexual activity - MEN, WOMEN or BOTH CAGE Review Ever Feel Need to CUT DOWN Ever Felt ANNOYED by criticism of drinking Ever Had GUILTY Feelings Ever Taken Morning EYE OPENER FH (family history) age & cause of death of relatives' family diseases (CAD, CA, DM, psych) SUBJECTIVE (Review of Systems) skin, hair, nails - lesions, rashes, pruritis, changes in moles; change in distribution; lymph nodes - enlargement, pain bones , joints muscles - fractures, pain, stiffness, weakness, atrophy blood - anemia, bruising head - H/A, trauma, vertigo, syncope, seizures, memory eyes- visual loss, diplopia, trauma, inflammation glasses ears - deafness, tinnitis, discharge, pain nose - discharge, obstruction, epistaxis mouth - sores, gingival bleeding, teeth,