Certified Surgical Assistant Exam-Study Guide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Single Port Laparoscopic Hysterectomy Through a 12Mm Incision Created by a Bladeless Trocar: a Novel Technique
Single Port Laparoscopic Hysterectomy through a 12mm incision created by a Bladeless Trocar: A Novel Technique Greg J. Marchand, M.D., Katelyn M. Sainz MS1 From the National Foundation for Minimally Invasive Surgery (minvase.org), and Research and Development division of Marchand OBGYN PLLC Precis: Single Port Hysterectomy can be performed safely through a 12mm bladeless incision via this novel technique. Decreasing port size is continually pushing the limits of minimally invasive surgery for enhanced patient outcomes. Corresponding author: Greg J. Marchand M.D., Marchand OBGYN Research and Development, 1520 S. Dobson #218, Mesa, AZ 85202, Tel: 480-628-0566, Fax: 480-999-0801 ABSTRACT Study Objective: The aim of this study is to report the technique used by one surgeon performing a laparoscopic hysterectomy performed through a single 12mm bladeless incision. With the exception of pure vaginal hysterectomy we believe this technique is the least invasive technique published thus far to date where the hysterectomy is performed entirely abdominally. Design: Retrospective Analysis of Charts and Technique Setting: One private Hospital in the Southwest US Patients: 6 patients receiving single port hysterectomy between 2013 and 2014 Intervention: Single Port Laparoscopic Hysterectomy was performed with our ultra-minimally invasive technique, using a Covidien(C) 12mm bladeless laparoscopic trocar followed by an Olympus(C) TriPort device and Olypus(C) articulating 5mm laparoscope without in any way stretching or extending the 12mm port. Other novel aspects of our technique include placement of the single port at the bottom of the umbilicus regardless of patient BMI, the usage of intra-abdominal marcaine to help with postoperative pain and vaginal repair of colpotomy. -

Entry Techniques in Gynecologic Laparoscopy—A Review
Gynecol Surg (2012) 9:139–146 DOI 10.1007/s10397-011-0710-8 REVIEW ARTICLE Entry techniques in gynecologic laparoscopy—a review Johannes Ott & Agnes Jaeger-Lansky & Gunda Poschalko & Regina Promberger & Eleen Rothschedl & René Wenzl Received: 9 June 2011 /Accepted: 19 October 2011 /Published online: 13 November 2011 # Springer-Verlag 2011 Abstract Laparoscopy is one of the most common surgical underpowered in order to assess the risk for rare but life- procedures in gynecologic medicine. Major complications threatening complications. In conclusion, there is no solid associated with gynecologic laparoscopy are relatively rare, evidence proving the superiority of any method of with up to 50% related to laparoscopic entry. Several entry laparoscopic entry. techniques have been developed, all of which aim to provide a safe and easy entry to the abdominal cavity. In Keywords Laparoscopy. Entry techniques . Gynecology. this article, we aim to review the available evidence on Complications . Veress needle . Hasson technique . Direct laparoscopic entry techniques in gynecologic surgery. We trocar entry found no evidence that the Hasson (open) technique is superior to the Veress needle entry, the preferred method of most gynecologists all over the world. When entering the Background abdomen using the Veress needle, an intraperitoneal pressure <10 mmHg is a reliable predictor of correct Laparoscopy is one of the most common surgical intraperitoneal placement. Entry at Palmer’s point (left procedures in gynecologic medicine and has become upper quadrant laparoscopy) is recommended for patients the method of choice over the last few decades for with suspected or known periumbilical adhesions, or a treating benign diseases that require surgery [1, 2]. -
CST-On-Demand-Binder.Pdf
Zander Perioperative Education Zander CST Exam Preparation Course Zander Perioperative Education Certification Preparation for CNOR, CAPA-CPAN, CST and CBSPD Wendy Zander MSN/Ed, RN, CNOR [email protected] Test Taking Strategies Objectives: 1. Apply Test Taking Strategies for the CST exam 2. Create a Personal Study Plan 3. Eligibility • Registering for the exam • Exam Format • Time Management • Test Taking Strategies Eligibility • Current or previously Certified Surgical Technologist (CST) ▫ Evidence of CST Certification • Graduate of a surgical technology program accredited by CAAHEP ▫ Evidence of proof of graduation • Graduate of a surgical technology accredited by ABHES ▫ Evidence of proof of graduation www.periop-ed.com 1 Zander Perioperative Education Military Eligible • A graduate of a military training program in surgical technology is always eligible whether it was before, during or after having CAAHEP accreditation. ▫ a copy of your DD214 (must state location of the base where program was completed), ▫ a copy of your graduation certificate from the surgical technology training program ▫ a smart transcript Accelerated Alternate Delivery (AAD) Pathway • Have on-the-job training in surgical technology • Are a graduate from a surgical technology program that did not hold CAAHEP accreditation during your enrollment CST Testing Fees First Time Test Takers Exam Fee (AST Members) Exam Fee (Non Members) $190 $290 Current or Previous Certified Surgical Technologist Renewing First Time Test Takers Certification by Examination Exam Fee -

Aspiration System and Suction Tip Yankauer
ILE R S E T E T R S I E L Mechanical Irrigation Kits: Physiodispenser and Piezoelectric Surgery 32.F0106.00 Irrigation set 1/2Y Aseptico Aeu 1000 -70/V, Aseptico Aeu 1070-70V 10 pcs 32.F0090.00 Irrigation set 1/2Y Dental Unit Sirona 10 pcs 32.F0019.00 Irrigation set 1/2Y ATR Plus /3000 /5000 10 pcs 32.F0090.00 32.F0106.00 Aspiration System and Suction Tip Yankauer The surgical aspirator with Yankauer suction tip is suitable for all those surgical operations, where an accurate aspiration is needed, so as not to impair the visibility of the operation field. The special nozzles that are placed all around the apical perimeter of the suction tip avoid any accidental suction of small edges of tissue during gingivoplasty. The aspirator is made of medical grade transparent PVC, so as not to absorb the light of shadow-free operating lamps obscuring the surgical site. It is supplied with bending-resistant flexible connectors. Surgical aspirator, 2.50, m with Yankauer suction tip and aspiration control 32.F2044.00 PVC 10 pcs system. (each pack contains 1 adapter Adat. 05) 32.F6361.00 Yankauer sterile suction tip (tip length: 24,5 cm) with aspiration control system PVC 10 pcs 1 Omnia® PTFE Sutures - Black Needle Omnia surgical PTFE sutures are ideal for any implant, periodontal and bone graft surgery where the usage of a monofilament suture with low bacterial adhesion is recommended. Omnia PTFE sutures are soft, biologi- cally inert and chemically non reactive. Compared to other monofilament synthetic sutures, this material is highly tolerated in the oral cavity. -

Comparison Between Different Entry Techniques in Performing Pneumoperitoneum In10.5005/Jp-Journals-10033-1257 Laparoscopic Gynecological Surgery REVIEW ARTICLE
WJOLS Comparison between Different Entry Techniques in Performing Pneumoperitoneum in10.5005/jp-journals-10033-1257 Laparoscopic Gynecological Surgery REVIEW ARTICLE Comparison between Different Entry Techniques in Performing Pneumoperitoneum in Laparoscopic Gynecological Surgery Mandavi Rai ABSTRACT safety of one technique over another. However, the included studies are small and cannot be used to confirm safety of any Background: The main challenge facing the laparoscopic particular technique. No single technique or instrument has surgery is the primary abdominal access, as it is usually a blind been proved to eliminate laparoscopic entry-associated injury. procedure associated with vascular and visceral injuries. Lapa- Proper evaluation of the patient, supported by good surgical roscopy is a very common procedure in gynecology. Complica- skills and reasonably good knowledge of the technology of the tions associated with laparoscopy are often related to entry. instruments remain to be the cornerstone for safe access and The life-threatening complications include injury to the bowel, success in minimal access surgery. bladder, major abdominal vessels, and anterior abdominal- wall vessel. Other less serious complications can also occur, Keywords: Complications, Laparoscopy, Pnumoperitoneum, such as postoperative infection, subcutaneous emphysema Trocar. and extraperitoneal insufflation. There is no clear consensus as to the optimal method of entry into the peritoneal cavity. It How to cite this article: Rai M. Comparison between Dif- has been proved from studies that 50% of laparoscopic major ferent Entry Techniques in Performing Pneumoperitoneum complications occur prior to the commencement of the surgery. in Laparos copic Gynecological Surgery. World J Lap Surg The surgeon must have adequate training and experience in 2015;8(3):101-106. -

Use of the Veress Needle to Obtain Pneumoperitoneum Prior to Laparoscopy
Use of the Veress needle to obtain pneumoperitoneum prior to laparoscopy Consensus statement of the Royal Australian & New Zealand College of Obstetricians & Gynaecologists This statement has been developed by the Women’s (RANZCOG) and the Australasian Gynaecological Health Committee. It has been reviewed by the Endoscopy and Surgery Society (AGES). Endoscopic Surgery Advisory Committee (RANZCOG/AGES) and approved by the Objectives: To provide advice on the use of the RANZCOG Board and Council. Veress needle to obtain pneumoperitoneum prior to laparoscopy. A list of Women’s Health Committee and Endoscopic Surgery Advisory Committee Target audience: Health professionals providing (RANZCOG/AGES) Members can be found in gynaecological care, and patients. Appendix A. Values: The evidence was reviewed by the Disclosure statements have been received from all Endoscopic Surgery Advisory Committee members of this committee. (RANZCOG/AGES), and applied to local factors relating to Australia and New Zealand. Disclaimer This information is intended to provide Background: This statement was first developed by general advice to practitioners. This information Women’s Health Committee in April 1990 and most should not be relied on as a substitute for proper recently reviewed by the Endoscopic Surgery assessment with respect to the particular Committee (RANZCOG/AGES) in July 2017. circumstances of each case and the needs of any patient. This document reflects emerging clinical Funding: The development and review of this and scientific advances as of the date issued and is statement was funded by RANZCOG. subject to change. The document has been prepared having regard to general circumstances. First endorsed by RANZCOG: April 1990 Current: July 2017 Review due: July 2020 1 Table of contents Table of contents ............................................................................................................................ -

CACI Revista 20140228 (2).Indd
ISSN 2250-7531 Colegio Argentino de Cardioangiólogos Intervencionistas CONTIENE ABSTRACTS Revista Argentina de SELECCIONADOS CardioangiologíaSOLACI CACI’14 Intervencionista Enero - Marzo 2014 | Año 5 | Número 1 Artículos Originales Entrenamiento, acreditación y recertifi cación en Cardioan- giología Intervencionista. Veinticinco años de experiencia: 1989-2014 Ruda Vega M, Londero HF, Cherro A Revascularization strategies for patients with multiple ves- sel coronary disease and unprotected left main. A prospec- tive, multicenter and controlled Argentina registry with a co- balt-chromium rapamycin eluting stent, FIREBIRD 2™: Protocol Design and Methods of the ERACI IV Registry Fernández-Pereira C, Santaera O, Larribau M, Haiek C, Sarmiento R, Mie- res J, Lloveras J, Pocoví A, Carlevaro O, Rifourcat I, Chen J, Zheng K, Ro- dríguez-Granillo AM, Antoniucci D, Rodríguez AE; on behalf of ERACI IV Investigators Caso Clínico Bifurcaciones coronarias: técnica stent pull-back modifi cada como estrategia alternativa en pacientes con revascularización previa Dionisio G, Puerta L, Carlevaro O, Kevorkián R, Centeno S Revista Argentina de Cardioangiología Intervencionista Enero - Marzo 2014 | Año 5 | Número 1 Editor en Jefe Marcelo Halac Jorge Leguizamón Eulogio García Traductor Alfredo E. Rodríguez Carlos Miranda Hugo Londero Joan Gómez Alejandro Fernández Pedro Lylyk Editores Asociados Alejandro Peirone Eberhard Grube Representante CACI Esteban Mendaro Liliana Grinfeld Sergio Sierre Luis Guzmán Ernesto M. Torresani Oscar Mendiz Rubén Piraino Pablo Stutzbach Ziyad Hijazi Alejandro Palacios Representante Carrera Antonio Pocoví León Valdivieso Mark Hlatky Juan Parodi Gastón Rodríguez-Granillo Héctor Vetulli Adnan Kastrati UBA-CACI Alfredo E. Rodríguez Gregg Stone José Vicario Kem Morton Guillermo Migliaro Jorge Wisner Omar Santaera Consejo de Redacción Carlos Sztejfman Pedro Lemos Relaciones José Alonso Secretaría Científi ca Alberto Tamashiro Carlos Macaya Institucionales CACI Rosana Ceratto Carla Agatiello David Vetcher Roxana Mehran Lic. -

Chargemaster
Charge Code Description Price Medicare CPT 400481 OR 481 TO 540 MIN 9100 SURG 400777 SUTURES-RUN 92 400778 SUTURE-POP OFF 128 400779 SUTURE-REEL 33 400780 SUTURE-TIES 84 440002 STALEVO 150 11.2 3000817 PNEUM VACCINE ADMINI 57 G0009 3000819 CA SCREEN; PELVIC/BR 103 G0101 3000823 COLORECTAL SCR SCOPE 1030 G0105 3001087 APPLICATION FOREARM 200 29085 3001104 TECH COMP EXC DEB 42 376 11042 3001297 HIPPS 0 MANUL 3001740 CENTRAL VENOUS LINE 1500 36556 3001741 TECH COMP REPLACMENT 1500 36580 3001742 TECH COMP REMOVAL HI 1000 36589 3001745 TECH COMP GASTROSTOM 325 3001746 TECH COMP I&D SCROTA 1700 55100 3001913 PRIVATE ROOM W/BATH 982 3002874 SEMI-PRIVATE 960 3002879 TECH COMP TUBE THORA 900 32551 3002882 TECH COMP REPLACEMEN 1500 36580 3003298 CVP TECHNICAL COMPON 1500 36556 3003882 ADMIN BLD/BLD PRDUCT 565 36430 3004250 TECH COMP INS ART LN 515 36245 3004251 CVP TECHNICAL COMPON 1500 36556 3004253 TECH COMP REPLACEMEN 1500 36580 3004256 TECH COMP BX 45100 3300 45100 3004259 TECH COMP PARACENTES 815 49082 3004261 INSERTION TEMP BLADD 200 51702 3004263 DILATION URETHRA SUB 275 53621 3004264 TECH COMP DILATION U 150 53661 3004538 NURSERY/SICK BABY 450 3004850 TREATMENT ROOM LVL 1 150 99211 3004853 TREATMENT RM LVL 3 250 99213 3004995 TECH COMP PARA REPEA 815 49082 3005022 OBS DIRECT ADMIT 1ST 600 G0379 3005110 SWING BED 441 3005209 OBSERV RM. EACH HR 50 G0378 3005845 INJ INTRA-A THERAPEU 200 96373 3005933 IMMUN ADMIN ONE VACC 53 90471 3005938 IV INF HYDRATION INI 215 96360 3005939 IV INF HYDRATION EAC 65 96361 3005940 IV INF THER PROPH DI 300 96365 -

AUA BLUS Handbook of Laparoscopic and Robotic Fundamentals
AUA BLUS Handbook of Laparoscopic and Robotic Fundamentals Sean Collins, Daniel S. Lehman, Elspeth M. McDougall, Ralph V. Clayman, and Jaime Landman ©American Urological Association Education & Research, Inc. Table of Contents 1. Introduction 2. Patient selection a. Indication b. contradindications c. special considerations 3. Physiologic effects of pneumoperitoneum a. Renal surgery transperitoneal b. Renal surgery retroperitoneal c. Hand-assisted laparoscopic nephrectomy d. Prostatectomy 4. Getting Started 5. Patient positioning a. Renal surgery transperitoneal b. Renal surgery retroperitoneal c. Hand-assisted laparoscopic nephrectomy d. Prostatectomy 6. Strategic placement of surgical team and operating room (OR) equipment 7. Access a. Primary access b. Renal surgery transperitoneal trocar placement c. Renal surgery retroperitoneal trocar placement d. Secondary access e. Retroperitoneal primary and secondary access f. Hand-assisted laparoscopic nephrectomy trocar placement g. Prostatectomy trocar placement 8. Instrumentation a. Trocars i. Cutting ii. Dilating iii. Radially dilating b. Bipolar cautery c. Monopolar cautery d. Ultrasonic instrumentation e. Vessel sealing devices i. LigaSure ii. Enseal f. Staplers g. Vascular clamps h. Suture anchors i. Titanium clips j. Locking clips q. Retractors r. Hemostatic agents s. Hand Assisted devices 2 9. Technique for Transperitoneal Laparoscopic Nephrectomy 10. Complications of laparoscopic surgery 3 Chapter 1. Introduction The American Urological Association (AUA) has prepared this handbook for all those new to laparoscopy. Rather than being a detailed surgical atlas, this is a handbook designed to introduce the fundamental principles of laparoscopy including: indications and contraindications for laparoscopy, the physiologic effects of pneumoperitoneum, patient positioning; abdominal access and trocar placement; strategic placement of the operating room (OR) team and equipment, overview of laparoscopic instrumentation, and complications unique to laparoscopic surgery. -

Trends of Increasing Medical Radiation Exposure in a Population Hospitalized for Cardiovascular Disease (1970–2009)
Trends of Increasing Medical Radiation Exposure in a Population Hospitalized for Cardiovascular Disease (1970–2009) Clara Carpeggiani*, Patrizia Landi, Claudio Michelassi, Paolo Marraccini, Eugenio Picano CNR, Institute of Clinical Physiology, Pisa, Italy Abstract Background: High radiation doses employed in cardiac imaging may increase cancer frequency in exposed patients after decades. The aim of this study was to evaluate the relative trends in medical radiation exposure in a population hospitalized for cardiovascular disease. Methods and Results: An observational single-center study was conducted to examine 16,431 consecutive patients with heart disease admitted to the Italian National Research Council Institute of Clinical Physiology between January 1970 and December 2009. In all patients, the cumulative estimated effective dose was obtained from data mining of electronic records of hospital admissions, adopting the effective dose typical values of the American Heart Association 2009 statement and Mettler’s 2008 catalog of doses. Cumulative estimated effective dose per patient in the last 5 years was 22 (12–42) mSv (median, 25th–75th percentiles), with higher values in ischemic heart disease (IHD), 37 (20–59) vs non-IHD, 13 (8–22) mSv, p,0.001. Trends in radiation exposure showed a steady increase in IHD and a flat trend in non-IHD patients, with variation from 1970–74 to 2005–2009 of +155% for IHD (p,0.001) and 21% in non-IHD (NS). The relative contribution of different imaging techniques was remodeled over time, with nuclear cardiology dominating in 1970s (23% of individual exposure) and invasive fluoroscopy in the last decade (90% of individual exposure). Conclusion: A progressive increase in cumulative estimated effective dose is observed in hospitalized IHD patients. -

Bone Forceps and Rongeurs
Bone Forceps and Rongeurs Zepf Bone Forceps and Preferred by both neurosurgeons and Rongeurs have double action joints orthopaedic surgeons. that allow a surgeon to use one hand to cut bone with ease and precision. Unique shape of rongeurs allows for no blocking of the field of vision. Secured with screws which allows instrument to be sharpened or repaired Long history of genuine reliability. as needed. Page 10 Zepf Bone Forceps and Rongeurs 35-6401 PLIERS W/SIDE CUT, WIDE JAW 8. 35-6504 LEWIN BONE HOLDING FORCEPS 7” 35-6508-18 VERBRUGGE BONE HOLD. FORCEPS 7” 35-6513 LANE BONE HOLDING FORCEPS 13” 35-6544 FARABEUF BONE HOLDING FORCEPS 10” 35-6554 KLEINERT-KUTZ BONE CUTTING FORCEPS 6” 35-6562 LISTON BONE CUTTING FORCEPS STR 7.5” 35-6566 LISTON BONE CUTTING FORCEPS STR 10.5” 35-6567 LISTON BONE CUTTING FORCEPS ANGLED 10.75” 35-6570 KLEINERT-KUTZ BONE RONGEUR CRV 5.25” 35-6571 KLEINERT-KUTZ RONGEUR STRONG CRV 5.25” 35-6579-16 LEMPERT BONE RONGEUR CVD.6.25” 35-6579-19 LEMPERT BONE RONGEUR 7.5” 35-6583 BEYER BONE RONGEUR 7” 35-6587-15 KLEINERT-KUTZ BONE RONGEUR 6” 35-6587-18 KLEINERT-KUTZ BONE RONGEUR 7” 35-6590 BEYER BONE RONGEUR 7.25” STR. 35-6591 BEYER BONE RONGEUR 7.25” CVD. 35-6595 ZAUFAL-JANSEN BONE RONGEUR 7” CRV 35-6600 MARQUARDT BONE RONGEUR 8” CRV 35-6604 LUER BONE RONGEUR 8.75” STR. 35-6606 LUER BONE RONGEUR 8.75” curved 35-6610-1 LEKSELL BONE RONGEUR 9.5 SLY CRV WIDE 35-6610-2 LEKSELL BONE RONGEUR 9.5” SLY CRV NARROW 35-6612 STILLE-LUER DUCKBILL RONGEUR 9.5” 35-6612-1 LEKSELL BONE RONGEUR 9.5” WIDE 35-6612-2 LEKSELL BONE RONGEUR 9.5” NARROW 35-7956-3 SELVERSTONE LAMINECTOMY RONGEUR 6” 2X3MM 35-7956-5 SELVERSTONE LAMINECTOMY RONGEUR 6” 2X5MM 35-7960-4 SCHLESINGER LAMINECTOMY RONGEUR 6” 35-7964 CUSHING LAMINECTOMY RONGEUR 6” CRV UP 35-7983 FERRIS-SMITH LAMINECTOMY RONGEUR 7” STR 35-8004-2 SPURLING-KERRISON LAMINECTOMY PUNCH 7” 35-8008-5 SPURLING-KERRISON LAMINECTOMY PUNCH 7” SURGICAL INSTRUMENTS, INC. -
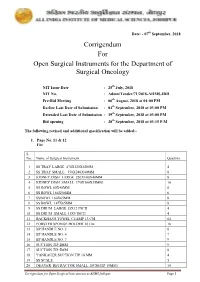
Corrigendum for Open Surgical Instruments for the Department Of
Date: - 07th September, 2018 Corrigendum For Open Surgical Instruments for the Department of Surgical Oncology NIT Issue Date : 25th July, 2018 NIT No. : Admn/Tender/71/2018-AIIMS.JDH Pre-Bid Meeting : 06th August, 2018 at 04:00 PM Earlier Last Date of Submission : 04th September, 2018 at 03:00 PM Extended Last Date of Submission : 19th September, 2018 at 03:00 PM Bid opening : 20th September, 2018 at 03:15 P.M The following revised and additional specification will be added:- 1. Page No. 11 & 12 For S. No. Name of Surgical Instrument Quantity 1 SS TRAY LARGE 470X320X50MM 4 2 SS TRAY SMALL 350X240X40MM 8 3 KIDNEY DISH LARGE 250X140X40MM 8 4 KIDNEY DISH SMALL 170X100X35MM 10 5 SS BOWL 80X40MM 6 6 SS BOWL 166X50MM 6 7 SSBOWL 160X65MM 8 8 SS BOWL 147X65MM 8 9 SS DRUM LARGE 15X12 INCH 4 10 SS DRUM SMALL 11X9 INCH 4 11 BACKHAUS TOWEL CLAMP 13 CM 64 12 FORSTER SPONGE HOLDER 18 Cm 18 13 BP HANDLE NO. 3 8 14 BP HANDLE NO. 4 7 15 BP HANDLE NO. 7 9 16 SUCTION TIP 2MM 9 17 SUCTION TIP 5MM 8 18 YANKAUER SUCTION TIP 10 MM 4 19 SS SCALE 5 20 DEAVER RETRACTOR SMALL 18CM(TIP 19MM) 14 Corrigendum for Open Surgical Instruments at AIIMS Jodhpur Page 1 21 DEAVER RETRACTOR MEDIUM 30.5CM (TIP 25 MM) 10 22 DEAVER RETRACTOR LARGE 31.5CM (TIP 50MM) 10 23 DOYEN’S RETRACTOR 4 24 MORRIS RETRACTOR 25cm ( BLADE 7x4cm) 6 25 SKIN HOOK 32 26 LANGENBECK RETRACTOR SMALL 16cm (TIP 21x 8mm) 16 27 LANGENBECK RETRACTOR MEDIUM 22cm (TIP 50x11mm) 16 28 LANGENBECK RETRACTOR LARGE 22.5cm (TIP 85x15mm) 14 29 C ZERNY RETRACTOR 17.2 cm 14 30 VEIN RETRACTOR 18 31 BALFOUR ABDOMINAL RETRACTOR 20cm 3 32 MASTOID RETRACTOR 4 33 PERIOSTEUM ELEVATOR SHARP 4 34 PERIOSTEUM ELEVATOR BLUNT 4 35 DISSECTING TOOTH FORCEPS 15 CM 16 36 DISSECTING PLAIN FORCEPS 18 CM 16 37 ARTERY FORCEPS CVD 15 CM 36 38 ARTERY FORCEPS ST.