Bioactive Alkaloids from Medicinal Plants of Bhutan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Molecular Genetic Characteristics of Nepalese Ephedra Plants (Ephedraceae)
J. Jpn. Bot. 86: 303–313 (2011) Molecular Genetic Characteristics of Nepalese Ephedra Plants (Ephedraceae) a a a Emi HAMANAKA , Keisuke OHKUBO , Masayuki MIKAGE and Nobuko b, KAKIUCHI * a Graduate School of Natural Science and Technology, Kanazawa University, Kakuma-machi, Kanazawa, 920-1192 JAPAN b Department of Pharmacognosy, School of Pharmaceutical Sciences, Kyusyu University of Health and Welfare, 1714-1, Yoshino-cho, Nobeoka, 882-8508 JAPAN * Corresponding author: [email protected] (Accepted on June 28, 2011) The aerial part of Ephedra plants is a staple crude drug worldwide. With the aim of developing new Ephedra resources, we investigated Nepalese wild Ephedra plants, E. gerardiana Wall. ex Stapf and E. pachyclada Boiss., and analyzed their molecular genetic features by DNA analysis. Ephedra gerardiana were distributed on the sub-Himalayan steppes at high altitudes, 3100–4500 m, and E. pachyclada were found along the Kali Gandaki River Valley in the Mustang region at relatively lower altitudes, 2000–3500 m. Ephedra gerardiana specimens from western collection sites shared an identical ITS1 sequence, while that of specimens from eastern collection sites at higher altitudes was 1–12 bases different from western specimens. Ephedra pachyclada specimens showed complex ITS1 signals by the overlapping of two type sequences. By cloning of ITS1 sequences of four E. pachyclada specimens from around the 400th nucleotide to separate these overlapping sequences, they were confirmed to contain sequences either monophyletic with E. intermedia Schrenk & C. A. Mey. or E. gerardiana. The ratio of clones with these two types varied among the specimens. Both Nepalese Ephedra plants, especially E. pachyclada, had a markedly heterogeneous ITS1 sequence that may be caused by harsh environmental pressure at high altitudes. -
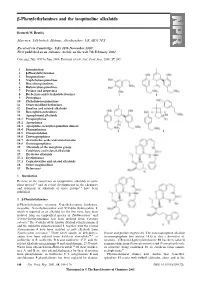
Β-Phenylethylamines and the Isoquinoline Alkaloids
-Phenylethylamines and the isoquinoline alkaloids Kenneth W. Bentley Marrview, Tillybirloch, Midmar, Aberdeenshire, UK AB51 7PS Received (in Cambridge, UK) 28th November 2000 First published as an Advance Article on the web 7th February 2001 Covering: July 1999 to June 2000. Previous review: Nat. Prod. Rep., 2000, 17, 247. 1 Introduction 2 -Phenylethylamines 3 Isoquinolines 4 Naphthylisoquinolines 5 Benzylisoquinolines 6 Bisbenzylisoquinolines 7 Pavines and isopavines 8 Berberines and tetrahydoberberines 9 Protopines 10 Phthalide-isoquinolines 11 Other modified berberines 12 Emetine and related alkaloids 13 Benzophenanthridines 14 Aporphinoid alkaloids 14.1 Proaporphines 14.2 Aporphines 14.3 Aporphine–benzylisoquinoline dimers 14.4 Phenanthrenes 14.5 Oxoaporphines 14.6 Dioxoaporphines 14.7 Aristolochic acids and aristolactams 14.8 Oxoisoaporphines 15 Alkaloids of the morphine group 16 Colchicine and related alkaloids 17 Erythrina alkaloids 17.1 Erythrinanes 17.2 Cephalotaxine and related alkaloids 18 Other isoquinolines 19 References 1 Introduction Reviews of the occurrence of isoquinoline alkaloids in some plant species 1,2 and of recent developments in the chemistry and synthesis of alkaloids of these groups 3–6 have been published. 2 -Phenylethylamines β-Phenylethylamine, tyramine, N-methyltyramine, hordenine, mescaline, N-methylmescaline and N,N-dimethylmescaline 1, which is reported as an alkaloid for the first time, have been isolated from an unspecified species of Turbinocarpus 7 and N-trans-feruloyltyramine has been isolated from Cananga odorata.8 The N-oxides of the known alkaloid culantraramine 2 and the unknown culantraraminol 3, together with the related avicennamine 4 have been isolated as new alkaloids from Zanthoxylum avicennae.9 Three novel amides of dehydrotyr- leucine and proline respectively. -

Next-Generation Sequencing Identification and Characterization
Next-generation sequencing identification and characterization of microsatellite markers in Aconitum austrokoreense Koidz., an endemic and endangered medicinal plant of Korea Y.-E. Yun, J.-N. Yu, G.H. Nam, S.-A. Ryu, S. Kim, K. Oh and C.E. Lim National Institute of Biological Resources, Environmental Research Complex, Incheon, Korea Corresponding author: C.E. Lim E-mail: [email protected] Genet. Mol. Res. 14 (2): 4812-4817 (2015) Received June 11, 2014 Accepted October 29, 2014 Published May 11, 2015 DOI http://dx.doi.org/10.4238/2015.May.11.13 ABSTRACT. We used next-generation sequencing to develop 9 novel microsatellite markers in Aconitum austrokoreense, an endemic and endangered medicinal plant in Korea. Owing to its very limited distribution, over-harvesting for traditional medicinal purposes, and habitat loss, the natural populations are dramatically declining in Korea. All novel microsatellite markers were successfully genotyped using 64 samples from two populations (Mt. Choejeong, Gyeongsangbuk- do and Ungseokbong, Gyeongsangnam-do) of Gyeongsang Province. The number of alleles ranged from 2 to 7 per locus in each population. Observed and expected heterozygosities ranged from 0.031 to 0.938 and from 0.031 to 0.697, respectively. The novel markers will be valuable tools for assessing the genetic diversity of A. austrokoreense and for germplasm conservation of this endangered species. Key words: Aconitum austrokoreense; Microsatellite marker; Endemic and endangered medicinal plant, Next-generation sequencing; Genetic diversity Genetics and Molecular Research 14 (2): 4812-4817 (2015) ©FUNPEC-RP www.funpecrp.com.br Novel microsatellite markers in A. austrokoreense 4813 INTRODUCTION Aconitum austrokoreense Koidz. -

1. Introduction
Introduction 1. Introduction 1.1. Alkaloids The term alkaloid is derived from Arabic word al-qali, the plant from which “soda” was first obtained (Kutchan, 1995). Alkaloids are a group of naturally occurring low-molecular weight nitrogenous compounds found in about 20% of plant species. The majority of alkaloids in plants are derived from the amino acids tyrosine, tryptophan and phenylalanine. They are often basic and contain nitrogen in a heterocyclic ring. The classification of alkaloids is based on their carbon-nitrogen skeletons; common alkaloid ring structures include the pyridines, pyrroles, indoles, pyrrolidines, isoquinolines and piperidines (Petterson et al., 1991; Bennett et al., 1994). In nature, plant alkaloids are mainly involved in plant defense against herbivores and pathogens. Many of these compounds have biological activity which makes them suitable for use as stimulants (nicotine, caffeine), pharmaceuticals (vinblastine), narcotics (cocaine, morphine) and poisons (tubocurarine). The discovery of morphine by the German pharmacist Friedrich W. Sertürner in 1806 began the field of plant alkaloid biochemistry. However, the structure of morphine was not determined until 1952 due to its stereochemical complexity. Major technical advances occurred in this field allowing for the elucidation of selected alkaloid biosynthetic pathways. Among these were the introduction of radiolabeled precursors in the 1950s and the establishment in the 1970s of plant cell suspension cultures as an abundant source of enzymes that could be isolated, purified and characterized. Finally, the introduction of molecular techniques has made possible the isolation of genes involved in alkaloid secondary pathways (Croteau et al., 2000; Facchini, 2001). 1.1.1. Benzylisoquinoline alkaloids Isoquinoline alkaloids represent a large and varied group of physiologically active natural products. -

A Systematic Review on Main Chemical Constituents of Papaver Bracteatum
Journal of Medicinal Plants A Systematic Review on Main Chemical Constituents of Papaver bracteatum Soleymankhani M (Ph.D. student), Khalighi-Sigaroodi F (Ph.D.)*, Hajiaghaee R (Ph.D.), Naghdi Badi H (Ph.D.), Mehrafarin A (Ph.D.), Ghorbani Nohooji M (Ph.D.) Medicinal Plants Research Center, Institute of Medicinal Plants, ACECR, Karaj, Iran * Corresponding author: Medicinal Plants Research Center, Institute of Medicinal Plants, ACECR, P.O.Box: 33651/66571, Karaj, Iran Tel: +98 - 26 - 34764010-9, Fax: +98 - 26-34764021 E-mail: [email protected] Received: 17 April 2013 Accepted: 12 Oct. 2014 Abstract Papaver bracteatum Lindly (Papaveraceae) is an endemic species of Iran which has economic importance in drug industries. The main alkaloid of the plant is thebaine which is used as a precursor of the semi-synthetic and synthetic compounds including codeine and naloxone, respectively. This systematic review focuses on main component of Papaver bracteatum and methods used to determine thebaine. All studies which assessed the potential effect of the whole plant or its extract on clinical or preclinical studies were reviewed. In addition, methods for determination of the main components, especially thebaine, which have been published from 1948 to March 2013, were included. Exclusion criteria were agricultural studies that did not assess. This study has listed alkaloids identified in P. bracteatum which reported since 1948 to 2013. Also, the biological activities of main compounds of Papaver bracteatum including thebaine, isothebaine, (-)-nuciferine have been reviewed. As thebaine has many medicinal and industrial values, determination methods of thebaine in P. bracteatum were summarized. The methods have being used for determination of thebaine include chromatographic (HPLC, GC and TLC) and non chromatographic methods. -

Dr. Duke's Phytochemical and Ethnobotanical Databases Chemicals Found in Papaver Somniferum
Dr. Duke's Phytochemical and Ethnobotanical Databases Chemicals found in Papaver somniferum Activities Count Chemical Plant Part Low PPM High PPM StdDev Refernce Citation 0 (+)-LAUDANIDINE Fruit -- 0 (+)-RETICULINE Fruit -- 0 (+)-RETICULINE Latex Exudate -- 0 (-)-ALPHA-NARCOTINE Inflorescence -- 0 (-)-NARCOTOLINE Inflorescence -- 0 (-)-SCOULERINE Latex Exudate -- 0 (-)-SCOULERINE Plant -- 0 10-HYDROXYCODEINE Latex Exudate -- 0 10-NONACOSANOL Latex Exudate Chemical Constituents of Oriental Herbs (3 diff. books) 0 13-OXOCRYPTOPINE Plant -- 0 16-HYDROXYTHEBAINE Plant -- 0 20-HYDROXY- Fruit 36.0 -- TRICOSANYLCYCLOHEXA NE 0 4-HYDROXY-BENZOIC- Pericarp -- ACID 0 4-METHYL-NONACOSANE Fruit 3.2 -- 0 5'-O- Plant -- DEMETHYLNARCOTINE 0 5-HYDROXY-3,7- Latex Exudate -- DIMETHOXYPHENANTHRE NE 0 6- Plant -- ACTEONLYDIHYDROSANG UINARINE 0 6-METHYL-CODEINE Plant Father Nature's Farmacy: The aggregate of all these three-letter citations. 0 6-METHYL-CODEINE Fruit -- 0 ACONITASE Latex Exudate -- 32 AESCULETIN Pericarp -- 3 ALANINE Seed 11780.0 12637.0 0.5273634907250652 -- Activities Count Chemical Plant Part Low PPM High PPM StdDev Refernce Citation 0 ALKALOIDS Latex Exudate 50000.0 250000.0 ANON. 1948-1976. The Wealth of India raw materials. Publications and Information Directorate, CSIR, New Delhi. 11 volumes. 5 ALLOCRYPTOPINE Plant Father Nature's Farmacy: The aggregate of all these three-letter citations. 15 ALPHA-LINOLENIC-ACID Seed 1400.0 5564.0 -0.22115561650586155 -- 2 ALPHA-NARCOTINE Plant Jeffery B. Harborne and H. Baxter, eds. 1983. Phytochemical Dictionary. A Handbook of Bioactive Compounds from Plants. Taylor & Frost, London. 791 pp. 17 APOMORPHINE Plant Father Nature's Farmacy: The aggregate of all these three-letter citations. 0 APOREINE Fruit -- 0 ARABINOSE Fruit ANON. -

Modulation of Ion Channels by Natural Products ‒ Identification of Herg Channel Inhibitors and GABAA Receptor Ligands from Plant Extracts
Modulation of ion channels by natural products ‒ Identification of hERG channel inhibitors and GABAA receptor ligands from plant extracts Inauguraldissertation zur Erlangung der Würde eines Doktors der Philosophie vorgelegt der Philosophisch-Naturwissenschaftlichen Fakultät der Universität Basel von Anja Schramm aus Wiedersbach (Thüringen), Deutschland Basel, 2014 Original document stored on the publication server of the University of Basel edoc.unibas.ch This work is licenced under the agreement „Attribution Non-Commercial No Derivatives – 3.0 Switzerland“ (CC BY-NC-ND 3.0 CH). The complete text may be reviewed here: creativecommons.org/licenses/by-nc-nd/3.0/ch/deed.en Genehmigt von der Philosophisch-Naturwissenschaftlichen Fakultät auf Antrag von Prof. Dr. Matthias Hamburger Prof. Dr. Judith Maria Rollinger Basel, den 18.02.2014 Prof. Dr. Jörg Schibler Dekan Attribution-NonCommercial-NoDerivatives 3.0 Switzerland (CC BY-NC-ND 3.0 CH) You are free: to Share — to copy, distribute and transmit the work Under the following conditions: Attribution — You must attribute the work in the manner specified by the author or licensor (but not in any way that suggests that they endorse you or your use of the work). Noncommercial — You may not use this work for commercial purposes. No Derivative Works — You may not alter, transform, or build upon this work. With the understanding that: Waiver — Any of the above conditions can be waived if you get permission from the copyright holder. Public Domain — Where the work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license. -

Diversity of the Mountain Flora of Central Asia with Emphasis on Alkaloid-Producing Plants
diversity Review Diversity of the Mountain Flora of Central Asia with Emphasis on Alkaloid-Producing Plants Karimjan Tayjanov 1, Nilufar Z. Mamadalieva 1,* and Michael Wink 2 1 Institute of the Chemistry of Plant Substances, Academy of Sciences, Mirzo Ulugbek str. 77, 100170 Tashkent, Uzbekistan; [email protected] 2 Institute of Pharmacy and Molecular Biotechnology, Heidelberg University, Im Neuenheimer Feld 364, 69120 Heidelberg, Germany; [email protected] * Correspondence: [email protected]; Tel.: +9-987-126-25913 Academic Editor: Ipek Kurtboke Received: 22 November 2016; Accepted: 13 February 2017; Published: 17 February 2017 Abstract: The mountains of Central Asia with 70 large and small mountain ranges represent species-rich plant biodiversity hotspots. Major mountains include Saur, Tarbagatai, Dzungarian Alatau, Tien Shan, Pamir-Alai and Kopet Dag. Because a range of altitudinal belts exists, the region is characterized by high biological diversity at ecosystem, species and population levels. In addition, the contact between Asian and Mediterranean flora in Central Asia has created unique plant communities. More than 8100 plant species have been recorded for the territory of Central Asia; about 5000–6000 of them grow in the mountains. The aim of this review is to summarize all the available data from 1930 to date on alkaloid-containing plants of the Central Asian mountains. In Saur 301 of a total of 661 species, in Tarbagatai 487 out of 1195, in Dzungarian Alatau 699 out of 1080, in Tien Shan 1177 out of 3251, in Pamir-Alai 1165 out of 3422 and in Kopet Dag 438 out of 1942 species produce alkaloids. The review also tabulates the individual alkaloids which were detected in the plants from the Central Asian mountains. -

Review Article SOME PLANTS AS a SOURCE of ACETYL CHOLINESTERASE INHIBITORS: a REVIEW Purabi Deka *, Arun Kumar, Bipin Kumar Nayak, N
Purabi Deka et al. Int. Res. J. Pharm. 2017, 8 (5) INTERNATIONAL RESEARCH JOURNAL OF PHARMACY www.irjponline.com ISSN 2230 – 8407 Review Article SOME PLANTS AS A SOURCE OF ACETYL CHOLINESTERASE INHIBITORS: A REVIEW Purabi Deka *, Arun Kumar, Bipin Kumar Nayak, N. Eloziia Division of Pharmaceutical Sciences, Shri Guru Ram Rai Institute of Technology & Science, Dehradun, India *Corresponding Author Email: [email protected] Article Received on: 27/03/17 Approved for publication: 27/04/17 DOI: 10.7897/2230-8407.08565 ABSTRACT The term dementia derives from the Latin demens (“de” means private, “mens” means mind, intelligence and judgment- “without a mind”). Dementia is a progressive, chronic neurological disorder which destroys brain cells and causes difficulties with memory, behaviour, thinking, calculation, comprehension, language and it is brutal enough to affect work, lifelong hobbies, and social life. Alzheimer’s disease, Parkinson’s disease, Dementia with Lewys Bodies are some common types of dementias. Acetylcholinesterase AChE) Inhibition, the key enzyme which plays a main role in the breakdown of acetylcholine and it is considered as a Positive strategy for the treatment of neurological disorders. Currently many AChE inhibitors namely tacrine, donepezil, rivastigmine, galantamine have been used as first line drug for the treatment of Alzheimer’s disease. They are having several side effects such as gastrointestinal disorder, hepatotoxicity etc, so there is great interest in finding new and better AChE inhibitors from Natural products. Natural products are the remarkable source of Synthetic as well as traditional products. Abundance of plants in nature gives a potential source of AChE inhibitors. The purpose of this article to present a complete literature survey of plants that have been tested for AChE inhibitory activity. -
Analytical Reference Standards
Cerilliant Quality ISO GUIDE 34 ISO/IEC 17025 ISO 90 01:2 00 8 GM P/ GL P Analytical Reference Standards 2 011 Analytical Reference Standards 20 811 PALOMA DRIVE, SUITE A, ROUND ROCK, TEXAS 78665, USA 11 PHONE 800/848-7837 | 512/238-9974 | FAX 800/654-1458 | 512/238-9129 | www.cerilliant.com company overview about cerilliant Cerilliant is an ISO Guide 34 and ISO 17025 accredited company dedicated to producing and providing high quality Certified Reference Standards and Certified Spiking SolutionsTM. We serve a diverse group of customers including private and public laboratories, research institutes, instrument manufacturers and pharmaceutical concerns – organizations that require materials of the highest quality, whether they’re conducing clinical or forensic testing, environmental analysis, pharmaceutical research, or developing new testing equipment. But we do more than just conduct science on their behalf. We make science smarter. Our team of experts includes numerous PhDs and advance-degreed specialists in science, manufacturing, and quality control, all of whom have a passion for the work they do, thrive in our collaborative atmosphere which values innovative thinking, and approach each day committed to delivering products and service second to none. At Cerilliant, we believe good chemistry is more than just a process in the lab. It’s also about creating partnerships that anticipate the needs of our clients and provide the catalyst for their success. to place an order or for customer service WEBSITE: www.cerilliant.com E-MAIL: [email protected] PHONE (8 A.M.–5 P.M. CT): 800/848-7837 | 512/238-9974 FAX: 800/654-1458 | 512/238-9129 ADDRESS: 811 PALOMA DRIVE, SUITE A ROUND ROCK, TEXAS 78665, USA © 2010 Cerilliant Corporation. -

Stammesspezifische Unterschiede in Der Analgetischen Wirkung Von Buprenorphin Bei Der Maus
Stammesspezifische Unterschiede in der analgetischen Wirkung von Buprenorphin bei der Maus vorgelegt von Master of Science Juliane Rudeck geb. in Berlin von der Fakultät III – Prozesswissenschaften der Technischen Universität Berlin zur Erlangung des akademischen Grades Doktorin der Naturwissenschaften - Dr. rer. nat. - genehmigte Dissertation Promotionsausschuss: Vorsitzender: Prof. Dr. Roland Lauster Erster Gutachter: Prof. Dr. Jens Kurreck Zweiter Gutachter: Prof. Dr. Gilbert Schönfelder Dritter Gutachter: Prof. Dr. Lars Lewejohann Tag der wissenschaftlichen Aussprache: 08.10.2018 Berlin 2018 Eidesstattliche Erklärung „Ich erkläre an Eides Statt, dass die vorliegende Dissertation in allen Teilen von mir selbstständig angefertigt wurde und die benutzten Hilfsmittel vollständig angegeben worden sind.“ Berlin, den (Juliane Rudeck) I Aus dieser Arbeit hervorgegangene Publikationen Die Arbeit wurde am Bundesinstitut für Risikobewertung in der Abteilung Experimentelle Toxikologie und ZEBET angefertigt und gefördert vom BMBF (Grant No. 031A262D). Die Inhalte der hier vorliegenden Dissertation wurden teilweise bereits in wissenschaftlichen Journalen veröffentlicht bzw. Eingereicht zur Veröffentlichung. Diese sind im Folgenden aufgelistet. J. Rudeck, B. Bert, P. Marx-Stoelting, G. Schönfelder, S. Vogl, Liver lobe and strain differences in the activity of murine cytochrome P450 enzymes. Toxicology, (2018). Jul 1; 404-405:76-85. https://doi.org/10.1016/j.tox.2018.06.001. J. Rudeck, S. Vogl, C. Heinl, M. Steinfath, B. Bert, G. Schönfelder, Analgesic efficacy of buprenorphine depends on the mouse strain. Submitted for publication, (2018). J. Rudeck, B. Bert, S. Vogl, G. Schönfelder, L. Lewejohann, The effectiveness of habituation on experimental design: A retrospective analysis. In progress, (2018). II Zusammenfassung Die Verwendung einer optimalen Analgesie sollte oberste Priorität in der Versuchstierkunde haben und ist nicht nur aus ethischen, sondern auch aus rechtlichen Gründen verpflichtend. -

Influence of Different Elicitors on BIA Production in Macleaya Cordata
www.nature.com/scientificreports OPEN Infuence of diferent elicitors on BIA production in Macleaya cordata Peng Huang1,2,7, Liqiong Xia3,7, Li Zhou1,7, Wei Liu1,4, Peng Wang1, Zhixing Qing5* & Jianguo Zeng1,6* Sanguinarine (SAN) and chelerythrine (CHE) have been widely used as substitutes for antibiotics for decades. For a long time, SAN and CHE have been extracted from mainly Macleaya cordata, a plant species that is a traditional herb in China and belongs to the Papaveraceae family. However, with the sharp increase in demand for SAN and CHE, it is necessary to develop a new method to enhance the supply of raw materials. Here, we used methyl jasmonate (MJ), salicylic acid (SA) and wounding alone and in combination to stimulate aseptic seedlings of M. cordata at 0 h, 24 h, 72 h and 120 h and then compared the diferences in metabolic profles and gene expression. Ultimately, we found that the efect of using MJ alone was the best treatment, with the contents of SAN and CHE increasing by 10- and 14-fold, respectively. However, the increased SAN and CHE contents in response to combined wounding and MJ were less than those for induced by the treatment with MJ alone. Additionally, after MJ treatment, SAN and CHE biosynthetic pathway genes, such as those encoding the protopine 6-hydroxylase and dihydrobenzophenanthridine oxidase enzymes, were highly expressed, which is consistent with the accumulation of SAN and CHE. At the same time, we have also studied the changes in the content of synthetic intermediates of SAN and CHE after elicitor induction.