Ucin1258490710.Pdf (6.65
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Neuropeptide Galanin Modulates Behavioral and Neurochemical Signs of Opiate Withdrawal
The neuropeptide galanin modulates behavioral and neurochemical signs of opiate withdrawal Venetia Zachariou*†, Darlene H. Brunzell*, Jessica Hawes*, Diann R. Stedman*, Tamas Bartfai‡, Robert A. Steiner§, David Wynick¶,U¨ lo Langelʈ, and Marina R. Picciotto*,** *Department of Psychiatry, Yale University School of Medicine, New Haven, CT 06508; †Faculty of Medicine, Department of Pharmacology, University of Crete, 711 10 Crete, Greece; ‡Department of Neuropharmacology, The Scripps Research Institute, La Jolla, CA 92037; §Department of Physiology and Biophysics, University of Washington, Seattle, WA 98195; ¶Department of Medicine, Bristol University, Bristol BS2 8HW, United Kingdom; and ʈDepartment of Neurochemistry and Neurotoxicology, Stockholm University, 106 91 Stockholm, Sweden Edited by Richard D. Palmiter, University of Washington School of Medicine, Seattle, WA, and approved June 2, 2003 (received for review May 23, 2003) Much research has focused on pathways leading to opiate addic- galanin-mediated effects on morphine withdrawal were exam- tion. Pathways opposing addiction are more difficult to study but ined in transgenic mice that overexpress the peptide under the may be critical in developing interventions to combat drug depen- control of the dopamine--hydroxylase (DH) promoter, which dence and withdrawal. Galanin decreases firing of locus coeruleus normally drives gene expression in noradrenergic neurons (20), neurons, an effect hypothesized to decrease signs of opiate with- and in studies of c-fos and tyrosine hydroxylase (TH) phosphor- drawal. The current study addresses whether galanin affects mor- ylation in the LC of wild-type mice administered galnon. phine withdrawal signs by using a galanin agonist, galnon, that crosses the blood–brain barrier, and mice genetically engineered Methods to under- or overexpress galanin peptide. -

Download Product Insert (PDF)
PRODUCT INFORMATION Galnon (trifluoroacetate salt) Item No. 29925 O CAS Registry No.: 1217448-19-5 O Formal Name: 3-cyclohexyl-N-[(9H-fluoren-9- ylmethoxy)carbonyl]-L-alanyl-N-(4- methyl-2-oxo-2H-1-benzopyran-7-yl)- N O L-lysinamide, trifluoroacetate salt H H Synonym: Fmoc-β-Cha-Lys-AMC O MF: C H N O • CF COOH O N 40 46 4 6 3 N NH FW: 792.9 2 O H Purity: ≥98% Supplied as: A crystalline solid Storage: -20°C • CF COOH Stability: ≥2 years 3 Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Galnon (trifluoroacetate salt) is supplied as a crystalline solid. A stock solution may be made by dissolving the galnon (trifluoroacetate salt) in the solvent of choice, which should be purged with an inert gas. Galnon (trifluoroacetate salt) is soluble in organic solvents such as DMSO and dimethyl formamide. The solubility of galnon (trifluoroacetate salt) in these solvents is approximately 10 mg/ml. Galnon (trifluoroacetate salt) is sparingly soluble in aqueous buffers. For maximum solubility in aqueous buffers, galnon (trifluoroacetate salt) should first be dissolved in DMSO and then diluted with the aqueous buffer of choice. Galnon (trifluoroacetate salt) has a solubility of approximately 0.3 mg/ml in a 1:2 solution of DMSO:PBS (pH 7.2) using this method. We do not recommend storing the aqueous solution for more than one day. Description 1 Galnon is a galanin (GAL) receptor agonist (KD = 2.9 µM in Bowes cells expressing GAL1 receptors). -

“I Am Among Those Who Think That Science Has Great Beauty. A
“I am among those who think that science has great beauty. A scientist in his laboratory is not only a technician: he is also a child placed before natural phenomena which impress him like a fairy tale.” Marie Curie “The most exciting phrase to hear in science, the one that heralds new discoveries, is not Eureka! (I found it!) but rather, "hmm.... that's funny...."” Isaac Asimov “Science is a wonderful thing if one does not have to earn one's living at it.” Albert Einstein University of Alberta The effects of neurosteroids and neuropeptides on anxiety-related behavior by Elif Engin A thesis submitted to the Faculty of Graduate Studies and Research in partial fulfillment of the requirements for the degree of Doctor of Philosophy Department of Psychology ©Elif Engin Fall 2009 Edmonton, Alberta Permission is hereby granted to the University of Alberta Libraries to reproduce single copies of this thesis and to lend or sell such copies for private, scholarly or scientific research purposes only. Where the thesis is converted to, or otherwise made available in digital form, the University of Alberta will advise potential users of the thesis of these terms. The author reserves all other publication and other rights in association with the copyright in the thesis and, except as herein before provided, neither the thesis nor any substantial portion thereof may be printed or otherwise reproduced in any material form whatsoever without the author's prior written permission. Examining Committee Dallas Treit, Psychology Frederick Colbourne, Psychology Clayton Dickson, Psychology Peter Hurd, Psychology Kathryn Todd, Psychiatry Anantha Shekhar, Psychiatry, Indiana University For Nur and Marc You are the light in my mind, the warmth in my heart. -

Design, Synthesis and Characterization of Galanin Receptor Selective Ligands
!" #$"% "!&$$ ' () * ( +",-& . #/0!$ !$ 1 &2 . &2 "3 ( &. 4 . ( ( ( . &5 ( &6 ( ( 4 ( ( 4 & 0 & ( & 2 & " # (3 7#""8&9 (. : 4 4 & # 4 4 "& ( . : & ! # : & ; &7!/<8 4 & 9 ( ( & !" #$"% =00 && 0 > ? == = = "!/@@$ 9-/%@/"%,;/%#"$ 9-/%@/"%,;/%##% # $% # ("$,/" Design, Synthesis and Characterization of Galanin Receptor Selective Ligands Kristin Webling Abstract Galanin is a 29/30 amino acid long bioactive peptide discovered over 30 years ago when C-terminally amidated peptides were isolated from porcine intestines. The name galanin originates from a combination of the first and last amino acids - G from glycine and the rest from alanine. The first 15 amino acids are highly conserved throughout species, which indicates that the N-terminus is important for receptor recognition and binding. Galanin exerts its effects by binding to three different G protein-coupled receptors, which all differ according to regional distribution, -

Effects of Galnon, a Non-Peptide Galanin-Receptor Agonist, on Insulin
BBRC Biochemical and Biophysical Research Communications 328 (2005) 213–220 www.elsevier.com/locate/ybbrc Effects of galnon, a non-peptide galanin-receptor agonist, on insulin release from rat pancreatic islets Nguyen Thi Thu Quynha, Shahidul Md Islamb, Anders Flore´nc, Tamas Bartfaid, U¨ lo Langelc, Claes-Go¨ran O¨ stensona,* a Department of Molecular Medicine, Karolinska Institutet and Hospital, Stockholm, Sweden b Department of Medicine, Stockholm So¨der Hospital, Forskningscentrum, Sweden c Department of Neurochemistry and Neurotoxicology, Stockholm University, Stockholm, Sweden d Deparment of Neuropharmacology, The Scripps Research Institute, La Jolla, CA 92037, USA Received 18 December 2004 Available online 6 January 2005 Abstract Galanin is a neurotransmitter peptide that suppresses insulin secretion. The present study aimed at investigating how a non-pep- tide galanin receptor agonist, galnon, affects insulin secretion from isolated pancreatic islets of healthy Wistar and diabetic Goto– Kakizaki (GK) rats. Galnon stimulated insulin release potently in isolated Wistar rat islets; 100 lM of the compound increased the release 8.5 times (p < 0.001) at 3.3 mM and 3.7 times (p < 0.001) at 16.7 mM glucose. Also in islet perifusions, galnon augmented several-fold both acute and late phases of insulin response to glucose. Furthermore, galnon stimulated insulin release in GK rat islets. These effects were not inhibited by the presence of galanin or the galanin receptor antagonist M35. The stimulatory effects of galnon were partly inhibited by the PKA and PKC inhibitors, H-89 and calphostin C, respectively, at 16.7 but not 3.3 mM glu- cose. In both Wistar and GK rat islets, insulin release was stimulated by depolarization of 30 mM KCl, and 100 lM galnon further enhanced insulin release 1.5–2 times (p < 0.05). -
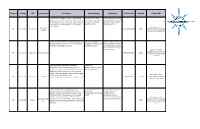
Category Catalog CAS Product Name Description Alias/Synonym Application M.F/Formula M.W/Mr
Category Catalog CAS Product Name Description Alias/Synonym Application M.F/Formula M.W/Mr. Product URL Pramlintide is an analogue of amylin, a small peptide AC 0137; AC 137; Symlin; Pramlintide (Symlin) has been hormone that is released into the bloodstream by the Tripro-Amylin; riproamylin; approved by the FDA as a new cells of the pancreas along with insulin, after a meal. Like Pramlintide; LS-181996; injectable drug for diabetes insulin, amylin is completely absent in individuals with LS181996; Amylin (both type 1 and 2). Type I diabetes. http://www.creative- Pramlintide APIs 10-101-28 151126-32-8 C171H267N51O53S2 3949.4 peptides.com/product/pramlin Acetate tide-item-10-101-28-89.html Sincalide corresponds to the C-terminal octapeptide of CCK-8; Cholecystokinin Sincalide ammonium salt is cholecystokinin (CCK) and acts on receptors within the Octapeptide; (Des-Pyr1,Des- used for the diagnosis of bile gallbladder wall causing it to contract. Gln2,Met5)-Caerulein tract and pancreatic diseases, and for the clinical radiology of the intestinal tract. http://www.creative- peptides.com/product/sincalid APIs 10-101-31 25126-32-3 Sincalide Acetate C49H62N10O16S3 1143.3 e-ammonium-salt-item-10-101- 31-98.html Creative peptides is specialized in the process Plenaxis;PPI- development and the manufacturing of bioactive 149;Abarelix;Abarelix-Depot- peptides. We offer custom peptide synthesis, process M;R-3827;R3827;R 3827 development, GMP manufacturing as well as catalog products. We supply Abarelix. More information please http://www.creative- visit the website: http://www.creative- APIs 10-101-60 183552-38-7 Abarelix C72H95ClN14O14 1416.06 peptides.com/product/abarelix- peptides.com/product/abarelix-item-10-101-60-2.html item-10-101-60-2.html Creative peptides is specialized in the process N-Acetyl-L-cysteine; NAC; L-α- Acute and chronic bronchitis, development and the manufacturing of bioactive Acetamido-β- laryngitis, tracheitis or peptides. -

Antibodies Products
Chapter 2 : Gentaur Products List • Anti Human mab TNFSF3 Source Mouse • Human VEGF165 Source E coli • Anti Human mab VEGFR 2 KDR 4 20I6 Biotin Source • Anti Human mab TNFSF4 Source Mouse • Mouse VEGF188 Source E coli Mouse • Anti Human mab TNFSF5 Source Mouse • Human VEGF189 Source E coli • Anti Human mab VEGFR 2 KDR 2F66 Source Mouse • Anti Human mab TNFSF6 Source Mouse • Anti Human mab VEGF165b Source Mouse • Anti Human mab VEGFR 2 KDR 2F46 Source Mouse • Anti Mouse mab TNFSF6 Source Rat • Anti Human mab VEGF A 3C5 Source Mouse • Anti Mouse mab VEGFR 2 Flk 1 3C8 Source Rat • Anti Human mab TNFSF8 Source Mouse • Anti Human mab VEGF A 2B86 Source Mouse • Anti Mouse mab VEGFR 2 Flk 1 3C8 Biotin Source Rat • Anti Mouse mab TNFSF8 Source Rat • Anti Human mab VEGF A 7G7 Source Mouse • Anti Mouse mab VEGFR 2 FLK 1 7A23 Source Rat • Anti Human mab TNFSF11A Source Mouse • Anti Human mab VEGF A 3 6D3 Source Mouse • Anti Mouse mab VEGFR 2 FLK 1 6C23 Source Rat • Anti Human mab TNFSF10 Source Mouse • Anti Mouse mab VEGF A 2G02 Source Rat • Anti Human mab VEGFR 2 KDR Agonistic Source Mouse • Anti Human mab TNFSF11 Source Mouse • Anti Human mab VEGF A 339 H2 Source Mouse • Anti Human pab VEGFR 2 KDR Agonistic Source Goat • Anti Human mab TNFSF12 Source Mouse • Anti Human pab VEGF A Source Rabbit • Anti Human mab VEGFR 2 KDR Agonistic Source Rat • Anti Human mab TNFSF13 Source Mouse • Anti Human pab VEGF A Source Goat • Anti Human mab VEGFR 2 KDR Antagonistic Source • Anti Human mab TNFSF13B Source Mouse • Anti Human pab VEGF Apan Peptide Source -

Supplementary Materials: AGTR1 Is Overexpressed in Neuroendocrine
Supplementary Materials: AGTR1 Is Overexpressed in Neuroendocrine Neoplasms, Regulates Secretion and May Potentially Serve as a Target for Molecular Imaging and Therapy Samantha Exner, Claudia Schuldt, Sachindra Sachindra, Jing Du, Isabelle Heing-Becker, Kai Licha, Bertram Wiedenmann and Carsten Grötzinger Table S1. Screening library compound list. -

Tocris製品30%Offキャンペーン価格表(2021/7/5~2021/8/31)
TOCRIS製品30%OFFキャンペーン価格表(2021/7/5~2021/8/31) (メーカーコード順) 希望納⼊価格 キャンペーン価格 コードNo.メーカーコード 英名 容量 (円) (円) 537-31171 0101/100 DL-2-Amino-4-phosphonobutyric Acid [DL-AP4] 100mg 24,000 16,800 - 0102/10 D(-)-2-Amino-4-phosphonobutyric Acid [D-AP4] 10mg 52,000 36,400 - 0102/50 D(-)-2-Amino-4-phosphonobutyric Acid [D-AP4] 50mg 222,000 155,400 - 0103/1 L(+)-2-Amino-4-phosphonobutyric Acid [L-AP4] 1mg 18,000 12,600 531-26804 0103/10 L(+)-2-Amino-4-phosphonobutyric Acid [L-AP4] 10mg 46,000 32,200 533-26803 0103/50 L(+)-2-Amino-4-phosphonobutyric Acid [L-AP4] 50mg 203,000 142,100 - 0104/10 DL-AP7 10mg 30,000 21,000 - 0104/50 DL-AP7 50mg 120,000 84,000 - 0105/10 DL-AP5 10mg 20,000 14,000 530-57943 0105/50 DL-AP5 50mg 81,000 56,700 - 0106/1 D-AP5 1mg 15,000 10,500 531-26843 0106/10 D-AP5 10mg 39,000 27,300 535-26846 0106/100 D-AP5 100mg 235,000 164,500 539-26844 0106/50 D-AP5 50mg 174,000 121,800 - 0107/10 L-AP5 10mg 54,000 37,800 - 0107/50 L-AP5 50mg 235,000 164,500 514-20993 0109/10 (-)-Bicuculline methobromide 10mg 28,000 19,600 518-20991 0109/50 (-)-Bicuculline methobromide 50mg 126,000 88,200 - 0111/1 Dihydrokainic acid 1mg 17,000 11,900 - 0111/10 Dihydrokainic acid 10mg 42,000 29,400 - 0111/50 Dihydrokainic acid 50mg 189,000 132,300 532-28291 0112/50 gamma-D-Glutamylglycine 50mg 38,000 26,600 539-26861 0114/50 N-Methyl-D-aspartic Acid [NMDA] 50mg 24,000 16,800 535-26863 0114/500 N-Methyl-D-aspartic Acid [NMDA] 500mg 100,000 70,000 533-31151 0125/100 DL-AP3 100mg 30,000 21,000 512-21011 0130/50 (+)-Bicuculline 50mg 47,000 32,900 535-57954 0131/10 (-)-Bicuculline -

Functional Μ-Opioid-Galanin Receptor Heteromers in the Ventral
1176 • The Journal of Neuroscience, February 1, 2017 • 37(5):1176–1186 Cellular/Molecular Functional -Opioid-Galanin Receptor Heteromers in the Ventral Tegmental Area Estefanía Moreno,1,2 Ce´sar Quiroz,3 William Rea,3 Ning-Sheng Cai,3 XJosefa Mallol,1,2 Antoni Corte´s,1,2 XCarme Lluís,1,2 X Enric I. Canela,1,2 Vicent Casado´,1,2* and XSergi Ferre´3* 1Center for Biomedical Research in Neurodegenerative Diseases Network and 2Department of Biochemistry and Molecular Biomedicine, Faculty of Biology, Institute of Biomedicine of the University of Barcelona, University of Barcelona, 08028 Barcelona, Spain, and 3Integrative Neurobiology Section, National Institute on Drug Abuse, Intramural Research Program, National Institutes of Health, Baltimore, Maryland 21224 The neuropeptide galanin has been shown to interact with the opioid system. More specifically, galanin counteracts the behavioral effects of the systemic administration of -opioid receptor (MOR) agonists. Yet the mechanism responsible for this galanin–opioid interaction has remained elusive. Using biophysical techniques in mammalian transfected cells, we found evidence for selective heteromerization of MOR and the galanin receptor subtype Gal1 (Gal1R). Also in transfected cells, a synthetic peptide selectively disrupted MOR–Gal1R heteromerization as well as specific interactions between MOR and Gal1R ligands: a negative cross talk, by which galanin counteracted MAPK activation induced by the endogenous MOR agonist endomorphin-1, and a cross-antagonism, by which a MOR antagonist coun- -

Galanin Mediates the Resilence Afforded by Exercise: Behavioral
GALANIN MEDIATES THE RESILENCE AFFORDED BY EXERCISE: BEHAVIORAL, NEUROCHEMICAL, AND NEUROANATOMICAL EVIDENCE by NATALE ROSE SCIOLINO (Under the Direction of Philip Holmes) ABSTRACT Exercise is effective treatment for symptoms of mental disorders such as anxiety and substance abuse. However, the neural mechanisms that support these benefits are only beginning to be identified and dissected. Our laboratory has repeatedly shown that exercise increases levels of the peptide galanin in the locus coeruleus (LC). The effects of galanin share many qualities with those of exercise. Both manipulations are protective against the behavioral impact of stress and cocaine in rodent models of mental disease. We hypothesized that the behavioral protection provided by exercise is mediated by galanin, and similarly that galanin receptor agonists would protect against stress- and drug-induced perturbation of behavior. We also predicted that exercise or administration of a galanin agonist would block neural markers of stress or cocaine in the frontal cortex, a region particularly vulnerable to these challenges. Male Sprague Dawley rats were used in all experiments, and a subset underwent stereotaxic brain cannulation for drug delivery (ICV) and/or in vivo microdialysis (intra-frontal cortex). Rats were assigned to sedentary or exercise conditions and then exposed to stress or cocaine as detailed in the experiments. We measured behavior in tests of anxiety, including the elevated plus maze, open field, and shock probe defensive burying test. We measured galanin levels after exercise using in situ hybridization and ELISA. We also performed in vivo microdialysis and Golgi- impregnation in the frontal cortex. The results showed that exercise increased galanin levels in the locus coeruleus. -

The Galanin Receptor Agonist, Galnon, Attenuates Cocaineinduced
bs_bs_banner PRECLINICAL STUDY doi:10.1111/adb.12166 The galanin receptor agonist, galnon, attenuates cocaine-induced reinstatement and dopamine overflow in the frontal cortex Yvonne E. Ogbonmwan1*, Natale R. Sciolino2*, Jessica L. Groves-Chapman2, Kimberly G. Freeman3, Jason P. Schroeder1, Gaylen L. Edwards3, Philip V. Holmes2,4 & David Weinshenker1 Department of Human Genetics, Emory University School of Medicine, Atlanta, GA, USA1, Neuroscience Program, Biomedical and Health Sciences Institute, University of Georgia, Athens, GA, USA2, Department of Physiology and Pharmacology, University of Georgia, Athens, GA, USA3 and Department of Psychology, University of Georgia, Athens, GA, USA4 ABSTRACT Relapse represents one of the most significant problems in the long-term treatment of drug addiction. Cocaine blocks plasma membrane monoamine transporters and increases dopamine (DA) overflow in the brain, and DA is critical for the motivational and primary reinforcing effects of the drug as well as cocaine-primed reinstatement of cocaine seeking in rats, a model of relapse. Thus, modulators of the DA system may be effective for the treatment of cocaine dependence. The endogenous neuropeptide galanin inhibits DA transmission, and both galanin and the synthetic galanin receptor agonist, galnon, interfere with some rewarding properties of cocaine. The purpose of this study was to further assess the effects of galnon on cocaine-induced behaviors and neurochemistry in rats. We found that galnon attenuated cocaine-induced motor activity, reinstatement and DA overflow in the frontal cortex at a dose that did not reduce baseline motor activity, stable self-administration of cocaine, baseline extracellular DA levels or cocaine-induced DA overflow in the nucleus accumbens (NAc).