MIST1, an Inductive Signal for Salivary Amylase in Mesenchymal Stem Cells
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Molecular Classification of Human Mesenchymal Stromal Cells Florian Rohart1, Elizabeth Mason1, Nicholas Matigian1, Rowland
bioRxiv preprint doi: https://doi.org/10.1101/024414; this version posted August 11, 2015. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Rohart'et'al,'The'MSC'Signature' 1' 1' A Molecular Classification of Human Mesenchymal Stromal Cells 2' Florian Rohart1, Elizabeth Mason1, Nicholas Matigian1, Rowland Mosbergen1, 3' Othmar Korn1, Tyrone Chen1, Suzanne Butcher1, Jatin Patel2, Kerry Atkinson2, 4' Kiarash Khosrotehrani2,3, Nicholas M Fisk2,4, Kim-Anh Lê Cao3 and Christine A 5' Wells1,5* 6' 1 Australian Institute for Bioengineering and Nanotechnology, The University of 7' Queensland, Brisbane, QLD Australia 4072 8' 2 The University of Queensland Centre for Clinical Research, Herston, Brisbane, 9' Queensland, Australia, 4029 10' 3 The University of Queensland Diamantina Institute, Translational Research 11' Institute, Woolloongabba, Brisbane QLD Australia, 4102 12' 4 Centre for Advanced Prenatal Care, Royal Brisbane & Women’s Hospital, Herston, 13' Brisbane, Queensland, Australia, 4029 14' 5 Institute for Infection, Immunity and Inflammation, College of Medical, Veterinary & 15' Life Sciences, The University of Glasgow, Scotland, UK G12 8TA 16' *Correspondence to: Christine Wells, [email protected] 17' bioRxiv preprint doi: https://doi.org/10.1101/024414; this version posted August 11, 2015. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. -

Identification of Pathways in Liver Repair Potentially Targeted By
International Journal of Molecular Sciences Article Identification of Pathways in Liver Repair Potentially Targeted by Secretory Proteins from Human Mesenchymal Stem Cells Sandra Winkler 1, Madlen Hempel 1, Sandra Brückner 1, Hans-Michael Tautenhahn 1, Roland Kaufmann 2 and Bruno Christ 1,* 1 Applied Molecular Hepatology Laboratory, Department of Visceral, Transplantation, Thoracic and Vascular Surgery, University Hospital of Leipzig, Liebigstraße 21, 04103 Leipzig, Germany; [email protected] (S.W.); [email protected] (M.H.); [email protected] (S.B.); [email protected] (H.-M.T.) 2 Department of General, Visceral and Vascular Surgery, Jena University Hospital, Erlanger Allee 101, 07747 Jena, Germany; [email protected] * Correspondence: [email protected]; Tel.: +49-160-903-19121; Fax: +49-341-971-13559 Academic Editor: Maurizio Muraca Received: 26 May 2016; Accepted: 29 June 2016; Published: 9 July 2016 Abstract: Background: The beneficial impact of mesenchymal stem cells (MSC) on both acute and chronic liver diseases has been confirmed, although the molecular mechanisms behind it remain elusive. We aim to identify factors secreted by undifferentiated and hepatocytic differentiated MSC in vitro in order to delineate liver repair pathways potentially targeted by MSC. Methods: Secreted factors were determined by protein arrays and related pathways identified by biomathematical analyses. Results: MSC from adipose tissue and bone marrow expressed a similar pattern of surface markers. After hepatocytic differentiation, CD54 (intercellular adhesion molecule 1, ICAM-1) increased and CD166 (activated leukocyte cell adhesion molecule, ALCAM) decreased. MSC secreted different factors before and after differentiation. -

Analysis of Mesenchymal Stem Cells (Mscs) Secretome from Mouse Models and Human Patients to Characterize Their Immunomodulatory Properties: a Proteomic Approach
UNIVERSITÀ DEGLI STUDI DI MILANO SCUOLA DI DOTTORATO Scienze Biochimiche DIPARTIMENTO DI MEDICINA VETERINARIA CORSO DI DOTTORATO DI RICERCA IN SCIENZE BIOCHIMICHE Ciclo XXX TESI DI DOTTORATO DI RICERCA Analysis of mesenchymal stem cells (MSCs) secretome from mouse models and human patients to characterize their immunomodulatory properties: a proteomic approach. Dott.ssa Fabiana SANTAGATA MATRICOLA: R10884 TUTOR: prof.ssa Gabriella TEDESCHI COORDINATORE DEL DOTTORATO: prof. Sandro SONNINO Anno Accademico 2016 - 2017 AIM OF THE WORK/SUMMARY ........................................................................................ 3 INTRODUCTION ................................................................................................................. 5 1.1 Stem cells ..................................................................................................................... 6 1.1.1 Definition and origin ................................................................................................. 6 1.1.1.1 Self-renewal .................................................................................................. 7 1.1.1.2 Potency ......................................................................................................... 7 1.1.2 Types of stem cells .................................................................................................. 8 1.1.2.1 Embryonic stem cells ........................................................................................ 8 1.1.2.2 Adult stem cells ................................................................................................ -

Gene-Expression and in Vitro Function of Mesenchymal Stromal Cells Are Affected in Juvenile Myelomonocytic Leukemia
Myeloproliferative Disorders SUPPLEMENTARY APPENDIX Gene-expression and in vitro function of mesenchymal stromal cells are affected in juvenile myelomonocytic leukemia Friso G.J. Calkoen, 1 Carly Vervat, 1 Else Eising, 2 Lisanne S. Vijfhuizen, 2 Peter-Bram A.C. ‘t Hoen, 2 Marry M. van den Heuvel-Eibrink, 3,4 R. Maarten Egeler, 1,5 Maarten J.D. van Tol, 1 and Lynne M. Ball 1 1Department of Pediatrics, Immunology, Hematology/Oncology and Hematopoietic Stem Cell Transplantation, Leiden University Med - ical Center, the Netherlands; 2Department of Human Genetics, Leiden University Medical Center, Leiden, the Netherlands; 3Dutch Childhood Oncology Group (DCOG), The Hague, the Netherlands; 4Princess Maxima Center for Pediatric Oncology, Utrecht, the Nether - lands; and 5Department of Hematology/Oncology and Hematopoietic Stem Cell Transplantation, Hospital for Sick Children, University of Toronto, ON, Canada ©2015 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol.2015.126938 Manuscript received on March 5, 2015. Manuscript accepted on August 17, 2015. Correspondence: [email protected] Supplementary data: Methods for online publication Patients Children referred to our center for HSCT were included in this study according to a protocol approved by the institutional review board (P08.001). Bone-marrow of 9 children with JMML was collected prior to treatment initiation. In addition, bone-marrow after HSCT was collected from 5 of these 9 children. The patients were classified following the criteria described by Loh et al.(1) Bone-marrow samples were sent to the JMML-reference center in Freiburg, Germany for genetic analysis. Bone-marrow samples of healthy pediatric hematopoietic stem cell donors (n=10) were used as control group (HC). -
The Knockout Mouse Project
COMMENTARY The Knockout Mouse Project Mouse knockout technology provides a powerful means of elucidating gene function in vivo, and a publicly available genome-wide collection of mouse knockouts would be significantly enabling for biomedical discovery. To date, published knockouts exist for only about 10% of mouse genes. Furthermore, many of these are limited in utility because they have not been made or phenotyped in standardized ways, and many are not freely available to researchers. It is time to harness new technologies and efficiencies of production to mount a high-throughput international effort to produce and phenotype knockouts for all mouse genes, and place these resources into the public domain. Now that the human and mouse genome expression pattern of the knocked-out gene in a dedicated project to produce knockout alleles http://www.nature.com/naturegenetics sequences are known1–3, attention has turned mouse tissues. Such marking of cells by a for all mouse genes and place them into the to elucidating gene function and identifying reporter gene facilitates the identification of public domain. The meeting took place from gene products that might have therapeutic new cell types according to their gene expres- 30 September to 1 October 2003 at the value. The laboratory mouse (Mus musculus) sion patterns and allows further characteriza- Banbury Conference Center at Cold Spring has had a prominent role in the study of tion of marked tissues and single cells. Harbor Laboratory. The attendees of the meet- human disease mechanisms throughout the Appreciation of the power of mouse genet- ing are the authors of this paper. -

The First Correct Three-Dimensional Structure of the DNA Molecule Was
Mutah University Dr. Jehad Al-Shuneigat Molecular Biology Faculty of Medicine Lecture 1 + 2 Second Semester: 2020/2021 Mu'tah University Faculty of Medicine Department of Biochemistry and Molecular Biology Course title: Molecular Biology Course code: 1503102 Credit hours: 2 credit hours Calendar description: 17 weeks / Second semester / 1st year Medicine Course description: This two-credit hours course is mandatory for first-year medical students. It consists of one lecture (1.5 hours) and a laboratory session a week. The course is designed to introduce students to the basics of molecular biology and genetics via starting with the chemical structures of the genetic material, cellular regulation of gene expression, mutations, and their relationship to health and disease. The laboratory is intended to facilitate students' understanding of theoretical concepts of both molecular biology and biochemistry. Objectives (intended learning outcomes): The overall objective is to enhance student understanding of advanced molecular biology and genetics-based medical topics to be covered in later courses. 1. Knowledge: A. Lectures Understand the involvement of molecular biology in medicine Understand the chemical structures of DNA and chromosomes Understand the mechanism and regulation of DNA replication Understand the mechanism and regulation of gene expression (transcription and translation) Understand the types and causes of DNA mutations Understand the mechanisms of DNA repair Understand the mechanism of inheritance Understand the mechanism -
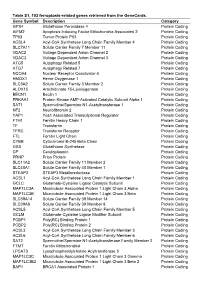
Table S1. 103 Ferroptosis-Related Genes Retrieved from the Genecards
Table S1. 103 ferroptosis-related genes retrieved from the GeneCards. Gene Symbol Description Category GPX4 Glutathione Peroxidase 4 Protein Coding AIFM2 Apoptosis Inducing Factor Mitochondria Associated 2 Protein Coding TP53 Tumor Protein P53 Protein Coding ACSL4 Acyl-CoA Synthetase Long Chain Family Member 4 Protein Coding SLC7A11 Solute Carrier Family 7 Member 11 Protein Coding VDAC2 Voltage Dependent Anion Channel 2 Protein Coding VDAC3 Voltage Dependent Anion Channel 3 Protein Coding ATG5 Autophagy Related 5 Protein Coding ATG7 Autophagy Related 7 Protein Coding NCOA4 Nuclear Receptor Coactivator 4 Protein Coding HMOX1 Heme Oxygenase 1 Protein Coding SLC3A2 Solute Carrier Family 3 Member 2 Protein Coding ALOX15 Arachidonate 15-Lipoxygenase Protein Coding BECN1 Beclin 1 Protein Coding PRKAA1 Protein Kinase AMP-Activated Catalytic Subunit Alpha 1 Protein Coding SAT1 Spermidine/Spermine N1-Acetyltransferase 1 Protein Coding NF2 Neurofibromin 2 Protein Coding YAP1 Yes1 Associated Transcriptional Regulator Protein Coding FTH1 Ferritin Heavy Chain 1 Protein Coding TF Transferrin Protein Coding TFRC Transferrin Receptor Protein Coding FTL Ferritin Light Chain Protein Coding CYBB Cytochrome B-245 Beta Chain Protein Coding GSS Glutathione Synthetase Protein Coding CP Ceruloplasmin Protein Coding PRNP Prion Protein Protein Coding SLC11A2 Solute Carrier Family 11 Member 2 Protein Coding SLC40A1 Solute Carrier Family 40 Member 1 Protein Coding STEAP3 STEAP3 Metalloreductase Protein Coding ACSL1 Acyl-CoA Synthetase Long Chain Family Member 1 Protein -

Molecular Diagnostic Methods for Early Detection of Breast Implant- Associated Anaplastic Large Cell Lymphoma in Plastic Surgery Procedures
WCRJ 2017; 4 (4): e982 MOLECULAR DIAGNOSTIC METHODS FOR EARLY DETECTION OF BREAST IMPLANT- ASSOCIATED ANAPLASTIC LARGE CELL LYMPHOMA IN PLASTIC SURGERY PROCEDURES A. SANTORELLI1, R. DI FRANCIA2, S. MARLINO1, A. DE MONACO3, A. GHANEM4, F. ROSSANO 5, S. DI MARTINO3 1Plastic Surgery, Health Park, Naples, Italy 2Italian Association of Pharmacogenomics and Molecular Diagnostics, Caserta, Italy 3CETAC Diagnostic and Research Center, Caserta, Italy 4Reconstructive and Aesthetic Surgery at Blizard Institute, Queen Mary University of London, London, United Kingdom 5Plastic Surgery, Clinica Grimaldi, S. Giorgio a Cremano, Naples, Italy Abstract – Background: Genotyping is crucial to the identification of genetic markers under- lying development of neoplastic T cell diseases and individual molecular monitoring of minimal residual disease. However, these methods need to fulfill the principles of analytical validation to determine their suitability to assess single point mutation in target genes. Methods: This review outlines current knowledge of the genetics of various forms of ALCL and new genetic markers in ALK-negative ALCL frequently recurred in Breast Implant-Associated Ana- plastic Large Cell Lymphoma (BIA-ALCL). For the appropriate choice of any method, several criteria must be considered: i) known genetic variants in a given cancer gene; ii) diffusion and availability of large platforms and required equipment; iii) suitability of tests for routine diagnostics; iv) capacity of methods to offer a specific and sensitive detection of mutant alleles within great excess of wild- type alleles in a given sample; v) cost-effectiveness. Conclusions: This review is intended to provide the reader with a better understanding of the various technologies available in the routine clinical laboratory for early detection of genetic mark- ers of cancer T cell. -
Systemic Mesenchymal Stem Cell Treatment Mitigates Structural and Functional Retinal Ganglion Cell Degeneration in a Mouse Model of Multiple Sclerosis
Article Systemic Mesenchymal Stem Cell Treatment Mitigates Structural and Functional Retinal Ganglion Cell Degeneration in a Mouse Model of Multiple Sclerosis Oliver W. Gramlich1,2,AlexanderJ.Brown3,4, Cheyanne R. Godwin1,2, Michael S. Chimenti5, Lauren K. Boland6, James A. Ankrum6, and Randy H. Kardon1,2 1 Department of Ophthalmology and Visual Sciences, The University of Iowa, Iowa City, IA, USA 2 Center for the Prevention and Treatment of Visual Loss, Iowa City VA Health Care System, Iowa City, IA, USA 3 Department of Biomedical Research, National Jewish Health, Denver, CO, USA 4 Department of Immunology & Microbiology, University of Colorado Anschutz Medical Campus, Aurora, CO, USA 5 Iowa Institute of Human Genetics, Carver College of Medicine, The University of Iowa, Iowa City, IA, USA 6 Roy J. Carver Department of Biomedical Engineering College, The University of Iowa, Iowa City, IA, USA Correspondence: Oliver W. Purpose: The purpose of this study was to determine mesenchymal stem cell (MSC) Gramlich, Department of therapy efficacy on rescuing the visual system in the experimental autoimmune Ophthalmology and Visual Sciences, encephalomyelitis (EAE) model of multiple sclerosis (MS) and to provide new mecha- The University of Iowa, 200 Hawkins nistic insights. Dr, Iowa City, IA 52242, USA. e-mail: Methods: [email protected] EAE was induced in female C57BL6 mice by immunization with myelin oligo- dendrocyte glycoprotein (MOG)35–55, complete Freund’s adjuvant, and pertussis toxin. Received: March 23, 2020 The findings were compared to sham-immunized mice. Half of the EAE mice received Accepted: May 26, 2020 intraperitoneally delivered stem cells (EAE + MSC). -

P16ink4a Gene Promoter Variation and Differential Binding of a Repressor, the Ras-Responsive Zinc-finger Transcription Factor, RREB
Oncogene (2003) 22, 2285–2295 & 2003 Nature Publishing Group All rights reserved 0950-9232/03 $25.00 www.nature.com/onc p16INK4a gene promoter variation and differential binding of a repressor, the ras-responsive zinc-finger transcription factor, RREB Shuling Zhang1, Xiaolan Qian2, Chanelle Redman1, Valeri Bliskovski1, Edward S Ramsay1, Douglas R Lowy2 and Beverly AMock* ,1 1Laboratory of Genetics, Center for Cancer Research, NCI, NIH, 37 Convent Drive, MSC 4255, Bldg. 37, Rm 2B-08, Bethesda, MD 20892-4255, USA; 2Laboratory of Cellular Oncology, Center for Cancer Research, NCI, NIH, 37 Convent Drive, MSC 4263, Bldg. 37, Rm 4106, Bethesda, MD 20892-4263, USA BALB/c mice are susceptible to the development of familial melanoma (Hussussian et al., 1994), and the pristane-induced plasma cell tumors, and have a rare gene is frequently inactivated in a wide variety of allelic variant in the coding region of the p16INK4a (p16) cancers by methylation or mutation (Baylin and Bestor, tumor suppressor gene that produces a protein with 2002; Jones and Baylin, 2002). Selective targeting of p16 impaired activity. We have now found that the BALB/c in mice place them at an increased risk for tumor p16 promoter has an allelic variant that may also development (Krimpenfort et al., 2001; Sharpless et al., compromise p16 activity. Following pristane treatment, 2001). Much less is known about the possible regulatory BALB/c p16 mRNA levels in B cells were lower than that defects. in DBA/2 or C.D2-Pctr1, a resistant BALB/c congenic Our recent work in knockout mice and transient strain that harbors DBA/2 chromatin surrounding the p16 transfections of p16 cDNAallelic variants has impli- locus. -
Alternative Splicing Regulates Mouse Embryonic Stem Cell Pluripotency and Differentiation
Alternative splicing regulates mouse embryonic stem cell pluripotency and differentiation Nathan Salomonisa,b,1, Christopher R. Schlievea, Laura Pereirac, Christine Wahlquistd, Alexandre Colasd, Alexander C. Zambone, Karen Vranizanf,2, Matthew J. Spindlera,b, Alexander R. Picoa, Melissa S. Clineg, Tyson A. Clarkg, Alan Williamsg, John E. Blumeg, Eva Samala, Mark Mercolad, Bradley J. Merrillc, and Bruce R. Conklina,b,h,1 aGladstone Institute of Cardiovascular Disease, San Francisco, CA 94158; bPharmaceutical Sciences and Pharmacogenomics Graduate Program, University of California, San Francisco, CA 94143; cDepartment of Biochemistry and Molecular Genetics, University of Illinois, Chicago, IL 60607; dSanford-Burnham Institute for Medical Research, La Jolla, CA 92037; eDepartment of Pharmacology, University of California, La Jolla, CA 92093; fFunctional Genomics Laboratory, University of California, Berkeley, CA 94720; gAffymetrix, Inc., Santa Clara, CA 95051; and hDepartments of Medicine and Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94143 Edited by Elaine Fuchs, The Rockefeller University, New York, NY, and approved April 27, 2010 (received for review October 27, 2009) Two major goals of regenerative medicine are to reproducibly APS appear to increase transcript diversity in ES cells and thus transform adult somatic cells into a pluripotent state and to con- are likely to affect differentiation to distinct tissue lineages (10– trol their differentiation into specific cell fates. Progress toward 13). A better understanding of how AS regulates protein di- these goals would be greatly helped by obtaining a complete pic- versity and translational repression during ES cell differentiation ture of the RNA isoforms produced by these cells due to alterna- may provide critical insights into this process. -

Open Full Page
Priority Reports Spontaneous Human Adult Stem Cell Transformation Daniel Rubio,1 Javier Garcia-Castro,1,2 Marı´a C. Martı´n,3 Ricardo de la Fuente,1 Juan C. Cigudosa,3 Alison C. Lloyd,4 and Antonio Bernad1 1Department of Immunology and Oncology, Centro Nacional de Biotecnologı´a/Consejo Superior de Investigaciones Cientificas, UAM Campus de Cantoblanco; 2Oncology Department, Hospital Universitario del Nin˜o Jesu´s; 3Cytogenetics Unit, Centro Nacional de Investigaciones Oncolo´gicas, Madrid, Spain; and 4Laboratory for Molecular Cell Biology, University College London, London, United Kingdom Abstract bypass this stage, they continue to grow until telomeres become critically short and cells enter crisis phase, characterized by Human adult stem cells are being evaluated widely for various generalized chromosome instability that provokes mass apoptosis therapeutic approaches. Several recent clinical trials have (5). Human cells immortalize at low frequency and seem resistant reported their safety, showing them to be highly resistant to to spontaneous transformation. Here we report that MSC in long- transformation. The clear similarities between stem cell and term cultures immortalize at high frequency and undergo cancer stem cell genetic programs are nonetheless the basis of a 2010 spontaneous transformation. recent proposal that some cancer stem cells could derive from human adult stem cells. Here we show that although they can be managed safely during the standard ex vivo expansion period Materials and Methods (6-8 weeks), human mesenchymal stem cells can undergo Isolation of adipose tissue–derived mesenchymal stem cell. Samples spontaneous transformation following long-term in vitro of discarded adipose15, tissue from eight pediatric and two adult non- culture (4-5 months).