Heroes' Compensation: an All-Points Bulletin Calling for Coverage Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

UNIVERSITY of CALIFORNIA, IRVINE Unraveling Host and Parasite Pathways in Human Innate Immunity to Toxoplasma Gondii DISSERTATIO
UNIVERSITY OF CALIFORNIA, IRVINE Unraveling host and parasite pathways in human innate immunity to Toxoplasma gondii DISSERTATION submitted in partial satisfaction of the requirements for the degree of DOCTOR OF PHILOSOPHY in Biological Sciences by Lanny Gov Dissertation Committee: Assistant Professor Melissa B. Lodoen, Chair Professor Andrea J. Tenner Professor Craig M. Walsh 2014 Chapter 2 © 2013 American Society for Microbiology All other materials © 2014 Lanny Gov DEDICATION To My mother: my hero and my champion; Jonathan Farnworth: my better half; My loving and supportive family: brothers George and James, and sister-in-law Kelly; My dearest friends: Eugenia Hu, Quen Vong, Tracy Tang, and Erika Villaruel Thank you for so many years of love, laughter, and encouragement, and for helping me believe I could accomplish anything. “Promise me you’ll always remember: You’re braver than you believe, and stronger than you seem, and smarter than you think.” –A.A. Milne, Winnie-the-Pooh “You don’t have to know everything, but you should try to.” -Nori Ueno, on preparation for my Advancement exam ii TABLE OF CONTENTS Page LIST OF FIGURES iv LIST OF TABLES v ACKNOWLEDGMENTS vi CURRICULUM VITAE ix ABSTRACT OF THE DISSERTATION xii CHAPTER ONE: Introduction to Toxoplasma gondii Immunity 1 Toxoplasma gondii Biology 2 T. gondii Clinical Disease 6 T. gondii Invasion of Host Cells 9 Three Modes of T. gondii Intracellular Entry 12 Immunity to T. gondii 13 Toll-like Receptor Sensing of T. gondii 15 Nod-like Receptor Sensing of T. gondii 17 Modulation of Host Cell Pathways by T. gondii Effectors 19 Monocytes in Immunity to T. -

Homeland Emergency Response Operational and Equipment Systems
Disclaimer: This report was prepared by the International Association of Fire Fighters (IAFF) under contract with NIOSH. It should not be considered a statement of NIOSH policy or of any agency or individual who was involved. PROJECT HEROES Homeland Emergency Response Operational and Equipment Systems Task 1: A Review of Modern Fire Service Hazards and Protection Needs Presented to: National Personal Protective Technology Laboratory National Institute for Occupational Safety and Health (NIOSH) Post Office Box 18070 626 Cochrans Mill Road Pittsburgh, Pennsylvania 15236 Presented by: Occupational Health and Safety Division International Association of Fire Fighters (IAFF) 1750 New York Avenue, N.W. Washington, DC 20006 13 October 2003 EXECUTIVE SUMMARY The first task of Project HEROES was undertaken by the International Association of Fire Fighters (IAFF) to examine and define the protection needs of fire fighters and other first responders during a broad array of different missions. This task began with a review for how the fire service and its responsibilities have changed over the past 20 years since personal protective equipment (PPE) was then affected by Project FIRES. In that 20 year period, the fire service has evolved to gain responsibility for a larger number of missions. Fire suppression is no longer the chief responsibility for most fire departments, but rather responses to a wide range of missions, including emergency medical aid, technical rescue, and more recently the prospect for terrorism events involving weapons of mass destruction. As America’s fire fighters attempt to keep up with these changing roles, it is noted that the level of preparedness and PPE needed to safety carry out the different missions is often lacking. -
Riparian Adaptive Management Symposium: a Conversation Between Scientists and Management Forks, Washington
United States Department of Agriculture Riparian Adaptive Forest Service Pacific Northwest Management Symposium: Research Station General Technical Report A Conversation between PNW-GTR-830 December 2010 Scientists and Management The Forest Service of the U.S. Department of Agriculture is dedicated to the principle of multiple use management of the Nation’s forest resources for sustained yields of wood, water, forage, wildlife, and recreation. Through forestry research, cooperation with the States and private forest owners, and management of the national forests and national grasslands, it strives—as directed by Congress—to provide increasingly greater service to a growing Nation. The U.S. Department of Agriculture (USDA) prohibits discrimination in all its programs and activities on the basis of race, color, national origin, age, disability, and where applicable, sex, marital status, familial status, parental status, religion, sexual orientation, genetic information, political beliefs, reprisal, or because all or part of an individual’s income is derived from any public assistance program. (Not all prohibited bases apply to all programs.) Persons with disabilities who require alternative means for communication of program information (Braille, large print, audiotape, etc.) should contact USDA’s TARGET Center at (202) 720-2600 (voice and TDD). To file a complaint of discrimination, write USDA, Director, Office of Civil Rights, Room 1400 Independence Avenue, SW, Washington, DC 20250-9410 or call (800) 795-3272 (voice) or (202) 720-6382 (TDD). USDA is an equal opportunity provider and employer. Technical Editors Douglas F. Ryan is an ecologist and decision support specialist, U.S. Department of Agriculture, Forest Service, Pacific Northwest Research Station, Focused Science Delivery Program, 3625 93rd Ave. -
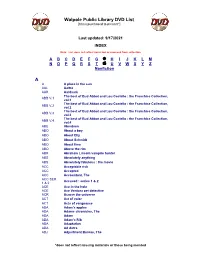
Walpole Public Library DVD List A
Walpole Public Library DVD List [Items purchased to present*] Last updated: 9/17/2021 INDEX Note: List does not reflect items lost or removed from collection A B C D E F G H I J K L M N O P Q R S T U V W X Y Z Nonfiction A A A place in the sun AAL Aaltra AAR Aardvark The best of Bud Abbot and Lou Costello : the Franchise Collection, ABB V.1 vol.1 The best of Bud Abbot and Lou Costello : the Franchise Collection, ABB V.2 vol.2 The best of Bud Abbot and Lou Costello : the Franchise Collection, ABB V.3 vol.3 The best of Bud Abbot and Lou Costello : the Franchise Collection, ABB V.4 vol.4 ABE Aberdeen ABO About a boy ABO About Elly ABO About Schmidt ABO About time ABO Above the rim ABR Abraham Lincoln vampire hunter ABS Absolutely anything ABS Absolutely fabulous : the movie ACC Acceptable risk ACC Accepted ACC Accountant, The ACC SER. Accused : series 1 & 2 1 & 2 ACE Ace in the hole ACE Ace Ventura pet detective ACR Across the universe ACT Act of valor ACT Acts of vengeance ADA Adam's apples ADA Adams chronicles, The ADA Adam ADA Adam’s Rib ADA Adaptation ADA Ad Astra ADJ Adjustment Bureau, The *does not reflect missing materials or those being mended Walpole Public Library DVD List [Items purchased to present*] ADM Admission ADO Adopt a highway ADR Adrift ADU Adult world ADV Adventure of Sherlock Holmes’ smarter brother, The ADV The adventures of Baron Munchausen ADV Adverse AEO Aeon Flux AFF SEAS.1 Affair, The : season 1 AFF SEAS.2 Affair, The : season 2 AFF SEAS.3 Affair, The : season 3 AFF SEAS.4 Affair, The : season 4 AFF SEAS.5 Affair, -

Volume 8, Number 1
POPULAR CULTURE STUDIES JOURNAL VOLUME 8 NUMBER 1 2020 Editor Lead Copy Editor CARRIELYNN D. REINHARD AMY DREES Dominican University Northwest State Community College Managing Editor Associate Copy Editor JULIA LARGENT AMANDA KONKLE McPherson College Georgia Southern University Associate Editor Associate Copy Editor GARRET L. CASTLEBERRY PETER CULLEN BRYAN Mid-America Christian University The Pennsylvania State University Associate Editor Reviews Editor MALYNNDA JOHNSON CHRISTOPHER J. OLSON Indiana State University University of Wisconsin-Milwaukee Associate Editor Assistant Reviews Editor KATHLEEN TURNER LEDGERWOOD SARAH PAWLAK STANLEY Lincoln University Marquette University Associate Editor Graphics Editor RUTH ANN JONES ETHAN CHITTY Michigan State University Purdue University Please visit the PCSJ at: mpcaaca.org/the-popular-culture-studies-journal. Popular Culture Studies Journal is the official journal of the Midwest Popular Culture Association and American Culture Association (MPCA/ACA), ISSN 2691-8617. Copyright © 2020 MPCA. All rights reserved. MPCA/ACA, 421 W. Huron St Unit 1304, Chicago, IL 60654 EDITORIAL BOARD CORTNEY BARKO KATIE WILSON PAUL BOOTH West Virginia University University of Louisville DePaul University AMANDA PICHE CARYN NEUMANN ALLISON R. LEVIN Ryerson University Miami University Webster University ZACHARY MATUSHESKI BRADY SIMENSON CARLOS MORRISON Ohio State University Northern Illinois University Alabama State University KATHLEEN KOLLMAN RAYMOND SCHUCK ROBIN HERSHKOWITZ Bowling Green State Bowling Green State -

Hero As Citizen Models of Heroic Thought and Action in Homer, Plato and Rousseau
Man as Hero - Hero as Citizen Models of Heroic Thought and Action in Homer, Plato and Rousseau Dominic Stefanson Thesis submitted for the degree of Doctor of Philosophy in the Discipline of Politics School of History and Politics The University of Adelaide December 2004 Frontisp iece Illustration included in print copy of thesis: Jacques-Louis David, The Death of Socrates (1787) iii Contents Abstract………………………………………………………………………… v Declaration…………………………………………………………………….. vi Acknowledgements……………………………………………………………. vii Introduction…………………………………………………………………… 1 PART I HOMER: THE BIRTH OF HEROISM 1. Homeric Man: The Hero …………………………………………………… 21 • Homeric heroes as models for men 22 • Seeking immortal glory achieving a “god-like status” 26 • Who is the hero? Preconditions for heroism 35 • A guide to heroism: transparency of thought, speech and action 44 • The transparency of Homeric narration 48 • Conclusion 55 2. Homeric Polis: the absence of a polis……………………………………… 57 • Finley and Adkins 58 • Seeking a polis in the Iliad 66 • The heroic code as an anti-model 77 • Patroclus’ funeral games as a microcosm of the polis 87 • Conclusion 93 PART II PLATO: EXTENDING HEROISM TO THE POLITICAL 3. Platonic Man: The philosopher as a new hero…………………………… 95 • Socrates: an heroic life 97 • Socratic Intellectualism: the primacy of knowledge 101 • Androgynous virtue 106 • Seeking eternity: philosophy as an activity for gods 111 • Tripartite psychology: heroism within human reach 117 • Theory of Forms 119 • The late dialogues 125 • Conclusion 130 iv 4. Platonic Polis: The political engagement of the heroic philosopher…….. 133 • Enlisting Philosophers to rule 135 • The elitist nature of philosophical rule throughout the Platonic corpus 137 • Philosophical leadership in the late dialogues 143 • The benefits of philosophical rule: harmony and unity in the Republic 150 • Does the community benefit from philosophical leadership? 154 • Conclusion 162 PART III ROUSSEAU: THE DEMISE OF HEROISM IN POLITICAL THOUGHT 5. -

Outstanding Original Screenplay Screenplay by Bong Joon Ho and Han Jin Won Story by Bong Joon Ho
FOR YOUR CONSIDERATION OUTSTANDING ORIGINAL SCREENPLAY SCREENPLAY BY BONG JOON HO AND HAN JIN WON STORY BY BONG JOON HO PARASITE Screenplay by Bong Joon Ho and Han Jin Won Story by Bong Joon Ho 1 TITLE SEQUENCE OVER BLACK 1 Accompanied by dark but curiously upbeat MUSIC. At the end of the credits, the MAIN TITLE, in strange calligraphy, fills the screen -- “PARASITE” MUSIC FADES. 2 INT. SEMI-BASEMENT - DAY 2 A dank semi-basement apartment. KI-WOO, 24, runs from corner to corner searching desperately for a Wi-Fi signal. Various networks pop up, but they’re all password-protected. KI-WOO NO. Not you too “iptime.” Ki-Jung! Upstairs neighbor finally locked up his Wi-Fi. ADJACENT ROOM -- Lying on the floor of the narrow room, KI-JUNG, 23, barely moves her lips -- ‘Fuck.’ KI-JUNG Try ‘123456789.’ Then try it backwards. KI-WOO No luck. ANOTHER ROOM -- Also lying on the floor, CHUNG-SOOK, 49, the mother, scoffs at their collective misery. CHUNG-SOOK What am I supposed to do if someone calls me? What if it’s a job? Hey, Ki-Tek! She kicks KI-TEK, 49, who is sleeping at her feet. CHUNG-SOOK (CONT’D) I know you’re awake, asshole. Care to comment? KI-TEK (wiping his drool) What? 2. CHUNG-SOOK Our phones have been suspended for weeks, and now the neighbors have shut us out. What’s your plan? She kicks him again. CHUNG-SOOK (CONT’D) What are you going to do about it? What’s the plan, genius? She treats Ki-Tek like shit, but it doesn’t bother him. -

Hartford Public Library DVD Title List
Hartford Public Library DVD Title List # 20 Wild Westerns: Marshals & Gunman 2 Days in the Valley (2 Discs) 2 Family Movies: Family Time: Adventures 24 Season 1 (7 Discs) of Gallant Bess & The Pied Piper of 24 Season 2 (7 Discs) Hamelin 24 Season 3 (7 Discs) 3:10 to Yuma 24 Season 4 (7 Discs) 30 Minutes or Less 24 Season 5 (7 Discs) 300 24 Season 6 (7 Discs) 3-Way 24 Season 7 (6 Discs) 4 Cult Horror Movies (2 Discs) 24 Season 8 (6 Discs) 4 Film Favorites: The Matrix Collection- 24: Redemption 2 Discs (4 Discs) 27 Dresses 4 Movies With Soul 40 Year Old Virgin, The 400 Years of the Telescope 50 Icons of Comedy 5 Action Movies 150 Cartoon Classics (4 Discs) 5 Great Movies Rated G 1917 5th Wave, The 1961 U.S. Figure Skating Championships 6 Family Movies (2 Discs) 8 Family Movies (2 Discs) A 8 Mile A.I. Artificial Intelligence (2 Discs) 10 Bible Stories for the Whole Family A.R.C.H.I.E. 10 Minute Solution: Pilates Abandon 10 Movie Adventure Pack (2 Discs) Abduction 10,000 BC About Schmidt 102 Minutes That Changed America Abraham Lincoln Vampire Hunter 10th Kingdom, The (3 Discs) Absolute Power 11:14 Accountant, The 12 Angry Men Act of Valor 12 Years a Slave Action Films (2 Discs) 13 Ghosts of Scooby-Doo, The: The Action Pack Volume 6 complete series (2 Discs) Addams Family, The 13 Hours Adventure of Sherlock Holmes’ Smarter 13 Towns of Huron County, The: A 150 Year Brother, The Heritage Adventures in Babysitting 16 Blocks Adventures in Zambezia 17th Annual Lane Automotive Car Show Adventures of Dally & Spanky 2005 Adventures of Elmo in Grouchland, The 20 Movie Star Films Adventures of Huck Finn, The Hartford Public Library DVD Title List Adventures of Ichabod and Mr. -

Petition to Protect the Monarch Butterfly (Danaus Plexippus Plexippus) Under the Endangered Species Act
BEFORE THE SECRETARY OF THE INTERIOR © Jeffrey E. Belth PETITION TO PROTECT THE MONARCH BUTTERFLY (DANAUS PLEXIPPUS PLEXIPPUS) UNDER THE ENDANGERED SPECIES ACT Notice of Petition Sally Jewell, Secretary U.S. Department of the Interior 1849 C Street NW Washington, D.C. 20240 [email protected] Dan Ashe, Director U.S. Fish and Wildlife Service 1849 C Street NW Washington, D.C. 20240 [email protected] Douglas Krofta, Chief Branch of Listing, Endangered Species Program U.S. Fish and Wildlife Service 4401 North Fairfax Drive, Room 420 Arlington, VA 22203 [email protected] Monarch ESA Petition 2 PETITIONERS The Center for Biological Diversity (“Center”) is a nonprofit, public interest environmental organization dedicated to the protection of imperiled species and the habitat and climate they need to survive through science, policy, law, and creative media. The Center is supported by more than 775,000 members and activists throughout the country. The Center works to secure a future for all species, great or small, hovering on the brink of extinction. The Center for Food Safety (“CFS”) is a nonprofit public interest organization established in 1997 whose mission centers on protecting public health and the environment by curbing the adverse impacts of industrial agriculture and food production systems on public health, the environment, and animal welfare, and by instead promoting sustainable forms of agriculture. As particularly relevant here, CFS is the leading nonprofit working on the adverse impacts of genetically engineered crops and neonicotinoid pesticides. CFS and its over half-a-million members are concerned about the impacts of industrial agriculture on biodiversity generally, and on monarch butterflies specifically. -
Heroes and Philosophy
ftoc.indd viii 6/23/09 10:11:32 AM HEROES AND PHILOSOPHY ffirs.indd i 6/23/09 10:11:11 AM The Blackwell Philosophy and Pop Culture Series Series Editor: William Irwin South Park and Philosophy Edited by Robert Arp Metallica and Philosophy Edited by William Irwin Family Guy and Philosophy Edited by J. Jeremy Wisnewski The Daily Show and Philosophy Edited by Jason Holt Lost and Philosophy Edited by Sharon Kaye 24 and Philosophy Edited by Richard Davis, Jennifer Hart Week, and Ronald Weed Battlestar Galactica and Philosophy Edited by Jason T. Eberl The Offi ce and Philosophy Edited by J. Jeremy Wisnewski Batman and Philosophy Edited by Mark D. White and Robert Arp House and Philosophy Edited by Henry Jacoby Watchmen and Philosophy Edited by Mark D. White X-Men and Philosophy Edited by Rebecca Housel and J. Jeremy Wisnewski Terminator and Philosophy Edited by Richard Brown and Kevin Decker ffirs.indd ii 6/23/09 10:11:12 AM HEROES AND PHILOSOPHY BUY THE BOOK, SAVE THE WORLD Edited by David Kyle Johnson John Wiley & Sons, Inc. ffirs.indd iii 6/23/09 10:11:12 AM This book is printed on acid-free paper. Copyright © 2009 by John Wiley & Sons, Inc. All rights reserved Published by John Wiley & Sons, Inc., Hoboken, New Jersey Published simultaneously in Canada No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, scanning, or otherwise, except as permitted under Section 107 or 108 of the 1976 United States Copyright Act, without either the prior written permission of the Publisher, or autho- rization through payment of the appropriate per-copy fee to the Copyright Clearance Center, 222 Rosewood Drive, Danvers, MA 01923, (978) 750–8400, fax (978) 646–8600, or on the web at www.copyright.com. -

The Multiplatform Brand Flows of Heroes
Selling Across the Spectrum: The Multiplatform Brand Flows of Heroes ERIN GIANNINI, independent scholar ABSTRACT This article examines how the NBC show Heroes and its use of product placement across multiple platforms represented an early response by networks and advertisers to concerns over ad-skipping and alternate viewing platforms by attempting to reconfigure how brand flow operates across multiple platforms. Not only did the series employ ‘second shift aesthetics’ (Caldwell 2003, 135), which represents networks bringing viewer-users back to the programme by ‘further engag[ing] and activat[ing] the text’ (Caldwell 2004, 50), but the products integrated within the text are pulled into the available world of Heroes’ alternative platform’s textual world, particularly Nissan branded cars. As Henry Jenkins writes: ‘Old media are not being displaced. Rather, their framework and structure shifted by the introduction of new technology’ (2006, 3-4). How these products are used within Heroes storylines and its interaction with characters and platform goes beyond simple placement to make the product another character within the show. Further, I examine the way in which Heroes, as a transmedia text, provided many points of entry for viewer-users to interact with it. While an analysis of fan activity is not the focus of this article, it is important to note these possibilities because of the ways in which the promotional apparatus of the network utilized these types of convergences for the series. Yet, in the case of Heroes, this was achieved by suturing new technological abilities of brand extension with an older model of ad- supported television (namely, the single-sponsorship model of early American television), both within the terrestrial television series and across multiple platforms. -

A God Why Is Hermes Hungry?1
CHAPTER FOUR A GOD WHY IS HERMES HUNGRY?1 Ἀλλὰ ξύνοικον, πρὸς θεῶν, δέξασθέ με. (But by the gods, accept me as house-mate) Ar. Plut 1147 1. Hungry Hermes and Greedy Interpreters In the evening of the first day of his life baby Hermes felt hungry, or, more precisely, as the Homeric Hymn to Hermes in which the god’s earliest exploits are recorded, says, “he was hankering after flesh” (κρειῶν ἐρατίζων, 64). This expression reveals only the first of a long series of riddles that will haunt the interpreter on his slippery journey through the hymn. After all, craving for flesh carries overtly negative connotations.2 In the Homeric idiom, for instance, the expression is exclusively used as a predicate of unpleasant lions.3 Nor does it 1 This chapter had been completed and was in the course of preparation for the press when I first set eyes on the important and innovative study of theHymn to Hermes by D. Jaillard, Configurations d’Hermès. Une “théogonie hermaïque”(Kernos Suppl. 17, Liège 2007). Despite many points of agreement, both the objectives and the results of my study widely diverge from those of Jaillard. The basic difference between our views on the sacrificial scene in the Hymn (which regards only a section of my present chapter on Hermes) is that in the view of Jaillard Hermes is a god “who sac- rifices as a god” (“un dieu qui sacrifie en tant que dieu,” p. 161; “Le dieu n’est donc, à aucun moment de l’Hymne, réellement assimilable à un sacrificateur humain,” p.