Common Pediatric Fractures
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Greenstick Fracture Soft Cast No FU
Orthopaedic Department York Teaching Hospital This is a follow-up letter to your recent telephone consultation with the fracture care team explaining the ongoing management of your injury. Your case has been reviewed by an Orthopaedic Consultant (Bone Specialist) and Fracture Care Physiotherapist. You have sustained a greenstick fracture to your distal radius and/or ulna (forearm just before the wrist). This is a specific type of fracture that occurs in children’s bones Healing: This normally takes approximately 4 - 6 weeks to heal. It is normal for it to continue to ache a bit for a few weeks after this. Pain and swelling: Take pain killers as needed. The plaster backslab helps healing by keeping the bones in a good position. Elevate the arm to reduce swelling for the first few days Using your arm: You may use the arm as pain allows. It is important to keep the elbow moving to prevent stiffness. Follow up: There is a small chance that this fracture can displace (move). Therefore we routinely recommend a repeat x ray at 1 week after the injury and a new plaster cast. Arrangements for this appointment should have been made during your telephone consultation. Should you need to reschedule this appointment please see contact details at the top of this letter. Area of injury: If you are worried that you are unable to follow this rehabilitation plan, Or, if you are experiencing pain or symptoms, other than at the site of the original injury or surrounding area, or have any questions, then please phone the Fracture Care Team for advice. -

Part Fracture Dislocation Due to Stress Concentration at Intramedullary Nail End 1Devendra Chouhan, 2Vishal Kumar, 3Manish Kundanmal Kothari, 4Mandeep S Dhillon
JPMER Devendra Chouhan et al 10.5005/jp-journals-10028-1142 CASE REPORT Dissociation of Shaft of Humerus from Head in Three- part Fracture Dislocation due to Stress Concentration at Intramedullary Nail End 1Devendra Chouhan, 2Vishal Kumar, 3Manish Kundanmal Kothari, 4Mandeep S Dhillon ABSTRACT authors best knowledge. We report the first such case A three-part fracture dislocation of the proximal humerus of three-part fracture dislocation involving the greater usually dissociates from the shaft at the level of the surgical tuberosity and proximal shaft of humerus with a 25 years neck or the anatomical neck. Dissociation from the shaft below old Rush nail in situ. this level has not reported in the literature before. Here we describe the injury of a middle aged patient with a three-part CASE REPORT fracture dislocation of the humerus with dissociation of the head from the shaft at the level of proximal shaft humerus with A 60-year-old male presented in the emergency depart- a 25 years old Rush nail in situ. The dislocated head was found ment with acute pain in right shoulder following road abutting the thoracic wall. This case report highlights the effect traffic accident 8 hours ago. He was travelling on a bike of stress concentration at intramedullary nail ends in the upper limb as well as the need for an extended approach when the when a car hit him from the side. He was violently thrown dislocated head appears close to the thoracic wall. off his motorcycle followed by fall on an outstretched hand. He had no other complaints. -
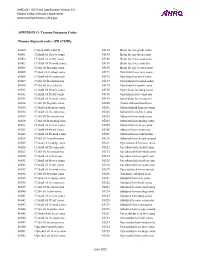
PSI Appendix G Version 6.0 Patient Safety Indicators Appendices
AHRQ QI™ ICD-9-CM Specification Version 6.0 Patient Safety Indicators Appendices www.qualityindicators.ahrq.gov APPENDIX G: Trauma Diagnosis Codes Trauma diagnosis codes: (TRAUMID) 80000 Closed skull vault fx 85184 Brain lac nec-proln coma 80001 Cl skull vlt fx w/o coma 85185 Brain lac nec-deep coma 80002 Cl skull vlt fx-brf coma 85186 Brain lacer nec-coma nos 80003 Cl skull vlt fx-mod coma 85189 Brain lacer nec-concuss 80004 Cl skl vlt fx-proln coma 85190 Brain lac nec w open wnd 80005 Cl skul vlt fx-deep coma 85191 Opn brain lacer w/o coma 80006 Cl skull vlt fx-coma nos 85192 Opn brain lac-brief coma 80009 Cl skl vlt fx-concus nos 85193 Opn brain lacer-mod coma 80010 Cl skl vlt fx/cerebr lac 85194 Opn brain lac-proln coma 80011 Cl skull vlt fx w/o coma 85195 Open brain lac-deep coma 80012 Cl skull vlt fx-brf coma 85196 Opn brain lacer-coma nos 80013 Cl skull vlt fx-mod coma 85199 Open brain lacer-concuss 80014 Cl skl vlt fx-proln coma 85200 Traum subarachnoid hem 80015 Cl skul vlt fx-deep coma 85201 Subarachnoid hem-no coma 80016 Cl skull vlt fx-coma nos 85202 Subarach hem-brief coma 80019 Cl skl vlt fx-concus nos 85203 Subarach hem-mod coma 80020 Cl skl vlt fx/mening hem 85204 Subarach hem-prolng coma 80021 Cl skull vlt fx w/o coma 85205 Subarach hem-deep coma 80022 Cl skull vlt fx-brf coma 85206 Subarach hem-coma nos 80023 Cl skull vlt fx-mod coma 85209 Subarach hem-concussion 80024 Cl skl vlt fx-proln coma 85210 Subarach hem w opn wound 80025 Cl skul vlt fx-deep coma 85211 Opn subarach hem-no coma 80026 Cl skull vlt fx-coma nos 85212 -

Management of Pediatric Forearm Torus Fractures: a Systematic
ORIGINAL ARTICLE Management of Pediatric Forearm Torus Fractures A Systematic Review and Meta-Analysis Nan Jiang, MD,*† Zhen-hua Cao, MD,*‡ Yun-fei Ma, MD,*† Zhen Lin, MD,§ and Bin Yu, MD*† many disadvantages, such as heavy, bulky, and requires a second Objectives: Pediatric forearm torus fracture, a frequent reason for emer- visit to the hospital for removal. These flaws of cast may bring gency department visits, can be immobilized by both rigid cast and non- inconvenience to children as well as their families. In recent years, rigid methods. However, controversy still exists regarding the optimal many pediatric clinicians reported other methods to instead tradi- treatment of the disease. The aim of this study was to compare, in a system- tionally used cast, including soft cast,9,10 Futuro wrist splint,8,11 atic review, clinical efficacy of rigid cast with nonrigid methods for immo- and double Tubigrip.11 Although patients that suffered from fore- bilization of the pediatric forearm torus fractures. arm torus fractures can be immobilized by both rigid cast and non- Methods: Literature search was performed of PubMed and Cochrane Li- rigid materials, controversy still exists in the optimal treatment of brary by 2 independent reviewers to identify randomized controlled trials this fracture. comparing rigid cast with nonrigid methods for pediatric forearm torus The aim of this study was to, in a systematic review and fractures from inception to December 31, 2013, without limitation of publi- meta-analysis, compare clinical efficacy of recently used nonrigid cation language. Trial quality was assessed using the modified Jadad scale. immobilization methods with rigid cast. -

Vanderbilt Sports Medicine
Alabama AAP Fall Meeting Sept.19-20, 2009 Pediatric Fracture Care for the Pediatrician Andrew Gregory, MD, FAAP, FACSM Assistant Professor Orthopedics & Pediatrics Program Director, Sports Medicine Fellowship Vanderbilt University Vanderbilt Sports Medicine Disclosure No conflict of interest - unfortunately for me, I have no financial relationships with companies making products regarding this topic to disclose Objectives Review briefly the differences of pediatric bone Review Pediatric Fracture Classification Discuss subtle fractures in kids Discuss a few other pediatric only conditions 1 Pediatric Skeleton Bone is relatively elastic and rubbery Periosteum is quite thick & active Ligaments are strong relative to the bone Presence of the physis - “weak link” Ligament injuries & dislocations are rare – “kids don’t sprain stuff” Fractures heal quickly and have the capacity to remodel Anatomy of Pediatric Bone Epiphysis Physis Metaphysis Diaphysis Apophysis Pediatric Fracture Classification Plastic Deformation – Bowing usually of fibula or ulna Buckle/ Torus – compression, stable Greenstick – unicortical tension Complete – Spiral, Oblique, Transverse Physeal – Salter-Harris Apophyseal avulsion 2 Plastic deformation Bowing without fracture Often deformed requiring reduction Buckle (Torus) Fracture Buckled Periosteum – Metaphyseal/ diaphyseal junction Greenstick Fracture Cortex Broken on Only One Side – Incomplete 3 Complete Fractures Transverse – Perpendicular to the bone Oblique – Across the bone at 45-60 o – Unstable Spiral – Rotational -

Pediatric Orthopedic Injuries… … from an ED State of Mind
Traumatic Orthopedics Peds RC Exam Review February 28, 2019 Dr. Naminder Sandhu, FRCPC Pediatric Emergency Medicine Objectives to cover today • Normal bone growth and function • Common radiographic abnormalities in MSK diseases • Part 1: Atraumatic – Congenital abnormalities – Joint and limb pain – Joint deformities – MSK infections – Bone tumors – Common gait disorders • Part 2: Traumatic – Common pediatric fractures and soft tissue injuries by site Overview of traumatic MSK pain Acute injuries • Fractures • Joint dislocations – Most common in ED: patella, digits, shoulder, elbow • Muscle strains – Eg. groin/adductors • Ligament sprains – Eg. Ankle, ACL/MCL, acromioclavicular joint separation Chronic/ overuse injuries • Stress fractures • Tendonitis • Bursitis • Fasciitis • Apophysitis Overuse injuries in the athlete WHY do they happen?? Extrinsic factors: • Errors in training • Inappropriate footwear Overuse injuries Intrinsic: • Poor conditioning – increased injuries early in season • Muscle imbalances – Weak muscle near strong (vastus medialus vs lateralus patellofemoral pain) – Excessive tightness: IT band, gastroc/soleus Sever disease • Anatomic misalignments – eg. pes planus, genu valgum or varum • Growth – strength and flexibility imbalances • Nutrition – eg. female athlete triad Misalignment – an intrinsic factor Apophysitis • *Apophysis = natural protruberance from a bone (2ndary ossification centres, often where tendons attach) • Examples – Sever disease (Calcaneal) – Osgood Schlatter disease (Tibial tubercle) – Sinding-Larsen-Johansson -

Metacarpal Fractures
METACARPAL FRACTURES BY LORYN P. WEINSTEIN, MD, AND DOUGLAS P. HANEL, MD The majority of metacarpal fractures are closed injuries amenable to conservative treatment with external immobilization and subsequent rehabilitation. Internal fixation is favored for unstable fracture patterns and patients who require early motion. Percutaneous pinning usually is successful for metacarpal neck fractures and comminuted head fractures. Shaft and base fractures can be treated with pinning or open reduction and internal fixation; the latter, being more rigid, allows early rehabilitation. External fixation has a limited yet defined role for metacarpal fractures with complex soft-tissue injury and/or segmental bone loss. The recent development of bioabsorbable implants holds promise for skeletal rigidity with minimal soft-tissue morbidity, but long-term in vivo data support- ing the use of these implants is not currently available. Copyright © 2002 by the American Society for Surgery of the Hand arly treatment of metacarpal fractures was lim- Surgical techniques rapidly expanded to include ret- ited to the only tools available: manipulation rograde fracture pinning, intramedullary pinning, and Eand casting. The discovery of percutaneous transfixion pinning. Many of the K-wires in use today fracture fixation near the turn of the century opened have the same diamond-shaped tip and sizing speci- up a new world of possibilities. It was 25 years after fications as the original design. Bennett’s original manuscript that Lambotte de- The first plate and screw set for the hand was scribed the first surgical stabilization of a basilar introduced in the late 1930s. By today’s standards, the thumb fracture by using a thin carpenter’s nail.1 By Hermann Metacarpal Bone Set was quite lean; it 1913, Lambotte had authored a fracture text with included 3 longitudinal plates of 2, 3, and 4 holes, a multiple examples of pinning, wiring, and plating of drill, screwdriver, and 9 screws.1 Improvements in hand fractures. -

Proximal Humerus Fracture After Keyhole Biceps Tenodesis
A Case Report & Literature Review Proximal Humerus Fracture After Keyhole Biceps Tenodesis Stefanie N. Reiff, BA, Shane J. Nho, MD, MS, and Anthony A. Romeo, MD is the only one published in English. The patient pro- Abstract vided written informed consent for print and electronic A biceps tenodesis is a common surgical procedure that publication of this case report. is often carried out in conjunction with other surgical shoulder repairs to relieve biceps tendonitis. This case CASE REPORT presents a 50-year-old woman who suffered a humerus The patient, a 50-year-old woman, underwent left shoul- fracture following an open keyhole biceps tenodesis. The potential reasons for the fracture as well as a brief der revision arthroscopic subacromial decompression analysis of the technique itself are presented. To our and open biceps tenodesis. Past medical history was sig- knowledge, this is the first case report of a humerus frac- nificant for insulin-dependent diabetes mellitus (onset age, ture following keyhole biceps tenodesis in the English- 15 years) and hypothyroidism. Past surgical history was language literature. notable for left shoulder os acromiale with arthroscopic subacromial decompression performed 7 months before iceps tendonitis, a relatively common condition the revision surgery pertinent to this case. Tenodesis of the that affects the shoulder, causes pain over its biceps tendon was indicated on the basis of past surgical anterior aspect, near the bicipital groove and history, clinical examination in the office, and intraopera- -

Ankle Injuries
Pediatric Fractures of the Ankle Nicholas Frane DO Zucker/Hofstra School of Medicine Northwell Health Core Curriculum V5 Disclosure • Radiographic Images Courtesy of: Dr. Jon-Paul Dimauro M.D or Christopher D Souder, MD, unless otherwise specified Core Curriculum V5 Outline • Epidemiology • Anatomy • Classification • Assessment • Treatment • Outcomes Core Curriculum V5 Epidemiology • Distal tibial & fibular physeal injuries 25%-38% of all physeal fractures • Ankle is the 2nd most common site of physeal Injury in children • Most common mechanism of injury Sports • 58% of physeal ankle fractures occur during sports activities • M>F • Commonly seen in 8-15y/o Hynes D, O'Brien T. Growth disturbance lines after injury of the distal tibial physis. Their significance in prognosis. J Bone Joint Surg Br. 1988;70:231–233 Zaricznyj B, Shattuck LJ, Mast TA, et al. Sports-related injuries in school-aged children. Am J Sports Med. 1980;8:318–324. Core Curriculum V5 Epidemiology Parikh SN, Mehlman CT. The Community Orthopaedic Surgeon Taking Trauma Call: Pediatric Ankle Fracture Pearls and Pitfalls. J Orthop Trauma. 2017;31 Suppl 6:S27-S31. doi:10.1097/BOT.0000000000001014 Spiegel P, et al. Epiphyseal fractures of the distal ends of the tibia and fibula. J Bone Joint Surg Am. 1978;60(8):1046-50. Core Curriculum V5 Anatomy • Ligamentous structures attach distal to the physis • Growth plate injury more likely than ligament failure secondary to tensile weakness in physis • Syndesmosis • Anterior Tibio-fibular ligament (AITFL) • Posterior Inferior Tibio-fibular -

Org Tibia (Shinbone) Shaft Fractures
.org Tibia (Shinbone) Shaf Fractures Page ( 1 ) The tibia, or shinbone, is the most common fractured long bone in your body. The long bones include the femur, humerus, tibia, and fi bula. A tibial shaf fracture occurs along the length of the bone, below the knee and above the ankle. Because it typically takes a major force to break a long bone, other injuries of en occur with these types of fractures. Anatomy The lower leg is made up of two bones: the tibia and fi bula. The tibia is the larger of the two bones. It supports most of your weight and is an important part of both the knee joint and ankle joint. The tibia is the larger bone in your lower leg. Tibial shaf fractures occur Types of Tibial Shaf Fractures along the length of the bone. The tibia can break in several ways. The severity of the fracture usually depends on the amount of force that caused the break. The fi bula is of en broken as well. Common types of tibial fractures include: Stable fracture: This type of fracture is barely out of place. The broken ends of the bones basically line up correctly and are aligned. In a stable fracture, the bones usually stay in place during healing. Displaced fracture: When a bone breaks and is displaced, the broken ends are separated and do not line up. These types of fractures of en require surgery to put the pieces back together. Transverse fracture: This type of fracture has a horizontal fracture line. This fracture can be unstable, especially if the fi bula is also broken. -

Common Fractures and Dislocations of the Hand
CME Common Fractures and Dislocations of the Hand Neil F. Jones, M.D. Learning Objectives: After reading this article, the participant should be able Jesse B. Jupiter, M.D. to: 1. Describe the concept of early protected movement with Kirschner-wired Donald H. Lalonde, M.D. finger fractures to the hand therapist. 2. Choose the most appropriate method Orange, Calif.; Boston, Mass.; and of fracture fixation to achieve the goal of a full range of motion. 3. Describe the Saint John, New Brunswick, Canada methods of treatment available for the most common fractures and dislocations of the hand. Background: The main goal of treatment of hand and finger fractures and dislocations is to attain a full range of wrist and nonscissoring finger motion after the treatment is accomplished. This CME article consists of literature review, illustrations, movies, and an online CME examination to bring the participant recent available information on the topic. Methods: The authors reviewed literature regarding the most current treat- ment strategies for common hand and finger fractures and dislocations. Films were created to illustrate operative and rehabilitation methods used to treat these problems. A series of multiple-choice questions, answers, discussions, and references were written and are provided online so that the participant can receive the full benefit of this review. Results: Many treatment options are available, from buddy and Coban taping to closed reduction with immobilization; percutaneous pins or screws; and open reduction with pins, screws, or plates. Knowledge of all available options is important because all can be used to achieve the goal of treatment in the shortest time possible. -

Torus (Buckle) Fracture Discharge Advice
Torus (Buckle) Fracture Discharge Advice Information for you Follow us on Twitter @NHSaaa Find us on Facebook at www.facebook.com/nhsaaa Visit our website: www.nhsaaa.net All our publications are available in other formats What has happened? Your child has sustained a torus fracture, also known as a “buckle” fracture, of the radius and/or ulna (the long bones at the wrist). The bone “buckles” on one side rather than actually breaks and is commonly seen in children as their bones are soft and flexible. Will my child need a cast? Torus fractures heal well without any long-term complications. They do not require any operations or to be placed in a cast. However, using a wrist splint provides comfort and reduces the risk of further injury. It should be worn at all times but can be removed for washing and showering without any risk to the fracture. Simple painkillers such as paracetamol and/or ibuprofen can also be used to reduce discomfort. How long should my child wear the splint for? In general, the older the child is, the longer they will need to wear the splint. We recommend that children under five years old should wear the splint for one week, those age five to ten years should wear it for two weeks and those over ten years should wear it for three weeks. If your child removes the splint before this time but is comfortable and moving their wrist freely then there is no need to insist that they wear the splint for longer. However, if your child is still sore and reluctant to use their wrist when the splint is removed, then you 2 may reapply the splint.