Exploratory Spatial Data Analysis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Edim Otop Gully Erosion Site in Calabar Municipality, Cross River State
FEDERAL REPUBLIC OF NIGERIA Public Disclosure Authorized THE NIGERIA EROSION AND WATERSHED MANAGEMENT PROJECT (NEWMAP) Public Disclosure Authorized FINAL REPORT OF THE ENVIRONMENTAL AND SOCIAL MANAGEMENT PLAN (ESMP) FOR EDIM OTOP GULLY EROSION SITE IN CALABAR Public Disclosure Authorized MUNICIPALITY, CROSS RIVER STATE Public Disclosure Authorized State Project Management Unit (SPMU) Cross River State, Calabar TABLE OF CONTENTS Cover Page i Table of Contents ii List of Tables vii List of Figures viii List of Plates ix Executive Summary xi CHAPTER ONE – INTRODUCTION 1 1.1 Background 1 1.2 Description of the Proposed Intervention 3 1.3 Rationale for the Study 5 1.4 Scope of Work 5 CHAPTER TWO - INSTITUTIONAL AND LEGAL FRAMEWORK 7 2.1 Background 7 2.2 World Bank Safeguard Policies 8 2.2.1 Environmental Assessment (EA) OP 4.01 9 2.2.2 Natural Habitats (OP 4.04) 9 2.2.3 Pest Management (OP 4.09) 10 2.2.4 Forest (OP 4.36) 10 2.2.5 Physical Cultural Resources (OP 4.11) 11 2.2.6 Involuntary Resettlement (OP 4.12) 11 2.2.7 Safety of Dams OP 4.37 12 2.2.8 Projects on International Waterways OP 7.50 12 2.3 National Policy, Legal, Regulatory and Administrative Frameworks 13 2.3.1 The Federal Ministry of Environment (FMENV) 13 2.3.2 The National Policy on the Environment (NPE) of 1989 14 2.3.3 Environmental Impact Assessment Act No. 86, 1992 (FMEnv) 14 2.3.4 The National Guidelines and Standards for Environmental Pollution Control in Nigeria 14 2.3.5 The National Effluents Limitations Regulation 15 ii 2.3.6 The NEP (Pollution Abatement in Industries and Facilities Generating Waste) Regulations 15 2.3.7 The Management of Solid and Hazardous Wastes Regulations 15 2.3.8 National Guidelines on Environmental Management Systems (1999) 15 2.3.9 National Guidelines for Environmental Audit 15 2.3.10 National Policy on Flood and Erosion Control 2006 (FMEnv) 16 2.3.11 National Air Quality Standard Decree No. -

Nigeria's Constitution of 1999
PDF generated: 26 Aug 2021, 16:42 constituteproject.org Nigeria's Constitution of 1999 This complete constitution has been generated from excerpts of texts from the repository of the Comparative Constitutions Project, and distributed on constituteproject.org. constituteproject.org PDF generated: 26 Aug 2021, 16:42 Table of contents Preamble . 5 Chapter I: General Provisions . 5 Part I: Federal Republic of Nigeria . 5 Part II: Powers of the Federal Republic of Nigeria . 6 Chapter II: Fundamental Objectives and Directive Principles of State Policy . 13 Chapter III: Citizenship . 17 Chapter IV: Fundamental Rights . 20 Chapter V: The Legislature . 28 Part I: National Assembly . 28 A. Composition and Staff of National Assembly . 28 B. Procedure for Summoning and Dissolution of National Assembly . 29 C. Qualifications for Membership of National Assembly and Right of Attendance . 32 D. Elections to National Assembly . 35 E. Powers and Control over Public Funds . 36 Part II: House of Assembly of a State . 40 A. Composition and Staff of House of Assembly . 40 B. Procedure for Summoning and Dissolution of House of Assembly . 41 C. Qualification for Membership of House of Assembly and Right of Attendance . 43 D. Elections to a House of Assembly . 45 E. Powers and Control over Public Funds . 47 Chapter VI: The Executive . 50 Part I: Federal Executive . 50 A. The President of the Federation . 50 B. Establishment of Certain Federal Executive Bodies . 58 C. Public Revenue . 61 D. The Public Service of the Federation . 63 Part II: State Executive . 65 A. Governor of a State . 65 B. Establishment of Certain State Executive Bodies . -

Cross River STATE-WIDE RAPID HEALTH FACILITY ASSESSMENT
Report of the Cross River STATE-WIDE RAPID HEALTH FACILITY ASSESSMENT In Preparation for Elimination of Mother-to-Child Transmission of HIV March 2013 Report of the Cross River STATE-WIDE RAPID HEALTH FACILITY ASSESSMENT In Preparation for Elimination of Mother-to-Child Transmission of HIV May 2013 This publication may be freely reviewed, quoted, reproduced, or translated, in full or in part, provided the source is acknowledged. The mention of specific organizations does not imply endorsement and does not suggest that they are recommended by the Cross River State Ministry of Health over others of a similar nature not mentioned. Copyright © 2013 Cross River State Ministry of Health, Nigeria Citation: Cross River State Ministry of Health and FHI 360. 2013. Cross River State-wide Rapid Health Facility Assessment, Nigeria: Cross River State Ministry of Health and FHI 360. The Cross River State-wide Rapid Health Facility Assessment was supported in part by the U.S. Agency for International Development (USAID). FHI 360 provided assistance to the Cross River State Government to conduct this assessment. Financial assistance was provided by USAID under the terms of the Cooperative Agreement AID-620-A-00002, of the Strengthening Integrated Delivery of HIV/ AIDS Services Project. This report does not necessarily reflect the views of FHI 360, USAID or the United States Government. Table of Contents Foreword ...................................................................................................................................................................................................... -

Nigeria - Accessibility to Emonc Facilities in the State of Cross River
Nigeria - Accessibility to EmONC facilities in the State of Cross River Last Update: March 2016 Nigeria - Accessibility to EmONC facilities for the Cross River State Table of Contents Acknowledgements ..................................................................................................................... 4 1. Introduction ............................................................................................................................. 5 2. Measured indicators and assumptions .................................................................................... 5 3. Tool used for the different analyses: AccessMod 5.0 ............................................................. 7 4. Data and national norms used in the different analyses .......................................................... 8 4.1 Statistical Data ............................................................................................................... 9 4.1.1 LGA Number of pregnant women for 2010 and 2015 ........................................... 9 4.2 Geospatial Data ........................................................................................................... 12 4.2.1 Administrative boundaries and extent of the study area ...................................... 13 4.2.2 Geographic location of the EmONC facilities and associated information ......... 17 4.2.4 Transportation network ........................................................................................ 26 4.2.5 Hydrographic network ........................................................................................ -

NIGERIA: Registration of Cameroonian Refugees September 2019
NIGERIA: Registration of Cameroonian Refugees September 2019 TARABA KOGI BENUE TAKUM 1,626 KURMI NIGERIA 570 USSA 201 3,180 6,598 SARDAUNA KWANDE BEKWARA YALA DONGA-MANTUNG MENCHUM OBUDU OBANLIKU ENUGU 2,867 OGOJA AKWAYA 17,301 EBONYI BOKI IKOM 1,178 MAJORITY OF THE ANAMBRA REFUGEES ORIGINATED OBUBRA FROM AKWAYA 44,247 ABI Refugee Settlements TOTAL REGISTERED YAKURR 1,295ETUNG MANYU REFUGEES FROM IMO CAMEROON CROSS RIVER ABIA BIOMETRICALLY BIASE VERIFIED 35,636 3,533 AKAMKPA CAMEROON Refugee Settlements ODUKPANI 48 Registration Site CALABAR 1,058MUNICIPAL UNHCR Field Office AKWA IBOM CALABAR NDIAN SOUTH BAKASSI667 UNHCR Sub Office 131 58 AKPABUYO RIVERS Affected Locations 230 Scale 1:2,500,000 010 20 40 60 80 The boundaries and names shown and the designations used on this map do not imply official Kilometers endorsement or acceptance by the United Nations. Data Source: UNHCR Creation Date: 2nd October 2019 DISCLAIMER: The boundaries and names shown, and the designations used on this map do not imply official endorsement or acceptance by the United Nations. A technical team has been conducting a thorough review of the information gathered so as to filter out any data discrepancies. BIOMETRICALLY VERIFIED REFUGEES REGISTRATION TREND PER MONTH 80.5% (35,636 individuals) of the total refugees 6272 counteded at household level has been 5023 registered/verified through biometric capture of iris, 4025 3397 fingerprints and photo. Refugee information were 2909 2683 2371 also validated through amendment of their existing 80.5% information, litigation and support of national 1627 1420 1513 1583 586 VERIFIED documentations. Provision of Refugee ID cards will 107 ensure that credible information will effectively and efficiently provide protection to refugees. -

Calabar Municipal Recreation Centre Expression Of
CALABAR MUNICIPAL RECREATION CENTRE EXPRESSION OF INDIGENOUS CONTEXT IN RECREATIONAL FACILITY DESIGN BY EkpaAyahambemNtan DEPARTMENT OF ARCHITECTURE, AHMADU BELLO UNIVERSITY, ZARIA NIGERIA MAY 2014 1 CALABAR MUNICIPAL RECREATION CENTRE EXPRESSION OF INDIGENOUS CONTEXT IN RECREATIONAL FACILITY DESIGN BY EkpaAyahambemNtan B.sc Arch (ABU 2007) M.sc/ENV-DESIGN/01787/2006–2007 A DISSERTATION SUBMITTED TO THE SCHOOL OF POSTGRADUATE STUDIES, AHMADU BELLO UNIVERSITY, ZARIA NIGERIA IN PARTIAL FULFILLMENT OF THE REQUIREMENT FOR THE AWARD OF MASTER OF SCIENCE DEGREE IN ARCHITECTURE DEPARTMENT OF ARCHITECTURE, AHMADU BELLO UNIVERSITY, ZARIA NIGERIA MAY 2014. 2 DECLARATION I declare that the work in the dissertation entitled „CALABAR MUNICIPAL RECREATION CENTRE EXPRESSION OF INDIGENOUS CONTEXT, IN RECREATIONAL FACILITY DESIGN‟ has been performed by me in the Department of Architecture under the supervision of Dr. S. N Oluigbo and Dr. A. Ango The information derived from the literature has duly been acknowledged in the text and a list of references provided. No part of this dissertation was previously presented for another degree or diploma at any university. EkpaAyahambemNtan May, 2014 Name of student Signature Date 3 CERTIFICATION This dissertation entitled “CALABAR MUNICIPAL RECREATION CENTRE EXPRESSION OF INDIGENOUS CONTEXT, IN RECREATIONAL FACILITY DESIGN” by Ekpa .A. Ntan, meets the regulations governing the award of the degree of Master of Science of Ahmadu Bello University, Zaria, and is approved for its contribution to knowledge and literary presentation. _____________________________ ________________ Dr S. N. Oluigbo Date Chairman, Supervisory Committee _____________________________ ________________ Dr. A. Ango Date Member, Supervisory Committee __________________________ __________________ Dr. M.L. Sagada Date Member, Supervisory Committee _____________________________ ________________ Arc. -

Conflict Incident Monthly Tracker
Conflict Incident Monthly Tracker Cross River State: February - M a rch 20 1 8 B a ck gro und Municipal. Others: In February, Cameroonian Criminality was a driver of Violence Affecting gendarmes reportedly killed three fishermen This monthly tracker is designed to update Women and Girls (VAWG) in the state during and injured two others in a border Peace Agents on patterns and trends in the period. In January, for instance, a female community in Ikom LGA. The incident conflict risk and violence, as identified by the medical doctor was abducted in Calabar happened while the gendarmes were in Integrated Peace and Development Unit Municipal. Separately, in January, a female pursuit of separatists agitating for (IPDU) early warning system, and to seek medical doctor was kidnapped in Akamkpa Ambazonia Republic in Southern Cameroon. feedback and input for response to mitigate LGA. areas of conflict. Gang/Cult Violence: In January, four people Recent Incidents or Patterns and Trends were reportedly killed during a rival cult Issues, March 2018 D ec 2 01 7 -Fe b 20 1 8 clash between Bendeghe Mafia and another local cult group in Boki LGA. A policeman Incidents reported during the month related According to Peace Map data (see Figure 1), was reportedly injured during a shootout mainly to communal tensions, criminality, incidents reported during this period with the cultists. Separately, a man was and cult violence. included communal violence, criminality, reportedly shot dead by members of a cult Communal Tensions: Eight people were militancy, cult violence, and child trafficking. group, known as the King Crackers during a reportedly killed during a clash over a land Communal Violence: In February, a political assembly in Calabar South LGA. -

A Case Study of Cross Rivers State, Nigeria
Business and Economic Research ISSN 2162-4860 2020, Vol. 10, No. 2 The Role of Non-State Actors in Strengthening the Developmental Capacity of the State: A Case Study of Cross Rivers State, Nigeria Felix Chukwudi Oparah Department Of Economics, University Of Calabar, Calabar, Nigeria Enya Ndem Bassey (Phd) Department Of Economics, University Of Calabar, Pmb 1115, Calabar, Nigeria Ohatu Ekoh Ohatu Department Of Economics, University Of Calabar, Calabar, Nigeria Email: [email protected] Received: February 13, 2020 Accepted: March 3, 2020 Published: April 23, 2020 doi:10.5296/ber.v10i2.16447 URL: https://doi.org/10.5296/ber.v10i2.16447 Abstract This study examined the role of Non State Actors (NSAs) in strengthening the developmental capacity of the state, using a case study of Cross River State, Nigeria. Primary and secondary data on selected constituents of NSAs including Non Governmental Organizations (NGOs), Privately Owned Companies, Banks, Private Hospitals and Private Schools were analyzed using tables and charts. The results revealed that activities of NSAs significantly enhance the developmental capacity of Cross River State especially in the areas of provision of public services, knowledge and skill acquisition, infrastructural development and employment generation. Besides other recommendations, it was recommended that NSAs and the government should perform complementary roles in enhancing developmental capacity and that the establishment of more NSAs in the rural areas should be encouraged through the provision of special funding and other incentives for NSAs that have their offices in the rural areas. Keywords: Non State Actors, Developmental capacity, NGOs, Cross River State 153 http://ber.macrothink.org Business and Economic Research ISSN 2162-4860 2020, Vol. -
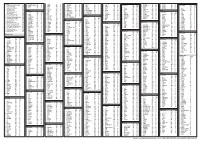
States and Lcdas Codes.Cdr
PFA CODES 28 UKANEFUN KPK AK 6 CHIBOK CBK BO 8 ETSAKO-EAST AGD ED 20 ONUIMO KWE IM 32 RIMIN-GADO RMG KN KWARA 9 IJEBU-NORTH JGB OG 30 OYO-EAST YYY OY YOBE 1 Stanbic IBTC Pension Managers Limited 0021 29 URU OFFONG ORUKO UFG AK 7 DAMBOA DAM BO 9 ETSAKO-WEST AUC ED 21 ORLU RLU IM 33 ROGO RGG KN S/N LGA NAME LGA STATE 10 IJEBU-NORTH-EAST JNE OG 31 SAKI-EAST GMD OY S/N LGA NAME LGA STATE 2 Premium Pension Limited 0022 30 URUAN DUU AK 8 DIKWA DKW BO 10 IGUEBEN GUE ED 22 ORSU AWT IM 34 SHANONO SNN KN CODE CODE 11 IJEBU-ODE JBD OG 32 SAKI-WEST SHK OY CODE CODE 3 Leadway Pensure PFA Limited 0023 31 UYO UYY AK 9 GUBIO GUB BO 11 IKPOBA-OKHA DGE ED 23 ORU-EAST MMA IM 35 SUMAILA SML KN 1 ASA AFN KW 12 IKENNE KNN OG 33 SURULERE RSD OY 1 BADE GSH YB 4 Sigma Pensions Limited 0024 10 GUZAMALA GZM BO 12 OREDO BEN ED 24 ORU-WEST NGB IM 36 TAKAI TAK KN 2 BARUTEN KSB KW 13 IMEKO-AFON MEK OG 2 BOSARI DPH YB 5 Pensions Alliance Limited 0025 ANAMBRA 11 GWOZA GZA BO 13 ORHIONMWON ABD ED 25 OWERRI-MUNICIPAL WER IM 37 TARAUNI TRN KN 3 EDU LAF KW 14 IPOKIA PKA OG PLATEAU 3 DAMATURU DTR YB 6 ARM Pension Managers Limited 0026 S/N LGA NAME LGA STATE 12 HAWUL HWL BO 14 OVIA-NORTH-EAST AKA ED 26 26 OWERRI-NORTH RRT IM 38 TOFA TEA KN 4 EKITI ARP KW 15 OBAFEMI OWODE WDE OG S/N LGA NAME LGA STATE 4 FIKA FKA YB 7 Trustfund Pensions Plc 0028 CODE CODE 13 JERE JRE BO 15 OVIA-SOUTH-WEST GBZ ED 27 27 OWERRI-WEST UMG IM 39 TSANYAWA TYW KN 5 IFELODUN SHA KW 16 ODEDAH DED OG CODE CODE 5 FUNE FUN YB 8 First Guarantee Pension Limited 0029 1 AGUATA AGU AN 14 KAGA KGG BO 16 OWAN-EAST -
A Review of Public Expenditure Management in Nigeria
Better systems, better health A REVIEW OF PUBLIC EXPENDITURE MANAGEMENT IN NIGERIA CROSS RIVER STATE REPORT February 2012 This publication was produced for review by the United States Agency for International Development. It was prepared by Marianne El-Khoury, Elizabeth Ohadi, Chinyere Omeogu, and Oluwaseun Adeleke for Health Systems 20/20 Project. Mission The Health Systems 20/20 cooperative agreement, funded by the U.S. Agency for International Development (USAID) for the period 2006–2011, helps USAID-supported countries address health system barriers to the use of life-saving priority health services. Health Systems 20/20 works to strengthen health systems through integrated approaches to improving financing, governance, and operations, and building sustainable capacity of local institutions. February 2012 For additional copies of this report, please email [email protected] or visit our website at www.healthsystems2020.org Cooperative Agreement No.: GHS-A-00-06-00010-00 Submitted to: Scott Stewart, AOTR Health Systems Division Office of Health, Infectious Disease and Nutrition Bureau for Global Health United States Agency for International Development Dr. Garoma Kena, MD, MPH, Activity Manager HIV/AIDS Team, Investing In People Office United States Agency for International Development/Nigeria Recommended Citation: El-Khoury, Marianne, Elizabeth Ohadi, Chinyere Omeogu, and Oluwaseun Adeleke. February 2012. A Review of Public Expenditure Management in Nigeria: Cross River State Report. Bethesda, MD: Health Systems 20/20 project, -

Cameroonian Refugee Situation, Nigeria 16 - 30 June 2018
EMERGENCY UPDATE Cameroonian refugee situation, Nigeria 16 - 30 June 2018 th th UNHCR, in collaboration with On 26 June, UNHCR was As of 30 June, a total of 81 Nigerian Government, started the officially granted by Buya refugee households printing of ID Cards for verified community (Obanliku Local benefited from shelter kits, to Cameroonian refugees, after the Government Area, Cross River build their own permanent decision to grant them state) 88 hectares of land to shelter in Anyake settlement Temporary Protection Status. host Cameroonian refugees. (Benue state). KEY INDICATORS 21,291 Cameroonian refugees registered with Level 1 registration Refugees and host community members march together in solidarity with refugees around the world © UNHCR/ C. Cavalcanti [October 2017 – March 2018] 3,267 Cameroonian refugees registered with biometrics [as of 30 June 2018] 1,235 Refugees and host community members march together in Cameroonian refugees relocated to Anyake settlement, solidarity with refugees around the world © UNHCR/ C. Cavalcanti Benue State [26 June 2018] Update On Achievements ■ World Refugee Day – the 20th June, on the occasion of World Refugee Day, several activities were carried out in Ikom (Cross River state) and Anyake settlement (Benue state), with the participation of refugees, UNHCR, Government officials, partners and host communities. Participants of all ages engaged themselves in sport competitions (soccer), dances, singing, drama and a march in solidarity with refugees around the world. ■ Protection – UNHCR, in collaboration with Nigerian Government, started issuing ID Cards to verified Cameroonian refugees aged from 14 years and above. This is in line with the Section 11 of the National Commission For Refugees Act which states that “Every person who has been granted refugee status under this Act, and members of his/her family, shall be issued with an Identity Card”. -

Cross River State, Nigeria
WORKING PAPER WORKING Use of Routine Health Information to Inform Budgetary Allocations for Reproductive Health in Cross River State, Nigeria Abiodun Hassan, MD, MPH November 2016 WP-16-168 FOREWORD We thank the United States Agency for International Development (USAID) for its support of the research and its publication. We also thank the USAID-funded MEASURE Evaluation project for its collaboration in implementing this baseline survey as the first step toward improving routine data demand and use for budget allocation in Cross River State. We are grateful to Dr. Abiodun Hassan, Monitoring and Evaluation Coordinator at ARFH, for his work and expertise on this research project, particularly with writing the research paper. We thank Ms. Bridgit Adamou, Family Planning Technical Advisor at MEASURE Evaluation, for her guidance both in the research and in the preparation of this report. Also deserving special attention and commendation are the Cross River State team, especially the staff of the Department of Planning, Research, and Statistics (PRS) and the budget office of the state ministry. Many thanks for the support we received from the state ethics committee and especially the role played by Dr. Comfort Ekanem, the former director of PRS and secretary of the Ethics Committee, who helped facilitate the review and approval of the survey protocol and who provided oversight of the conduct of the baseline assessment. Of note is the support we received from Mr. Oba N. Okina and Mr. Duke Bassey, who took pains to facilitate completion of the report and the dissemination meeting. Many thanks to all of the stakeholders and partners in Cross River and Calabar Municipal Local Government Areas (FHI360, Pathfinder, World Health Organization, Population Council, Budget Transparency and Accountability Initiative Nigeria, and the Health Strategy and Delivery Foundation) for their splendid support.