White Blood Cell Count and Eosinopenia As Valuable Tools for the Diagnosis of Bacterial Infections in the ED
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

• Cytosis: O Neutrophilia: Defined As an Increase in the Neutrophilic Count in the Peripheral Blood Above Reference Range for Age
HENATOLYMPHOID SYSTEM THIRD YEAR MEDICAL STUDENTS-UNIVERSITY OF JORDAN AHMAD T. MANSOUR, MD NONNEOPLASTIC DISEASES OF THE WHITE BLOOD CELLS • There are five major types of WBCs in the blood: neutrophils, lymphocytes, eosinophils, basophils and monocytes. • The normal function of the white blood cells depends on a tight regulation of their count and their function. Therefore, disease develops if there is a derangement of the cells count or function, it takes one of the following forms: o Cytosis: increase in the number of circulating cells above reference range. (Note: leukocytosis means an increase in the WBC count, neutrophilia means increase in the neutrophilic count, lymphocytosis means increase in the lymphocytic count, monocytosis means increase in the monocytic count, basophilia means increase in the basophilic count and eosinophilia means in crease in the eosinophilic count). o Cytopenia: decrease in the number of circulating cells below reference range. (Note: neutropenia means decreased neutrophils, lymphocytopenia, or simply lymphopenia, means decrease in lymphocytes, monocytopenia means decrease in monocytes, eosinopenia means decrease in eosinophils, and basopenia means decrease in basophils). o Abnormal or absent function • Cytosis: o Neutrophilia: defined as an increase in the neutrophilic count in the peripheral blood above reference range for age. o Causes: bacterial infection is the most common and most important etiology. Tissue necrosis in cases of burns or trauma and medications such as epinephrine and corticosteroids are also additional causes for neutrophilia. § Some physiologic conditions can lead to neutrophilia such as stress, smoking and pregnancy. o Pathophysiology: neutrophils are present in the blood in two populations: circulating and marginal (meaning neutrophils stuck to the vessel wall). -

Complete Blood Count in Primary Care
Complete Blood Count in Primary Care bpac nz better medicine Editorial Team bpacnz Tony Fraser 10 George Street Professor Murray Tilyard PO Box 6032, Dunedin Clinical Advisory Group phone 03 477 5418 Dr Dave Colquhoun Michele Cray free fax 0800 bpac nz Dr Rosemary Ikram www.bpac.org.nz Dr Peter Jensen Dr Cam Kyle Dr Chris Leathart Dr Lynn McBain Associate Professor Jim Reid Dr David Reith Professor Murray Tilyard Programme Development Team Noni Allison Rachael Clarke Rebecca Didham Terry Ehau Peter Ellison Dr Malcolm Kendall-Smith Dr Anne Marie Tangney Dr Trevor Walker Dr Sharyn Willis Dave Woods Report Development Team Justine Broadley Todd Gillies Lana Johnson Web Gordon Smith Design Michael Crawford Management and Administration Kaye Baldwin Tony Fraser Kyla Letman Professor Murray Tilyard Distribution Zane Lindon Lyn Thomlinson Colleen Witchall All information is intended for use by competent health care professionals and should be utilised in conjunction with © May 2008 pertinent clinical data. Contents Key points/purpose 2 Introduction 2 Background ▪ Haematopoiesis - Cell development 3 ▪ Limitations of reference ranges for the CBC 4 ▪ Borderline abnormal results must be interpreted in clinical context 4 ▪ History and clinical examination 4 White Cells ▪ Neutrophils 5 ▪ Lymphocytes 9 ▪ Monocytes 11 ▪ Basophils 12 ▪ Eosinophils 12 ▪ Platelets 13 Haemoglobin and red cell indices ▪ Low haemoglobin 15 ▪ Microcytic anaemia 15 ▪ Normocytic anaemia 16 ▪ Macrocytic anaemia 17 ▪ High haemoglobin 17 ▪ Other red cell indices 18 Summary Table 19 Glossary 20 This resource is a consensus document, developed with haematology and general practice input. We would like to thank: Dr Liam Fernyhough, Haematologist, Canterbury Health Laboratories Dr Chris Leathart, GP, Christchurch Dr Edward Theakston, Haematologist, Diagnostic Medlab Ltd We would like to acknowledge their advice, expertise and valuable feedback on this document. -

Anemic Syndrome and White Blood Cells Disorders
27. 11. 2020 Anemic syndrome and white blood cells disorders Kristína Repová, M.D., PhD. [email protected] Institute of Pathophysiology, Faculty of Medicine, Bratislava Prepared exclusively for the purposes of distance education at the Faculty of Medicine, Comenius University in Bratislava in 2020/21 Hematopoeisis • Hematopoietic organs: • Bone marrow: • forming of erythrocytes, granulocytes, monocytes, thrombocytes, partially lymphocytes • Thymus: • forming of T-lymphocytes • Lymphatic nodes, tonsils, spleen: • forming of B-lymphocytes lymphoid multipotent stem cell pluripotent progenitor cell precursor cell stem cell myleoid multipotent stem cell 1 27. 11. 2020 Hematopoeisis 3 Pluripotent hematopoietic stem cell (self-renewal) Myeloid multipotent Lymphoid multipotent stem cell stem cell Megacaryocyte and Granulocyte and T-cell and NK B-cell erythroid progenitor Macrophage progenitor cell progenitor progenitor Megacaryocyte Erythrocyte Granulocyte Monocyte progenitor progenitor progenitor progenitor (CFU-Meg) (CFU-E) (CFU-G) (CFU-M) Myeloblast NK-cell Proerythroblast Monoblast Lymphoblast Lymphoblast Promyelocyte Megacaryoblast Erythroblast Myelocyte Promonocyte Prolymphocyte Prolymphocyte Megacaryocyte Reticulocyte Metamyelocyte Monocyte T-cell B-cell Thrombocyte Erythrocyte Band cell Basophil Eosinophil Macrophage Dendritic cell Neutrophil 2 27. 11. 2020 I. Disorders of red blood cells II. Disorders of white blood cells III. Myeloproliferative and lymphoproliferative disorders I. Disorders of red blood cells 1. Anemia 2. -

Trapped Neutrophil Syndrome in a Border Collie Dog: Clinical, Clinico-Pathologic, and Molecular Findings
NOTE Internal Medicine Trapped Neutrophil Syndrome in a Border Collie Dog: Clinical, Clinico-Pathologic, and Molecular Findings Keijiro MIZUKAMI1), Tomoaki SHOUBUDANI2), Seira NISHIMOTO2), Ryuta KAWAMURA2), Akira YABUKI1) and Osamu YAMATO1)* 1)Laboratory of Clinical Pathology, Department of Veterinary Medicine, Kagoshima University, 1–21–24 Kohrimoto, Kagoshima 890–0065, Japan 2)Athena Pet Care Clinic, 3 Tamaike-cho, Nishi-ku, Nagoya 452–0812, Japan (Received 21 October 2011/Accepted 27 December 2011/Published online in J-STAGE 12 January 2012) ABSTRACT. Trapped neutrophil syndrome (TNS) is an autosomal recessive inherited neutropenia known in Border Collies since the 1990’s. Recently, the causative mutation has been identified in the canine VPS13B gene and a DNA-based diagnosis has now become available. The present paper describes clinical and clinico-pathologic findings in a Border Collie with TNS that was molecularly diag- nosed for the first time in Japan. In a 10-week-old male Border Collie with microgenesis and symptoms related to recurrent infections, a hematological examination revealed severe leukopenia due to neutropenia, suggesting the dog to be affected by inherited neutro- penic immunodeficiency. Direct DNA sequencing demonstrated that the dog was homozygous for the causative mutation of TNS and both its parents were heterozygous carriers. In addition, a simple and rapid polymerase chain reaction-based length polymorphism analysis coupled with microchip electrophoresis was developed for the genotyping of TNS. This assay could discriminate clearly all genotypes, suggesting that it was suitable for both individual diagnosis and large-scale surveys for prevention. KEY WORDS: Border Collie dog, Cohen syndrome, neutropenia, trapped neutrophil syndrome. -

The Importance of Eosinopenia for Predicting Treatment Response In
ORIGINAL ARTICLE The Importance of Eosinopenia for Predicting Treatment Response in Patients with Cholangitis Cengiz Karacaer1, Ahmet Tarik Eminler2, Bilal Toka2, Mukaddes Tozlu2, Erkan Parlak2 and Aydin Seref Koksal2 1Department of Internal Medicine, Sakarya University Research and Education Hospital, Sakarya, Turkey 2Department of Gastroenterology, Sakarya University Research and Education Hospital, Sakarya, Turkey ABSTRACT Objective: To compare recovery of eosinopenia, C-reactive protein (CRP) and procalcitonin levels in predicting the response to treatment in patients with cholangitis. Study Design: Descriptive, analytical study. Place and Duration of Study: Department of Gastroenterology, Sakarya Training and Research Hospital, Turkey between September 2018 and February 2019. Methodology: Patients with cholangitis, who underwent endoscopic retrograde cholangiopancreatography (ERCP), were inducted. Those with choledocholic thiasis alone were considered controls. Eosinophil count above 100.5 cells/µL was the limit value accepted as improvement. ERCP repeat was decided according to eosinophil count below 100.5 and not clinically improving. Relationship between inflammatory markers such as CRP, procalcitonin and eosinopenia values in patients with stone-associated cholangitis was investigated. Results: The cholangitis group was comprised of 62 patients [mean age 67±14.57 years; 26 (41.9%) female], while control group was comprised of 57 patients [mean age 57.4±18.10 years; 39 (68.4%) females, p=0.004].At time of admission, median eosinophils was significantly lower in cholangitis group at17.50 [9.82-84] ×103/µL compared to control group at168 [100.11-270] ×103/µL (p=0.001). ERCP were repeated on two patients as their clinical conditions and unremitting eosinophil counts worsened. Eosinophil and CRP markers and clinical improvement were observed after second ERCP procedure. -
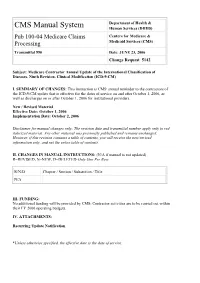
Pub 100-04 Medicare Claims Processing
Department of Health & CMS Manual System Human Services (DHHS) Pub 100-04 Medicare Claims Centers for Medicare & Processing Medicaid Services (CMS) Transmittal 990 Date: JUNE 23, 2006 Change Request 5142 Subject: Medicare Contractor Annual Update of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) I. SUMMARY OF CHANGES: This instruction is CMS' annual reminder to the contractors of the ICD-9-CM update that is effective for the dates of service on and after October 1, 2006, as well as discharges on or after October 1, 2006 for institutional providers. New / Revised Material Effective Date: October 1, 2006 Implementation Date: October 2, 2006 Disclaimer for manual changes only: The revision date and transmittal number apply only to red italicized material. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents. II. CHANGES IN MANUAL INSTRUCTIONS: (N/A if manual is not updated) R=REVISED, N=NEW, D=DELETED-Only One Per Row. R/N/D Chapter / Section / Subsection / Title N/A III. FUNDING: No additional funding will be provided by CMS; Contractor activities are to be carried out within their FY 2006 operating budgets. IV. ATTACHMENTS: Recurring Update Notification *Unless otherwise specified, the effective date is the date of service. Attachment – Recurring Update Notification Pub. 100-04 Transmittal: 990 Date: June 23, 2006 Change Request 5142 SUBJECT: Medicare Contractor Annual Update of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) I. -

N-Formyl-Methionyl-Leucyl-Phenylalanine in Man Thorax: First Published As 10.1136/Thx.47.4.284 on 1 April 1992
284 Thorax 1992;47:284-287 Haematological effects of inhalation of N-formyl-methionyl-leucyl-phenylalanine in man Thorax: first published as 10.1136/thx.47.4.284 on 1 April 1992. Downloaded from M J Peters, A B X Breslin, A S Kemp, J Chu, N Berend Abstract Background including chemotaxis, lysosomal enzyme N-Formyl-methionyl- release and oxygen free radical generation.4 leucyl-phenylalanine (FMLP) is a bac- It also contracts smooth muscle. There is a terial oligopeptide which stimulates close correlation between chemotactic and neutrophil chemotaxis, degranulation spasmogenic activity5 between the different and superoxide generation. Inhalation of related formyl peptides. Following the finding FMLP produces bronchoconstriction in that inhaled FMLP produces broncho- man; in the rabbit this is in part neutro- constriction in normal phil dependent. subjects,6 we suggested The effects of inhalation that it may cause bronchoconstriction during of FMLP on peripheral blood leucocytes bacterial bronchial infection, particularly in in normal subjects has been studied. patients with chronic airflow limitation. Methods This was an open study in Although FMLP contracts human bron- non-asthmatic subjects. Change in total chial smooth muscle directly in vitro,7 its peripheral white cell count were studied bronchoconstrictor activity in vivo in for 15 minutes after may inhalation of 04 part be neutrophil dependent as neutropenic umol FMLP in six subjects. Change rabbits show a reduced bronchoconstrictor in total and differential white cell count response to FMLP.8 Infusions of substances and spontaneous neutrophil chemi- known to activate neutrophils (FMLP, luminescence were then studied five and platelet activating factor (PAF), C5a, 30 minutes after inhalation of 0 4 pmol granulocyte-monocyte colony stimulating FMLP (n = 7) or diluent (n = 4). -

Evaluation of White Blood Cells Picture (Leukocytes) I-General the Term Leukocyte Include All White Blood Cells and Their Precursors
Dr.Iman Daham , BSci., MSc., PhD. Assist. Prof., Department of Internal and Preventive Medicine College of Veterinary Medicine, University of Mosul, Mosul, Iraq https://orcid.org/0000-0002-0947-7169 https://www.researchgate.net/profile/Iman Daham Clinical Pathology | Part I | 4th year 2019 Evaluation of White Blood Cells Picture (Leukocytes) I-General The term leukocyte include all white blood cells and their precursors. These cells use blood stream as a means of transport from their site of origin to the site in tissues where they are required . The circulating numbers therefore reflect the balance between supply and demand , and usually rang between about 5-14 ×10/L depending to some extent on species. The leukocytes can be divided in two basic categories: 1-The granulocytes which include Neutrophils , Eosinophil’s and Basophils. 2-Agranulocytes which include Lymphocytes and Monocytes. II-Alteration of the Leukocyte picture 1-Leukocytosis A-Physiological leukocytosis : a-age of animal: Total leukocyte count are higher in the young than in the adult of Dog and Cattle. Lowered leukocyte count in young animals than in adults appeared in Swine. No significant difference in total leukocyte count of young animal and adults in Horse and Sheep. b-Digestion is accompanied with leukocytosis as in Dog (one hour after digestion that reached its maximum about 3-4 hours and then declines) Horses have a weak digestion leukocytosis. c-Epinephrine injection. d-Pregnancy in cattle induces Leukocytosis with Neutrophilia especially two weeks before parturition. B-Pathological Leukocytosis: a-Acute infection by pyogenic bacteria as 1-Staphilococcus 2-Streptococcus. b-Rabies virus infection induces mild Leukocytosis. -

Hematological Profile of Normal Pregnant Women
Blood of & al L n y Mutua et al., J Blood Lymph 2018, 8:2 r m u p o h J Journal of Blood & Lymph DOI: 10.4172/2165-7831.1000220 ISSN: 2165-7831 Review Article Open Access Hematological Profile of Normal Pregnant Women David Nzioka Mutua1,2*, Eliud Nyaga Mwaniki Njagi1 and George Owino Orinda1 1Department of Biochemistry and Biotechnology, School of Pure and Applied Sciences, Kenyatta University, Nairobi, Kenya 2Department of Medical Biochemistry, School of Medicine and Health Sciences, Kenya Methodist University, Meru, Kenya Abstract With the advent of many interventions to improve maternal and child health, pregnant women have become the focus of many health programs. However, few data exist regarding this important population. Although pregnancy- induced changes occur in hematological values, very few laboratories provide specific reference ranges for pregnant women. Most laboratory information systems report reference values based on samples obtained from non–pregnant women which may not be useful for clinical decisions during pregnancy. Thus, there is an increased risk of overlooking important physiologic alterations resulting from pathological conditions and of misinterpreting normal changes as pathological events. It is therefore important to understand pregnancy-induced hematological changes for correct clinical evaluation of pregnant women. In this review, we discuss complete blood count and the associated pregnancy-induced hematological changes. We also highlight the dynamic changes of these parameters per trimester and show how they differ between populations. Keywords: Pregnancy; Complete blood count; Hematological Hematocrit (Hct), Hemoglobin (Hb or Hgb), Mean Corpuscular changes; Trimester Volume (MCV), Mean Corpuscular Hemoglobin (MCH), and Mean Corpuscular Hemoglobin Concentration (MCHC) [5,26]. -

Clozapine-Induced Late Agranulocytosis and Severe
Hindawi Publishing Corporation Case Reports in Medicine Volume 2015, Article ID 703218, 7 pages http://dx.doi.org/10.1155/2015/703218 Case Report Clozapine-Induced Late Agranulocytosis and Severe Neutropenia Complicated with Streptococcus pneumonia, Venous Thromboembolism, and Allergic Vasculitis in Treatment-Resistant Female Psychosis Christina Voulgari,1 Raphael Giannas,1 Georgios Paterakis,2 Anna Kanellou,1 Nikolaos Anagnostopoulos,3 and Stamata Pagoni1 1 3rd Department of Internal Medicine, Athens General Regional Hospital “G. Gennimatas”, Mesogeion Avenue 154, 11527Athens,Greece 2Flow Cytometry Laboratory, Department of Immunology, Athens General Regional Hospital “G. Gennimatas”, Athens, Greece 3Department of Hematology, Athens General Regional Hospital “G. Gennimatas”, Athens, Greece Correspondence should be addressed to Christina Voulgari; c v [email protected] Received 10 November 2014; Accepted 27 January 2015 Academic Editor: B. Carpiniello Copyright © 2015 Christina Voulgari et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Clozapine is a second-generation antipsychotic agent from the benzodiazepine group indicated for treatment-resistant schizophre- nia and other psychotic conditions. Using clozapine earlier on once a case appears to be refractory limits both social and personal morbidity of chronic psychosis. However treatment with second-generation antipsychotics is often complicated by adverse effects. We present a case of a 33-year-old Caucasian woman with a 25-year history of refractory psychotic mania after switching to a 2-year clozapine therapy. She presented clozapine-induced absolute neutropenia, agranulocytosis, which were complicated by Streptococcus pneumonia and sepsis. -

Wight Blood Pathology
WHITE BLOOD PATHOLOGY Alteration of leukocytes function, leukemia Normal distribution of white blood cells Total white cells count 4,0 – 11,0 x 10 9/L CELL ABSOLUTE PER sent % NUMBER x109 /L Neutrophils 2,5 – 7,5 58 - 72 BAND cells 0,04 – 0,4 1 - 6 Lymphocytes 1,5 – 4,0 19 -37 Monocytes 0,2 – 0,8 3 - 11 Eosinophils 0,04 – 0,4 1 - 6 Basophiles 0,01 – 0,1 0,5 - 1 Calculation of absolute or relative leukocytosis Example: Blood examination: Leukocytes – 1,5 x 109 /l segmented neutrophils – 15% Lymphocytes - 70% Estimate the absolute amount of neutrophils and lymphocytes Total amount of leukocytes 1,5 x 109 - 100% neutrophils X - 15% X= ( 1,5 x 109 x 15 ) : 100 = 0,225 x 109 ( 2,5 – 7,5 x109 ) Absolute neutropenia Total amount of leukocytes 1,5 x 10 9 - 100% lymphocytes X - 70% X = ( 1,5 x 109 x 70 ): 100 = 1,05 x 10 9 ( 1,5 – 4 x 10 9 ) Relative lymphocytosis Leukocytosis - ↑amount of L > 9 x 10 9 /L NEUTROPHILIA ← Causes: - infection, - APR, - tissue injury - hemorrhage, - neoplasm, - metabolic disorders, - stress states, - inflammation, - severe colic, - glucocorticoid administration. MONOCYTOSIS ← -chronic infection: tuberculosis, lepra, siphilis, malaria, rikketsiosis, endocarditis - infection mononucleosis, - vasculitis, - collagen disease EOSINOPHYLIA ← - allergy, - atopic diseases, - neoplasms, - chronic paracitic invasion, - dermatologic disorders LYMPHOCYTOSIS ← - acute viral infection, - hepatitis, - typhoid, - thyrotoxicosis, - adrenal insufficiency - infectious mononucleosis LYMPHOCYTOSIS NON – MELIGNANT CAUSES OF LYMPHOSITOSIS -

(WBC) Interpretive Summary
White Blood Cells (WBC) Interpretive Summary Description: White blood cells are part of the immune system and defend against infectious diseases and foreign substances. Decreased White Blood Cells Common Causes Decreased bone marrow production o Infection . Parvovirus in dogs and cats . Feline leukemia virus . Toxoplasmosis . Rickettsial disease o Neoplasia Increased tissue demand o Sepsis o Viral infections o Sequestration: collection of cells within an organ system or body compartment: abscess, pyometra, peritonitis, pneumonia, necrotic tumor, etc. Toxicity o Chemotherapy o Estrogens o Chloramphenicol, sulfas o Idiosyncratic drug reactions, toxicities Uncommon Causes Decreased bone marrow production o Immune-mediated destruction within the bone marrow o Bone marrow fibrosis, aplasia o Idiopathic Peripheral destruction by immune or other mechanisms Related Findings Decreased bone marrow production o Decreases in all three cell lines (red blood cells, white blood cells and platelets) or two of three cell lines may suggest a bone marrow disorder o Infection . Positive serology or PCR tests for infectious organisims . WBC morphologic abnormalities such as toxicity, reactive lymphocytes o Neoplasia . Nonregenerative anemia, thrombocytopenia, and/or leukopenia . Atypical or unclassified cells found on blood smear evaluation . Neoplastic cells on bone marrow aspirate cytology or biopsy Increased tissue demand o Sepsis . Toxic neutrophils and/or band neutrophils . Increased PT and PTT, decreased platelets and fibrinogen (due to DIC) . Positive culture of urine, CSF, joint fluid, blood, tissue, body cavity effusion, other . Pleural effusion or pneumonia on thoracic radiographs Generated by VetConnect® PLUS: White Blood Cells (WBC) Page 1 of 3 . Peritoneal effusion, prostatic abscess/prostatitis, pyometra, or necrotic mass on thoracic or abdominal radiographs, or abdominal ultrasound .