Feline Cytauxzoonosis Marcella D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Molecular Parasitology Protozoan Parasites and Their Molecules Molecular Parasitology Julia Walochnik • Michael Duchêne Editors
Julia Walochnik Michael Duchêne Editors Molecular Parasitology Protozoan Parasites and their Molecules Molecular Parasitology Julia Walochnik • Michael Duchêne Editors Molecular Parasitology Protozoan Parasites and their Molecules Editors Julia Walochnik Michael Duchêne Institute of Specifi c Prophylaxis Institute of Specifi c Prophylaxis and Tropical Medicine and Tropical Medicine Center for Pathophysiology, Infectiology Center for Pathophysiology, Infectiology and Immunology and Immunology Medical University of Vienna Medical University of Vienna Vienna Vienna Austria Austria ISBN 978-3-7091-1415-5 ISBN 978-3-7091-1416-2 (eBook) DOI 10.1007/978-3-7091-1416-2 Library of Congress Control Number: 2016947730 © Springer-Verlag Wien 2016 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specifi c statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The publisher, the authors and the editors are safe to assume that the advice and information in this book are believed to be true and accurate at the date of publication. Neither the publisher nor the authors or the editors give a warranty, express or implied, with respect to the material contained herein or for any errors or omissions that may have been made. -

Feline Cytauxzoonosis
Article #5 CE Feline Cytauxzoonosis Peter J. Bondy, Jr, DVM, MS, DACVIM Leah A. Cohn, DVM, PhD, DACVIM Marie E. Kerl, DVM, DACVIM, DACVECC University of Missouri ABSTRACT: Cytauxzoon felis is a protozoal organism transmitted to cats through a tick bite. Region- ally restricted to the south central and southeastern United States, C. felis infection of domestic cats is usually fatal.The parasite life cycle includes both a tissue and an erythro- cytic phase.The clinical disease course is rapid, with onset of fever, lethargy, and anorexia 5 to 20 days after infection and death within a week of initial signs. Leukocytosis, hemolytic anemia, icterus, and elevated liver enzymes are usually present. Definitive diag- nosis is based on microscopic identification of parasites. Effective medical therapy remains elusive, although several cats have reportedly survived. ytauxzoon felis is a protozoal organism schizont phase of the genus Theileria occurs in that causes fatal illness in domestic lymphocytic cells.3 The infected macrophage cats. It is related to other Cytauxzoon cells occlude venules in the liver, spleen, lung, C 1 spp of African ungulates and was first recog- and lymph nodes (Figure 2). The schizont nized in Missouri in 1976.1 Geographically phase is most closely associated with clinical limited primarily to the south central and disease, and the degree of schizogony is southeastern United States (Figure 1), C. felis reflected in the severity of illness.4 In domestic seems to infect only felidae and therefore cats, the schizont burden is extensive, whereas it poses no zoonotic or agricultural risk.2 Diag- is usually small and brief in mildly affected nosing cytauxzoonosis in cats is based on com- species such as the bobcat.5 patible clinical signs and identifying the Fission of the schizonts results in formation organisms in tissue or blood. -

An Intestinal Gregarine of Nothria Conchylega (Polychaeta, Onuphidae)
Journal of Invertebrate Pathology 104 (2010) 172–179 Contents lists available at ScienceDirect Journal of Invertebrate Pathology journal homepage: www.elsevier.com/locate/jip Description of Trichotokara nothriae n. gen. et sp. (Apicomplexa, Lecudinidae) – An intestinal gregarine of Nothria conchylega (Polychaeta, Onuphidae) Sonja Rueckert *, Brian S. Leander Canadian Institute for Advanced Research, Program in Integrated Microbial Biodiversity, Departments of Botany and Zoology, University of British Columbia, #3529 – 6270 University Blvd., Vancouver, BC, Canada V6T 1Z4 article info abstract Article history: The trophozoites of a novel gregarine apicomplexan, Trichotokara nothriae n. gen. et sp., were isolated and Received 12 November 2009 characterized from the intestines of the onuphid tubeworm Nothria conchylega (Polychaeta), collected at Accepted 11 March 2010 20 m depth from the North-eastern Pacific Coast. The trophozoites were 50–155 lm long with a mid-cell Available online 23 March 2010 indentation that formed two prominent bulges (anterior bulge, 14–48 lm wide; posterior bulge, 15– 55 lm wide). Scanning electron microscopy (SEM) demonstrated that approximately 400 densely packed, Keywords: longitudinal epicytic folds (5 folds/lm) inscribe the surface of the trophozoites, and a prominently elon- Alveolata gated mucron (14–60 lm long and 6–12 lm wide) was covered with hair-like projections (mean length, Apicomplexa 1.97 m; mean width, 0.2 m at the base). Although a septum occurred at the junction between the cell Lecudinidae l l Lecudina proper and the mucron in most trophozoites, light microscopy (LM) demonstrated that the cell proper Parasite extended into the core of the mucron as a thin prolongation. -

Feline Immune Response to Infection with Cytauxzoon Felis and The
FELINE IMMUNE RESPONSE TO INFECTION WITH CYTAUXZOON FELIS AND THE ROLE OF CD18 IN THE PATHOGENESIS OF CYTAUXZOONOSIS by KARELMA FRONTERA-ACEVEDO (Under the Direction of Kaori Sakamoto) ABSTRACT Cytauxzoonosis is a highly fatal, hemoprotozoal disease of cats in the Mid-Western, Mid- Atlantic, and Southeastern United States, caused by Cytauxzoon felis. Although the causative agent has been recognized since 1976, no study has profiled the immune response of infected cats, there is no definitive cure, and C. felis has not been successfully maintained in cell cultures in vitro, thwarting research efforts. One of the main histopathologic characteristics of this disease is the presence of giant, infected, intravascular macrophages, many of which are adhered to the vascular endothelium. The main goals of this project are: 1) to characterize the feline immune response to C. felis; 2) to develop a cell culture system in order to study C. felis in vitro; and 3) to determine whether CD18 plays a role in the pathogenesis of cytauxzoonosis. INDEX WORDS: Cat, Cytauxzoon felis, pathogenesis, protozoal disease, veterinary pathology FELINE IMMUNE RESPONSE TO INFECTION WITH CYTAUXZOON FELIS AND THE ROLE OF CD18 IN THE PATHOGENESIS OF CYTAUXZOONOSIS by KARELMA FRONTERA-ACEVEDO BS, University of Florida, 2004 DVM, Louisiana State University, 2008 A Dissertation Submitted to the Graduate Faculty of The University of Georgia in Partial Fulfillment of the Requirements for the Degree DOCTOR OF PHILOSOPHY ATHENS, GEORGIA 2013 © 2013 Karelma Frontera-Acevedo All -

Transmission of Cytauxzoon Felis by Amblyomma Americanum: Engorgement Weight of Nymphs and Attachment Time of Adults for Transmission to Domestic Cats
TRANSMISSION OF CYTAUXZOON FELIS BY AMBLYOMMA AMERICANUM: ENGORGEMENT WEIGHT OF NYMPHS AND ATTACHMENT TIME OF ADULTS FOR TRANSMISSION TO DOMESTIC CATS By YOKO NAGAMORI Bachelor of Arts in Biology Augustana University Sioux Falls, South Dakota 2008 Doctor of Veterinary Medicine Iowa State University Ames, Iowa 2013 Submitted to the Faculty of the Graduate College of the Oklahoma State University in partial fulfillment of the requirements for the Degree of MASTER OF SCIENCE July, 2016 TRANSMISSION OF CYTAUXZOON FELIS BY AMBLYOMMA AMERICANUM: ENGORGEMENT WEIGHT OF NYMPHS AND ATTACHMENT TIME OF ADULTS FOR TRANSMISSION TO DOMESTIC CATS Thesis Approved: Dr. Mason V. Reichard Thesis Adviser Dr. Susan E. Little Dr. James Meinkoth Dr. Mark Payton ii ACKNOWLEDGEMENTS I would like to thank my thesis advisor, Dr. Mason V. Reichard, MS, PhD Associate Professor in Veterinary Pathobiology as well as the rest of my master’s committee Dr. Susan E. Little, DVM, PhD, DACVM-Parasit Regents Professor and Krull-Ewing Chair in Veterinary Parasitology, Dr. Mark Payton PhD Regents Service Professor and Department Head of Statistics, and Dr. James Meinkoth, DVM, PhD Professor in Veterinary Pathobiology for their support, time, and dedication. Additional support for this project came from Dr. Jennifer E. Slovak DVM, MS, DACVIM Assistant Professor in Small Animal Internal Medicine at Washington State University College of Veterinary Medicine for sending me blood samples from Ames, Iowa, Operation Catnip Stillwater for allowing me to collect blood samples from free-roaming cats, and Lisa Coburn and the Tick Laboratory. I would also like to show my special gratitude to Dr. Eileen Johnson DVM, MS, PhD Clinical Associate Professor Emerita and Rebecca Duncan-Decocq, MS for their unconditional support. -

Redalyc.Cytauxzoon Felis and 'Candidatus Mycoplasma
Revista Brasileira de Parasitologia Veterinária ISSN: 0103-846X [email protected] Colégio Brasileiro de Parasitologia Veterinária Brasil Mendes Pupio Maia, Leticia; de Mello Figueiredo Cerqueira, Aloysio; de Barros Macieira, Daniel; Moreira de Souza, Aline; Santos Moreira, Namir; Vieira da Silva, Adrianna; Belle Messick, Joanne; Fernandes Ferreira, Renata; Pereira Almosny, Nádia Regina Cytauxzoon felis and ‘Candidatus Mycoplasma haemominutum’ coinfection in a Brazilian domestic cat (Felis catus) Revista Brasileira de Parasitologia Veterinária, vol. 22, núm. 2, abril-junio, 2013, pp. 289- 291 Colégio Brasileiro de Parasitologia Veterinária Jaboticabal, Brasil Available in: http://www.redalyc.org/articulo.oa?id=397841488019 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Research Note Rev. Bras. Parasitol. Vet., Jaboticabal, v. 22, n. 2, p. 289-291, abr.-jun. 2013 ISSN 0103-846X (impresso) / ISSN 1984-2961 (eletrônico) Cytauxzoon felis and ‘Candidatus Mycoplasma haemominutum’ coinfection in a Brazilian domestic cat (Felis catus) Co-infecção por Cytauxzoon felis e ‘Candidatus Mycoplasma haemominutum’ em um gato doméstico (Felis catus) no Brasil Leticia Mendes Pupio Maia1; Aloysio de Mello Figueiredo Cerqueira2; Daniel de Barros Macieira1; Aline Moreira de Souza1; Namir Santos Moreira1; Adrianna Vieira -

Cytauxzoon Felis Infection in Domestic Cats, Yunnan Province, China, 2016
Cytauxzoon felis Infection in Domestic Cats, Yunnan Province, China, 2016 Feng-Cai Zou,1 Zhao Li,1 Jian-Fa Yang, cats and 237 pet cats) in Yunnan Province in southwestern Jiang-Yan Chang, Guo-Hua Liu, China using EDTA tubes. We stored these EDTA whole Yan Lv, Xing-Quan Zhu blood samples at –20°C and then performed genomic DNA extraction with the TIANamp Genomic DNA Kit (TianGen, We performed a molecular survey for Cytauxzoon felis http://www.tiangen.com) following the manufacturer’s pro- infection in 311 domestic cats in Yunnan Province, China, tocol. To detect C. felis infection, we performed a PCR tar- in 2016 and found a prevalence of 21.5%. C. felis infection geting the second internal transcribed spacer (ITS-2) of ribo- in domestic and wild cats in other provinces should be investigated to determine parasite prevalence and genetic somal DNA (6). We sequenced amplicons in both directions diversity among cats throughout China. and compared these sequences with those of other relevant C. felis isolates available in GenBank. We analyzed differ- ences in C. felis prevalence in domestic cats according to ytauxzoonosis is a tickborne hemoprotozoal disease lifestyle, region, sex, and age using the χ2 test in SPSS 22.0 Cof both domestic cats and wild felids caused mainly standard version for Windows (IBM Corporation, https:// by Cytauxzoon felis protozoa (1,2). In the late 1900s, C. www.ibm.com). We considered differences statistically sig- felis protozoa were reported exclusively in North America, nificant when the p value obtained was <0.05. particularly in the mid-Atlantic states of the United States In total, 67 (21.5%) of 311 examined domestic cats (3), but in the early 2000s, this pathogen was reported in some were positive for the C. -

Highly Rearranged Mitochondrial Genome in Nycteria Parasites (Haemosporidia) from Bats
Highly rearranged mitochondrial genome in Nycteria parasites (Haemosporidia) from bats Gregory Karadjiana,1,2, Alexandre Hassaninb,1, Benjamin Saintpierrec, Guy-Crispin Gembu Tungalunad, Frederic Arieye, Francisco J. Ayalaf,3, Irene Landaua, and Linda Duvala,3 aUnité Molécules de Communication et Adaptation des Microorganismes (UMR 7245), Sorbonne Universités, Muséum National d’Histoire Naturelle, CNRS, CP52, 75005 Paris, France; bInstitut de Systématique, Evolution, Biodiversité (UMR 7205), Sorbonne Universités, Muséum National d’Histoire Naturelle, CNRS, Université Pierre et Marie Curie, CP51, 75005 Paris, France; cUnité de Génétique et Génomique des Insectes Vecteurs (CNRS URA3012), Département de Parasites et Insectes Vecteurs, Institut Pasteur, 75015 Paris, France; dFaculté des Sciences, Université de Kisangani, BP 2012 Kisangani, Democratic Republic of Congo; eLaboratoire de Biologie Cellulaire Comparative des Apicomplexes, Faculté de Médicine, Université Paris Descartes, Inserm U1016, CNRS UMR 8104, Cochin Institute, 75014 Paris, France; and fDepartment of Ecology and Evolutionary Biology, University of California, Irvine, CA 92697 Contributed by Francisco J. Ayala, July 6, 2016 (sent for review March 18, 2016; reviewed by Sargis Aghayan and Georges Snounou) Haemosporidia parasites have mostly and abundantly been de- and this lack of knowledge limits the understanding of the scribed using mitochondrial genes, and in particular cytochrome evolutionary history of Haemosporidia, in particular their b (cytb). Failure to amplify the mitochondrial cytb gene of Nycteria basal diversification. parasites isolated from Nycteridae bats has been recently reported. Nycteria parasites have been primarily described, based on Bats are hosts to a diverse and profuse array of Haemosporidia traditional taxonomy, in African insectivorous bats of two fami- parasites that remain largely unstudied. -
Troccap-Feline-Endo-Guidelines
Disclaimer The guidelines presented in this booklet were independently developed by members of the Tropical Council for Companion Animal Parasites Ltd. These best-practice guidelines are based on evidence-based, peer reviewed, published scientific literature. The authors of these guidelines have made considerable efforts to ensure the information upon which they are based is accurate and up-to-date. Individual circumstances must be taken into account where appropriate when following the recommendations in these guidelines. Sponsors The Tropical Council for Companion Animal Parasites Ltd. wish to acknowledge the kind donations of our sponsors for facilitating the publication of these freely available guidelines. Contents General considerations and recommendations .......................................................... 1 Diagnosis ................................................................................................................ 1 Treatment ............................................................................................................... 1 Prevention and control ............................................................................................ 1 Public health considerations ................................................................................... 2 Gastrointestinal Parasites .......................................................................................... 3 Ascarids (Toxocara spp., Toxascaris leonina) ........................................................ 3 Hookworms (Ancylostoma -

Revisions to the Classification, Nomenclature, and Diversity of Eukaryotes
University of Rhode Island DigitalCommons@URI Biological Sciences Faculty Publications Biological Sciences 9-26-2018 Revisions to the Classification, Nomenclature, and Diversity of Eukaryotes Christopher E. Lane Et Al Follow this and additional works at: https://digitalcommons.uri.edu/bio_facpubs Journal of Eukaryotic Microbiology ISSN 1066-5234 ORIGINAL ARTICLE Revisions to the Classification, Nomenclature, and Diversity of Eukaryotes Sina M. Adla,* , David Bassb,c , Christopher E. Laned, Julius Lukese,f , Conrad L. Schochg, Alexey Smirnovh, Sabine Agathai, Cedric Berneyj , Matthew W. Brownk,l, Fabien Burkim,PacoCardenas n , Ivan Cepi cka o, Lyudmila Chistyakovap, Javier del Campoq, Micah Dunthornr,s , Bente Edvardsent , Yana Eglitu, Laure Guillouv, Vladimır Hamplw, Aaron A. Heissx, Mona Hoppenrathy, Timothy Y. Jamesz, Anna Karn- kowskaaa, Sergey Karpovh,ab, Eunsoo Kimx, Martin Koliskoe, Alexander Kudryavtsevh,ab, Daniel J.G. Lahrac, Enrique Laraad,ae , Line Le Gallaf , Denis H. Lynnag,ah , David G. Mannai,aj, Ramon Massanaq, Edward A.D. Mitchellad,ak , Christine Morrowal, Jong Soo Parkam , Jan W. Pawlowskian, Martha J. Powellao, Daniel J. Richterap, Sonja Rueckertaq, Lora Shadwickar, Satoshi Shimanoas, Frederick W. Spiegelar, Guifre Torruellaat , Noha Youssefau, Vasily Zlatogurskyh,av & Qianqian Zhangaw a Department of Soil Sciences, College of Agriculture and Bioresources, University of Saskatchewan, Saskatoon, S7N 5A8, SK, Canada b Department of Life Sciences, The Natural History Museum, Cromwell Road, London, SW7 5BD, United Kingdom -
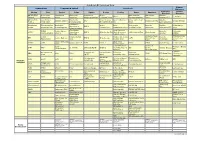
Iipcr Assay List 2020.Xlsx
GeneReach Biotechnology Corp. Human Aquaculture Companion animal Livestock Diseases Emerging Human Shrimp Fish Canine Feline Equine Bovine Poultry Swine Ruminant Diseases Diseases AHPND/EMS Aeromonas Anaplasma Bartonella Anaplasma Bovine Actinobacillus Bluetongue Bacillus ALV-J C. difficile Plasmid salmonicida platys henselae phagocytophilum Leukemia Virus Pleuropneumonia Virus anthracis PL3 AHPND/EMS Carp Edema Bordetella Bovine Papular Avian Influenza Africa Swine Fever Bacillus Babesia gibsoni EAV Brucella abortus Chagas Disease Toxin 1 Virus (CEV) bronchiseptica Stomatitis Virus H9 Virus anthracis pXO1 Candidatus Baculovirus Flavobacterium Bordetella Bovine Avian Brachyspira Brucella Bacillus Chikungunya Mycoplasma EHV-1 penaei psychrophilum bronchiseptica Tuberculosis metapneumovirus hyodysenteriae melitensis anthracis pXO2 virus haemominutum Candidatus Avian Reovirus IRIDO- Canine Adeno Brucella Chlamydia CMNV Mycoplasma EHV-3 Brucella abortus (Asia & America Chlamydia psittaci Brucella spp. Megalocytivirus Virus 2 abortus psittaci turicensis regions only) Crimean-Congo Crimean–Congo IRIDO- Chlamydophila Chicken infectious Brucella EHP Canine Babesia EHV-4 Brucella spp. CSFV Hemorrhagic hemorrhagic Ranaviruses felis anemia virus melitensis Fever fever Canine Influenza Duck Virus IHHNV ISAV Cytauxzoon felis EIAV BVDV-1 FMDV FMDV Brucella spp. Dengue Virus Virus Enteritis Virus Fowl adenovirus Infectious Canine Filariasis (Brugia IMNV KHV D. immitis Influenza H3N8 BVDV-2 (Pan Adv, type 4, JEV Bovine Chagas disease Leishmaniasis spp.) -

Emerging Human Babesiosis with “Ground Zero” in North America
microorganisms Review Emerging Human Babesiosis with “Ground Zero” in North America Yi Yang 1, Jevan Christie 2, Liza Köster 3 , Aifang Du 1,* and Chaoqun Yao 4,* 1 Department of Veterinary Medicine, College of Animal Sciences, Zhejiang Provincial Key Laboratory of Preventive Veterinary Medicine, Zhejiang University, Hangzhou 310058, China; [email protected] 2 The Animal Hospital, Murdoch University, 90 South Street, Murdoch, WA 6150, Australia; [email protected] 3 Department of Small Animal Clinical Sciences, College of Veterinary Medicine, University of Tennessee, 2407 River Drive, Knoxville, TN 37996, USA; [email protected] 4 Department of Biomedical Sciences and One Health Center for Zoonoses and Tropical Veterinary Medicine, Ross University School of Veterinary Medicine, Basseterre 00334, Saint Kitts and Nevis * Correspondence: [email protected] (A.D.); [email protected] (C.Y.) Abstract: The first case of human babesiosis was reported in the literature in 1957. The clinical disease has sporadically occurred as rare case reports in North America and Europe in the subsequent decades. Since the new millennium, especially in the last decade, many more cases have apparently appeared not only in these regions but also in Asia, South America, and Africa. More than 20,000 cases of human babesiosis have been reported in North America alone. In several cross-sectional surveys, exposure to Babesia spp. has been demonstrated within urban and rural human populations with clinical babesiosis reported in both immunocompromised and immunocompetent humans. This review serves to highlight the widespread distribution of these tick-borne pathogens in humans, their tick vectors in readily accessible environments such as parks and recreational areas, and their Citation: Yang, Y.; Christie, J.; Köster, phylogenetic relationships.