Emerging Human Babesiosis with “Ground Zero” in North America
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Basal Body Structure and Composition in the Apicomplexans Toxoplasma and Plasmodium Maria E
Francia et al. Cilia (2016) 5:3 DOI 10.1186/s13630-016-0025-5 Cilia REVIEW Open Access Basal body structure and composition in the apicomplexans Toxoplasma and Plasmodium Maria E. Francia1* , Jean‑Francois Dubremetz2 and Naomi S. Morrissette3 Abstract The phylum Apicomplexa encompasses numerous important human and animal disease-causing parasites, includ‑ ing the Plasmodium species, and Toxoplasma gondii, causative agents of malaria and toxoplasmosis, respectively. Apicomplexans proliferate by asexual replication and can also undergo sexual recombination. Most life cycle stages of the parasite lack flagella; these structures only appear on male gametes. Although male gametes (microgametes) assemble a typical 9 2 axoneme, the structure of the templating basal body is poorly defined. Moreover, the rela‑ tionship between asexual+ stage centrioles and microgamete basal bodies remains unclear. While asexual stages of Plasmodium lack defined centriole structures, the asexual stages of Toxoplasma and closely related coccidian api‑ complexans contain centrioles that consist of nine singlet microtubules and a central tubule. There are relatively few ultra-structural images of Toxoplasma microgametes, which only develop in cat intestinal epithelium. Only a subset of these include sections through the basal body: to date, none have unambiguously captured organization of the basal body structure. Moreover, it is unclear whether this basal body is derived from pre-existing asexual stage centrioles or is synthesized de novo. Basal bodies in Plasmodium microgametes are thought to be synthesized de novo, and their assembly remains ill-defined. Apicomplexan genomes harbor genes encoding δ- and ε-tubulin homologs, potentially enabling these parasites to assemble a typical triplet basal body structure. -
Distribution of Tick-Borne Diseases in China Xian-Bo Wu1, Ren-Hua Na2, Shan-Shan Wei2, Jin-Song Zhu3 and Hong-Juan Peng2*
Wu et al. Parasites & Vectors 2013, 6:119 http://www.parasitesandvectors.com/content/6/1/119 REVIEW Open Access Distribution of tick-borne diseases in China Xian-Bo Wu1, Ren-Hua Na2, Shan-Shan Wei2, Jin-Song Zhu3 and Hong-Juan Peng2* Abstract As an important contributor to vector-borne diseases in China, in recent years, tick-borne diseases have attracted much attention because of their increasing incidence and consequent significant harm to livestock and human health. The most commonly observed human tick-borne diseases in China include Lyme borreliosis (known as Lyme disease in China), tick-borne encephalitis (known as Forest encephalitis in China), Crimean-Congo hemorrhagic fever (known as Xinjiang hemorrhagic fever in China), Q-fever, tularemia and North-Asia tick-borne spotted fever. In recent years, some emerging tick-borne diseases, such as human monocytic ehrlichiosis, human granulocytic anaplasmosis, and a novel bunyavirus infection, have been reported frequently in China. Other tick-borne diseases that are not as frequently reported in China include Colorado fever, oriental spotted fever and piroplasmosis. Detailed information regarding the history, characteristics, and current epidemic status of these human tick-borne diseases in China will be reviewed in this paper. It is clear that greater efforts in government management and research are required for the prevention, control, diagnosis, and treatment of tick-borne diseases, as well as for the control of ticks, in order to decrease the tick-borne disease burden in China. Keywords: Ticks, Tick-borne diseases, Epidemic, China Review (Table 1) [2,4]. Continuous reports of emerging tick-borne Ticks can carry and transmit viruses, bacteria, rickettsia, disease cases in Shandong, Henan, Hebei, Anhui, and spirochetes, protozoans, Chlamydia, Mycoplasma,Bartonia other provinces demonstrate the rise of these diseases bodies, and nematodes [1,2]. -

Babesia Species
Laboratory diagnosis of babesiosis Babesia species Basic guidelines A. Capillary blood should be obtained by fingerstick, or venous blood should be obtained by venipuncture. B. Blood smears, at least two thick and two thin, should be prepared as soon as possible after col- lection. Delay in preparation of the smears can result in changes in parasite morphology and staining characteristics. In Babesia infections, infected red blood cells (rbcs) are normal in size. Typically rings are seen, and they may be vacuolated, pleomorphic or pyriform. Extracellular or tetrad-forms may also be present. Unlike Plasmodium spp., Babesia organisms lack pigment. Rings Rings of Babesia spp. have delicate cytoplasm and are often pleomorphic. Infected rbcs are not enlarged; multiple infection of rbcs can be common. Rings are usually vacuolated and do not produce pigment. Oc- casional classic tetrad-forms (Maltese Cross) or extracellular rings can be present. Rings of Babesia sp. in thick blood smears. Thin, delicate rings of Babesia sp. in a Babesia sp. in a thin blood smear, Thin blood smear showing a cluster of thin blood smear. showing pleomorphic rings and multiply- extracellular rings. infected rbcs. Laboratory diagnosis of babesiosis Babesia species Babesia microti in a thin blood smear. Note Babesia microti in thin blood smears. Notice the vacuolated and pleomorphic rings and multi- the classic “Maltese Cross” tetrad-form in ply-infected rbcs. Notice also there is no pigment present in any of the parasites. the infected rbc in the lower part of the image. Babesia sp. in a thin blood smear stained with Giemsa, showing pleomorphic rings and Babesia sp. -

Severe Babesiosis Caused by Babesia Divergens in a Host with Intact Spleen, Russia, 2018 T ⁎ Irina V
Ticks and Tick-borne Diseases 10 (2019) 101262 Contents lists available at ScienceDirect Ticks and Tick-borne Diseases journal homepage: www.elsevier.com/locate/ttbdis Severe babesiosis caused by Babesia divergens in a host with intact spleen, Russia, 2018 T ⁎ Irina V. Kukinaa, Olga P. Zelyaa, , Tatiana M. Guzeevaa, Ludmila S. Karanb, Irina A. Perkovskayac, Nina I. Tymoshenkod, Marina V. Guzeevad a Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russian Federation b Central Research Institute of Epidemiology, Moscow, Russian Federation c Infectious Clinical Hospital №2 of the Moscow Department of Health, Moscow, Russian Federation d Centre for Hygiene and Epidemiology in Moscow, Moscow, Russian Federation ARTICLE INFO ABSTRACT Keywords: We report a case of severe babesiosis caused by the bovine pathogen Babesia divergens with the development of Protozoan parasites multisystem failure in a splenic host. Immunosuppression other than splenectomy can also predispose people to Babesia divergens B. divergens. There was heavy multiple invasion of up to 14 parasites inside the erythrocyte, which had not been Ixodes ricinus previously observed even in asplenic hosts. The piroplasm 18S rRNA sequence from our patient was identical B. Tick-borne disease divergens EU lineage with identity 99.5–100%. Human babesiosis 1. Introduction Leucocyte left shift with immature neutrophils, signs of dysery- thropoiesis, anisocytosis, and poikilocytosis were seen on the peripheral Babesia divergens, a protozoan blood parasite (Apicomplexa: smear. Numerous intra-erythrocytic parasites were found, which were Babesiidae) is primarily specific to bovines. This parasite is widespread initially falsely identified as Plasmodium falciparum. The patient was throughout Europe within the vector Ixodes ricinus. -

And Toxoplasmosis in Jackass Penguins in South Africa
IMMUNOLOGICAL SURVEY OF BABESIOSIS (BABESIA PEIRCEI) AND TOXOPLASMOSIS IN JACKASS PENGUINS IN SOUTH AFRICA GRACZYK T.K.', B1~OSSY J.].", SA DERS M.L. ', D UBEY J.P.···, PLOS A .. ••• & STOSKOPF M. K .. •••• Sununary : ReSlIlIle: E x-I1V\c n oN l~ lIrIUSATION D'Ar\'"TIGENE DE B ;IB£,'lA PH/Re El EN ELISA ET simoNi,cATIVlTli t'OUR 7 bxo l'l.ASMA GONIJfI DE SI'I-IENICUS was extracted from nucleated erythrocytes Babesia peircei of IJEMIiNSUS EN ArRIQUE D U SUD naturally infected Jackass penguin (Spheniscus demersus) from South Africo (SA). Babesia peircei glycoprotein·enriched fractions Babesia peircei a ele extra it d 'erythrocytes nue/fies p,ovenanl de Sphenicus demersus originoires d 'Afrique du Sud infectes were obto ined by conca navalin A-Sepharose affinity column natulellement. Des fractions de Babesia peircei enrichies en chromatogrophy and separated by sod ium dodecyl sulphate glycoproleines onl ele oblenues par chromatographie sur colonne polyacrylam ide gel electrophoresis (SDS-PAGE ). At least d 'alfinite concona valine A-Sephorose et separees par 14 protein bonds (9, 11, 13, 20, 22, 23, 24, 43, 62, 90, electrophorese en gel de polyacrylamide-dodecylsuJfale de sodium 120, 204, and 205 kDa) were observed, with the major protein (SOS'PAGE) Q uotorze bandes proleiques au minimum ont ete at 25 kDa. Blood samples of 191 adult S. demersus were tes ted observees (9, 1 I, 13, 20, 22, 23, 24, 43, 62, 90, 120, 204, by enzyme-linked immunosorbent assoy (ELISA) utilizing B. peircei et 205 Wa), 10 proleine ma;eure elant de 25 Wo. -

Zoonotic Significance and Prophylactic Measure Against Babesiosis
Int.J.Curr.Microbiol.App.Sci (2015) 4(7): 938-953 International Journal of Current Microbiology and Applied Sciences ISSN: 2319-7706 Volume 4 Number 7 (2015) pp. 938-953 http://www.ijcmas.com Review Article Zoonotic significance and Prophylactic Measure against babesiosis Faryal Saad, Kalimullah Khan, Shandana Ali and Noor ul Akbar* Department of Zoology, Kohat University of Science and Technology, Kohat, Khyber Pakhtunkhwa, Pakistan *Corresponding author ABSTRACT Babesiosis is a vector borne disease by the different species of genus Babesia, affecting a large no of mammals worldwide. Babesiosis has zoonotic significance all over the world, causing huge loss to livestock industry and health hazards in human population. The primary zoonotic vector of babesia is ixodes ticks. Keywo rd s Different species have different virulence, infectivity and pathogenicity. Literature was collected from the individual researchers published papers. Table was made in Babesiosis , the MS excel. The present study review for the current knowledge about the Prophylactic, babesia species ecology, host specificity, life cycle and pathogenesis with an Tick borne, emphasis on the zoonotic significance and prophylactic measures against Vector, Babesiosis. Prophylactic measure against Babesiosis in early times was hindered Zoonosis. but due to advancement in research, the anti babesial drugs and vaccines have been developed. This review emphasizes on the awareness of public sector, rural communities, owners of animal husbandry and health department about the risk of infection in KPK and control measure should be implemented. Vaccines of less price tag should be designed to prevent the infection of cattles and human population. Introduction Babesiosis is a tick transmitted disease, At specie level there is considerable infecting a wide variety of wild and confusion about the true number of zoonotic domestic animals, as well as humans. -

Neglected Parasitic Infections in the United States Toxoplasmosis
Neglected Parasitic Infections in the United States Toxoplasmosis Toxoplasmosis is a preventable disease caused by the parasite Toxoplasma gondii. An infected individual can experience fever, malaise, and swollen lymph nodes, but can also show no signs or symptoms. A small number of infected persons may experience eye disease, and infection during pregnancy can lead to miscarriage or severe disease in the newborn, including developmental delays, blindness, and epilepsy. Once infected with T. gondii, people are generally infected for life. As a result, infected individuals with weakened immune systems—such as in the case of advanced HIV disease, during cancer treatment, or after organ transplant—can experience disease reactivation, which can result in severe illness or even death. In persons with advanced HIV disease, inflammation of the brain (encephalitis) due to toxoplasmosis is common unless long-term preventive medication is taken. Researchers have also found an association of T. gondii infection with the risk for mental illness, though this requires further study. Although T. gondii can infect most warm-blooded animals, cats are the only host that shed an environmentally resistant form of the organism (oocyst) in their feces. Once a person or another warm-blooded animal ingests the parasite, it becomes infectious and travels through the wall of the intestine. Then the parasite is carried by blood to other tissues including the muscles and central nervous system. Humans can be infected several ways, including: • Eating raw or undercooked meat containing the parasite in tissue cysts (usually pork, lamb, goat, or wild game meat, although beef and field-raised chickens have been implicated in studies). -

Anaplasmosis: an Emerging Tick-Borne Disease of Importance in Canada
IDCases 14 (2018) xxx–xxx Contents lists available at ScienceDirect IDCases journal homepage: www.elsevier.com/locate/idcr Case report Anaplasmosis: An emerging tick-borne disease of importance in Canada a, b,c d,e e,f Kelsey Uminski *, Kamran Kadkhoda , Brett L. Houston , Alison Lopez , g,h i c c Lauren J. MacKenzie , Robbin Lindsay , Andrew Walkty , John Embil , d,e Ryan Zarychanski a Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Internal Medicine, University of Manitoba, Winnipeg, MB, Canada b Cadham Provincial Laboratory, Government of Manitoba, Winnipeg, MB, Canada c Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Medical Microbiology and Infectious Diseases, University of Manitoba, Winnipeg, MB, Canada d Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Internal Medicine, Section of Medical Oncology and Hematology, University of Manitoba, Winnipeg, MB, Canada e CancerCare Manitoba, Department of Medical Oncology and Hematology, Winnipeg, MB, Canada f Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Pediatrics and Child Health, Section of Infectious Diseases, Winnipeg, MB, Canada g Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Internal Medicine, Section of Infectious Diseases, University of Manitoba, Winnipeg, MB, Canada h Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Community Health Sciences, University of Manitoba, Winnipeg, MB, Canada i Public Health Agency of Canada, National Microbiology Laboratory, Zoonotic Diseases and Special Pathogens, Winnipeg, MB, Canada A R T I C L E I N F O A B S T R A C T Article history: Human Granulocytic Anaplasmosis (HGA) is an infection caused by the intracellular bacterium Received 11 September 2018 Anaplasma phagocytophilum. -

Ehrlichiosis and Anaplasmosis Are Tick-Borne Diseases Caused by Obligate Anaplasmosis: Intracellular Bacteria in the Genera Ehrlichia and Anaplasma
Ehrlichiosis and Importance Ehrlichiosis and anaplasmosis are tick-borne diseases caused by obligate Anaplasmosis: intracellular bacteria in the genera Ehrlichia and Anaplasma. These organisms are widespread in nature; the reservoir hosts include numerous wild animals, as well as Zoonotic Species some domesticated species. For many years, Ehrlichia and Anaplasma species have been known to cause illness in pets and livestock. The consequences of exposure vary Canine Monocytic Ehrlichiosis, from asymptomatic infections to severe, potentially fatal illness. Some organisms Canine Hemorrhagic Fever, have also been recognized as human pathogens since the 1980s and 1990s. Tropical Canine Pancytopenia, Etiology Tracker Dog Disease, Ehrlichiosis and anaplasmosis are caused by members of the genera Ehrlichia Canine Tick Typhus, and Anaplasma, respectively. Both genera contain small, pleomorphic, Gram negative, Nairobi Bleeding Disorder, obligate intracellular organisms, and belong to the family Anaplasmataceae, order Canine Granulocytic Ehrlichiosis, Rickettsiales. They are classified as α-proteobacteria. A number of Ehrlichia and Canine Granulocytic Anaplasmosis, Anaplasma species affect animals. A limited number of these organisms have also Equine Granulocytic Ehrlichiosis, been identified in people. Equine Granulocytic Anaplasmosis, Recent changes in taxonomy can make the nomenclature of the Anaplasmataceae Tick-borne Fever, and their diseases somewhat confusing. At one time, ehrlichiosis was a group of Pasture Fever, diseases caused by organisms that mostly replicated in membrane-bound cytoplasmic Human Monocytic Ehrlichiosis, vacuoles of leukocytes, and belonged to the genus Ehrlichia, tribe Ehrlichieae and Human Granulocytic Anaplasmosis, family Rickettsiaceae. The names of the diseases were often based on the host Human Granulocytic Ehrlichiosis, species, together with type of leukocyte most often infected. -

A Comparative Genomic Study of Attenuated and Virulent Strains of Babesia Bigemina
pathogens Communication A Comparative Genomic Study of Attenuated and Virulent Strains of Babesia bigemina Bernardo Sachman-Ruiz 1 , Luis Lozano 2, José J. Lira 1, Grecia Martínez 1 , Carmen Rojas 1 , J. Antonio Álvarez 1 and Julio V. Figueroa 1,* 1 CENID-Salud Animal e Inocuidad, Instituto Nacional de Investigaciones Forestales Agrícolas y Pecuarias, Jiutepec, Morelos 62550, Mexico; [email protected] (B.S.-R.); [email protected] (J.J.L.); [email protected] (G.M.); [email protected] (C.R.); [email protected] (J.A.Á.) 2 Centro de Ciencias Genómicas, Universidad Nacional Autónoma de México, AP565-A Cuernavaca, Morelos 62210, Mexico; [email protected] * Correspondence: fi[email protected]; Tel.: +52-777-320-5544 Abstract: Cattle babesiosis is a socio-economically important tick-borne disease caused by Apicom- plexa protozoa of the genus Babesia that are obligate intraerythrocytic parasites. The pathogenicity of Babesia parasites for cattle is determined by the interaction with the host immune system and the presence of the parasite’s virulence genes. A Babesia bigemina strain that has been maintained under a microaerophilic stationary phase in in vitro culture conditions for several years in the laboratory lost virulence for the bovine host and the capacity for being transmitted by the tick vector. In this study, we compared the virulome of the in vitro culture attenuated Babesia bigemina strain (S) and the virulent tick transmitted parental Mexican B. bigemina strain (M). Preliminary results obtained by using the Basic Local Alignment Search Tool (BLAST) showed that out of 27 virulence genes described Citation: Sachman-Ruiz, B.; Lozano, and analyzed in the B. -

An Intestinal Gregarine of Nothria Conchylega (Polychaeta, Onuphidae)
Journal of Invertebrate Pathology 104 (2010) 172–179 Contents lists available at ScienceDirect Journal of Invertebrate Pathology journal homepage: www.elsevier.com/locate/jip Description of Trichotokara nothriae n. gen. et sp. (Apicomplexa, Lecudinidae) – An intestinal gregarine of Nothria conchylega (Polychaeta, Onuphidae) Sonja Rueckert *, Brian S. Leander Canadian Institute for Advanced Research, Program in Integrated Microbial Biodiversity, Departments of Botany and Zoology, University of British Columbia, #3529 – 6270 University Blvd., Vancouver, BC, Canada V6T 1Z4 article info abstract Article history: The trophozoites of a novel gregarine apicomplexan, Trichotokara nothriae n. gen. et sp., were isolated and Received 12 November 2009 characterized from the intestines of the onuphid tubeworm Nothria conchylega (Polychaeta), collected at Accepted 11 March 2010 20 m depth from the North-eastern Pacific Coast. The trophozoites were 50–155 lm long with a mid-cell Available online 23 March 2010 indentation that formed two prominent bulges (anterior bulge, 14–48 lm wide; posterior bulge, 15– 55 lm wide). Scanning electron microscopy (SEM) demonstrated that approximately 400 densely packed, Keywords: longitudinal epicytic folds (5 folds/lm) inscribe the surface of the trophozoites, and a prominently elon- Alveolata gated mucron (14–60 lm long and 6–12 lm wide) was covered with hair-like projections (mean length, Apicomplexa 1.97 m; mean width, 0.2 m at the base). Although a septum occurred at the junction between the cell Lecudinidae l l Lecudina proper and the mucron in most trophozoites, light microscopy (LM) demonstrated that the cell proper Parasite extended into the core of the mucron as a thin prolongation. -
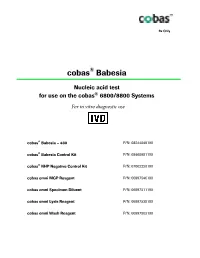
Package Insert
Rx Only ® cobas Babesia Nucleic acid test ® for use on the cobas 6800/8800 Systems For in vitro diagnostic use ® cobas Babesia – 480 P/N: 08244049190 cobas® Babesia Control Kit P/N: 08460981190 cobas® NHP Negative Control Kit P/N: 07002220190 cobas omni MGP Reagent P/N: 06997546190 cobas omni Specimen Diluent P/N: 06997511190 cobas omni Lysis Reagent P/N: 06997538190 cobas omni Wash Reagent P/N: 06997503190 cobas® Babesia Table of contents Intended use ............................................................................................................................ 4 Summary and explanation of the test ................................................................................. 4 Reagents and materials ......................................................................................................... 7 cobas® Babesia reagents and controls ....................................................................................................... 7 cobas omni reagents for sample preparation ........................................................................................ 10 Reagent storage and handling requirements ......................................................................................... 11 Additional materials required ................................................................................................................. 12 Instrumentation and software required ................................................................................................. 12 Precautions and handling requirements