Natural Medicine & Kidney Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PDI Appendix G Intermediate-Risk Immunocompromised State Ef Ec2
AHRQ QI™ ICD‐10‐CM/PCS Specification Enhanced Version 5.0 1 of 6 Pediatric Quality Indicators Appendices www.qualityindicators.ahrq.gov Pediatric Quality Indicators Appendices APPENDIX G: Intermediate-Risk Immunocompromised State Diagnosis Codes Intermediate-risk immunocompromised state diagnosis codes: (IMMUITD) ICD-9-CM Description ICD-10-CM Description 07022 VIRAL HEPATITIS B W HEPATIC COMA, CHRONIC WO B180 Chronic viral hepatitis B with delta‐agent MENTION OF HEPATITIS DELTA 07023 VIRAL HEPATITIS B W HEPACTIC COMA, CHRONIC W B181 Chronic viral hepatitis B without delta‐agent HEPATITIS DELTA 07044 CHRONIC HEPATITIS C WITH HEPACTIC COMMA B182 Chronic viral hepatitis C 2894 HYPERSPLENISM B520 Plasmodium malariae malaria with nephropathy 28950 DISEASE OF SPLEEN NOS D5702 Hb‐SS disease with splenic sequestration 28951 CHRONIC DIGESTIVE SPLENOMEGALY D57212 Sickle‐cell/Hb‐C disease with splenic sequestration 28952 SPLENIC SEQUESTRATION D57412 Sickle‐cell thalassemia with splenic sequestration 28959 OTHER DISEASE OF SPLEEN, OTHER D57812 Other sickle‐cell disorders with splenic sequestration 4560 ESOPHAGEAL VARICES W BLEEDING D730 Hyposplenism 4561 ESOPHAGEAL VARICES WO MENTION OF BLEEDING D731 Hypersplenism 45620 ESOPHAGEAL VARICES IN DISEASE CLASSIFIED D732 Chronic congestive splenomegaly ELSEWHERE, W BLEEDING 45621 ESOPHAGEAL VARICES IN DISEASE CLASSIFIED D733 Abscess of spleen ELSEWHERE, WO MENTION OF BLEEDING 5723 PORTAL HYPERTENSION D735 Infarction of spleen 5728 OTHER SEQUELAE OF CHRONIC LIVER DISEASE D7389 Other diseases of spleen 5735 -

Extrarenal Complications of the Nephrotic Syndrome
Kidney International, Vol. 33 (/988), pp. 1184—1202 NEPHROLOGY FORUM Extrarenal complications of the nephrotic syndrome Principal discussant: DAVID B. BERNARD The University Hospital and Boston University Sc/zoo!ofMedicine, Boston, Massachusetts present and equal. The temperature was 100°F. The blood pressure was 110/70 mm Hg in the right arm with the patient supine and standing. The Editors patient had no skin rashes, peteehiae, clubbing, or jaundice. Examina- JORDANJ. COHEN tion of the head and neck revealed intact cranial nerves and normal fundi. Ears, nose, and throat were normal. The jugular venous pressure Jot-IN T. HARRtNOTON was not increased. No lymph glands were palpable in the neck or JEROME P. KASSIRER axillae, and the trachea was midline, cardiac examination was normal. NICOLA05 E. MAmAs Examination of the lungs revealed coarse rales at the right base but no other abnormalities. Abdominal examination revealed aseites, but no Editor abdominal guarding, tenderness, or rigidity. The liver and spleen were Managing not palpable and no masses were present. The urine contained 4± CHERYL J. ZUSMAN protein; microscopic examination revealed free fat droplets, many oval fat bodies, and numerous fatty casts. Five to 10 red blood cells were seen per high-power field, but no red blood cell casts were present. A Universityof'Chicago Pritzker School of Medicine 24-hr urine collection contained 8 g of protein. The BUN was 22 mg/dl; creatinine, 2.0 mg/dl; and electrolytes were and normal. Serum total calcium was 7.8 mg/dl, and the phosphorus was 4.0 Taf is University School of' Medicine mg/dl. -

Path Renal Outline
Path Renal Outline Krane’s Categorization of Disease + A lot of Extras Kidney Disease Acute Renal Failure Intrinsic Kidney Disease Pre‐Renal Renal Intrinsic Post‐Renal Sodium Excretion <1% Glomerular Disease Tubulointerstitial Disease Sodium Excretion < 1% Sodium Excretion >2% Labs aren’t that useful BUN/Creatinine > 20 BUN/Creatinine < 10 CHF, Cirrhosis, Edema Urinalysis: Proteinuria + Hematuria Benign Proteinuria Spot Test Ratio >1.5, Spot Test Ratio <1.5, Acute Tubular Acute Interstitial Acute 24 Urine contains > 2.0g/24hrs 24 Urine contains < 1.0g/24hrs Necrosis Nephritis Glomerulonephritis Nephrotic Syndrome Nephritic Syndrome Inability to concentrate Urine RBC Casts Dirty Brown Casts Inability to secrete acid >3.5g protein / 24 hrs (huge proteinuria) Hematuria and Proteinuria (<3.5) Sodium Excretion >2% Edema Hypoalbuminemia RBC Casts Hypercholesterolemia Leukocytes Salt and Water Retention = HTN Focal Tubular Necrosis Edema Reduced GFR Pyelonephritis Minimal change disease Allergic Interstitial Nephritis Acute Proliferative Glomerulonephritis Membranous Glomerulopathy Analgesic Nephropathy Goodpasture’s (a form of RPGN) Focal segmental Glomerulosclerosis Rapidly Progressive Glomerulonephritis Multiple Myeloma Post‐Streptococcal Glomerulonephritis Membranoproliferative Glomerulonephritis IgA nephropathy (MPGN) Type 1 and Type 2 Alport’s Meleg‐Smith’s Hematuria Break Down Hematuria RBCs Only RBC + Crystals RBC + WBC RBC+ Protein Tumor Lithiasis (Stones) Infection Renal Syndrome Imaging Chemical Analysis Culture Renal Biopsy Calcium -

Management of the Nephrotic Syndrome GAVIN C
Arch Dis Child: first published as 10.1136/adc.43.228.257 on 1 April 1968. Downloaded from Personal Practice* Arch. Dis. Childh., 1968, 43, 257. Management of the Nephrotic Syndrome GAVIN C. ARNEIL From the Department of Child Health, University of Glasgow The nephrotic syndrome may be defined as gross (3) Idiopathic nephrosis. This may be re- proteinuria, predominantly albuminuria, with con- garded either as a primary disease, or as a secondary sequent selective hypoproteinaemia; usually accom- disorder, with the primary cause or causes still panied by oedema, ascites, and hyperlipaemia, and unknown. It is the common form of nephrosis in sometimes by systemic hypertension, azotaemia, or childhood, but the less common in adult patients. excessive erythrocyturia. Unless otherwise specified, the present discussion concerns idiopathic nephrosis. Grouping of Nephrotic Syndrome The syndrome falls into three groups. Assessment of the Case Full history and examination helps to exclude (1) Congenital nephrosis. A group of dis- many secondary forms of the disease. Blood orders present at and presenting soon after birth, pressure is recorded employing as broad a cuff as which are familial and may be acquired or inherited. practicable, and the width of the cuff used is Persistent oedema attracts attention in the first recorded as of importance in comparative estima- weeks of life. The disease may be rapidly lethal, tions. A careful search for concomitant infection but occasionally the patient will survive for a year is made, particularly to exclude pneumococcal copyright. or more without fatal infection or lethal azotaemia. peritonitis or low grade cellulitis. In a patient The disease pattern tends to run true within a previously treated elsewhere, evidence of steroid family. -

The Nephrotic Syndrome in Early Infancy: a Report of Three Cases* by H
Arch Dis Child: first published as 10.1136/adc.32.163.167 on 1 June 1957. Downloaded from THE NEPHROTIC SYNDROME IN EARLY INFANCY: A REPORT OF THREE CASES* BY H. McC. GILES, R. C. B. PUGH, E. M. DARMADY, FAY STRANACK and L. I. WOOLF From the Department of Paediatrics, St. Mary's Hospital, The Hospital for Sick Children, Great Ormond Street, London, and the Central Laboratory, Portsmouth (RECEIVED FOR PUBLICATION, DECEMBER 12, 1956) The nephrotic syndrome is characterized by evidence of genetic aetiology inasmuch as two of generalized oedema, hypoproteinaemia with diminu- the infants were brother and sister and both sets of tion or reversal of the albumin/globulin ratio, hyper- parents were cousins. Further points of interest lipaemia and gross albuminuria. Haematuria is not were the demonstration of anisotropic crystalline prominent; hypertension and azotaemia, except in material in alcohol-fixed tissues from all three the terminal stages, are slight and transient and infants, and the discovery on renal microdissection often do not occur at all. Recognition of this of lesions of the proximal tubule recalling those syndrome presents no difficulty but in many cases, found in Fanconi-Lignac disease (cystinosis). particularly in childhood, its cause remains obscure. Occasionally certain drugs such as troxidone or mercury, or certain diseases such as amyloidosis, Case Reports pyelonephritis, diabetes, disseminated lupus erythe- The parents of the first two patients (and the paternal copyright. matosus or renal vein thrombosis, can be in- grandparents) are first cousins. They, and a sister born criminated. In cases which develop renal failure three years before the first of her affected siblings, have and come to necropsy the lesions of glomerulo- been investigated in detail and show no sign of renal II disease. -

Acute Renal Failure Introduction • Incidence Can Range from 7% to 50
Acute Renal Failure Introduction Incidence can range from 7% to 50% of ICU patients Abrupt decline in kidney function (hours to weeks) Acute Kidney Injury Network Criteria (Bellomo R et al. Crit Care. 2004;8(4):R204-R212) Stage Serum Creatinine Criteria Urine Output 1 Cr inc by 1.5-2x or Cr inc by 0.3 mg/dL <0.5 mL/kg/hr for 6 h 2 Cr inc by 2-3x <0.5 mL/kg/hr for 12 h 3 Cr inc by more than 3x or Cr inc of 0.5 <0.3 mL/kg/hr for 24 hr (or anuria with baseline Cr >4 mg/dL for 12 h) Use criteria after fluid challenge in most cases Causes Pre-renal o Volume depletion o Cardiac o Redistribution o Hepatorenal syndrome . Cirrhosis with ascites . Serum creatinine > 1.5 mg/dL . Not improved by holding diuretics and giving albumin challenge (1g/kg for 2 days) . Absence of shock and nephrotoxins . No intrinsic renal disease i.e. no proteinuria (<500 mg/day) or microhematuria (< 50 RBCs) o NSAIDS o ACE-inhibitor Post-renal o Consider obstruction in every patient with ARF o Sites of obstruction . Bladder neck obstruction . Bilateral ureters o Urine volume is variable. Patients can be asymptomatic and with no change in urine output. o Diagnose with renal USG, straight catherization, or bladder scan Intrinsic o Vascular . Vascular occlusion . Atheroembolic disease Eosinophilia, low complement Can see multi-organ dysfunction, livedo reticularis, blue toes Generally irreversible . Thrombotic microangiopathy Fibrin deposition in the microvasculature, intravascular hemolysis, thrombocytopenia, organ dysfunction Associated disorders: Malignant HTN, HUS/TTP, Scleroderma renal crises, HELLP, drugs (tacrolimus, cyclosporine, mitomycin, Plavix) o Glomerular: RPGN . -

An Unusual Occurrence of Erythrocytosis in a Child with Nephrotic Syndrome and Advanced Chronic Kidney Disease
Case Report An Unusual Occurrence of Erythrocytosis in a Child with Nephrotic Syndrome and Advanced Chronic Kidney Disease Ratna Acharya 1 and Kiran Upadhyay 2,* 1 Division of General Pediatrics, Department of Pediatrics, University of Florida, Gainesville, FL 32610, USA; racharya@ufl.edu 2 Division of Pediatric Nephrology, Department of Pediatrics, University of Florida, Gainesville, FL 32610, USA * Correspondence: kupadhyay@ufl.edu; Tel.: +1-352-273-9180 Abstract: Background: Anemia is common in patients with nephrotic syndrome (NS) for various reasons. Furthermore, anemia can occur in patients with chronic kidney disease (CKD) predominantly owing to inappropriately low erythropoietin (EPO) production relative to the degree of anemia. However, erythrocytosis is uncommon in patients with NS and advanced CKD who are not treated with exogenous erythropoietin stimulating agents, and when present, will necessitate exploration of the other etiologies. Case summary: Here, we describe an 8-year-old girl with erythrocytosis in association with NS and advanced CKD. The patient was found to have erythrocytosis during the evaluation for hypertensive urgency. She also had nephrotic range proteinuria without edema. Serum hemoglobin and hematocrit were 17 gm/dL and 51%, respectively, despite hydration. Renal function test showed an estimated glomerular filtration rate of 30 mL/min/1.73 m2. There was mild iron deficiency anemia with serum iron saturation of 18%. Serum EPO level was normal. Urine EPO was not measured. Renal biopsy showed evidence of focal segmental glomerulosclerosis. Genetic testing for NS showed mutations in podocyte genes: NUP93, INF2, KANK1, and ACTN4. Gene Citation: Acharya, R.; Upadhyay, K. sequence analysis of genes associated with erythrocytosis showed no variants in any of these genes. -

Kidney Disease: the Basics
Kidney Disease: The Basics Note: Footnotes in body text may not run sequentially due to ongoing updates. However, they do correspond correctly to the numbers in the reference list. Fast Facts Kidney disease, also known as chronic kidney disease or CKD, causes more deaths than breast cancer or prostate cancer (NVS 2021 report of 2018 data).1 It is the under-recognized public health crisis. • Kidney disease affects an estimated 37 million people in the U.S. (15% of the adult population; more than 1 in 7 adults).2,3,4 • Approximately 90% of those with kidney disease don’t know they have it.2 • And 2 of 5 adults with severe kidney disease don’t know they have it.2 • 1 in 3 adults in the U.S. (approximately 80 million) is at risk for kidney disease.2,5 • Kidney disease is more common in women (14%) than men (12%).2 But for every 2 women who develop end- stage kidney disease (ESKD), 3 men’s kidneys fail.2 • Kidney disease is a leading cause of death in the U.S.1,6,7 • About 1 in 2 people with very low kidney function (not on dialysis) don’t know they have kidney disease.2,13 • Approximately 1 in 3 adults with diabetes and 1 in 5 adults with high blood pressure may have kidney disease.2 • COVID-19 is targeting people with kidney disease, kidney transplant patients, and those at risk for kidney disease. [See www.kidney.org/covid-19] What is Kidney Disease? Chronic kidney disease (CKD) means your kidneys are damaged and losing their ability to keep you healthy by filtering your blood. -
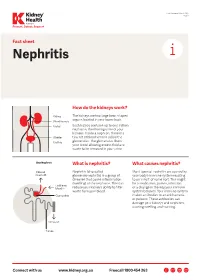
Nephritis Fact Sheet
Last Reviewed March 2017 Page 1 Prevent, Detect, Support. Fact sheet Nephritis How do the kidneys work? The kidneys are two large bean-shaped organs located in your lower back. Each kidney contains up to one million nephrons, the filtering units of your kidneys. Inside a nephron, there is a tiny set of blood vessels called the glomerulus. The glomerulus filters your blood allowing excess fluid and waste to be removed in your urine. What is nephritis? What causes nephritis? Nephritis (also called Most types of nephritis are caused by glomerulonephritis) is a group of your body’s immune system reacting diseases that cause inflammation to an ‘insult’ of some sort. This might (swelling) of the nephrons. This can be a medication, poison, infection reduce your kidney’s ability to filter or a change in the way your immune waste from your blood. system behaves. Your immune system makes antibodies to attack bacteria or poisons. These antibodies can damage your kidneys and nephrons, causing swelling and scarring. Connect with us www.kidney.org.au Freecall 1800 454 363 Kidney Health Australia Nephritis Last Reviewed March 2017 Prevent, Detect, Support. Page 2 What are the different types of nephritis? There are many different types of Different types of nephritis include: Nephrotic syndrome: Damage to the nephritis. It can vary from a mild, nephrons causes them to leak large Focal nephritis: Less than a half of non-damaging condition to a serious amounts of protein into your urine your nephrons have scarring, and problem causing kidney failure. Some but little blood. Losing this protein blood and a small amount of protein types of nephritis appear mild at means your body does not have are found in your urine. -

Nephrotic Syndrome What You Should Know
Nephrotic Syndrome what you should know WHAT IS NEPHROTIC SYNDROME? • Tiny filtering units (glomeruli) in the kidney are damaged or not working. • Protein normally kept in your body, leaks into the urine. Signs and symptoms include: Many diseases can cause it: • High urine protein (proteinuria) • Minimal change disease (MCD) • Swelling (edema) around the eyes, • Membranous glomerulonephritis face, feet, ankles, and/or belly • Focal segmental glomerulosclerosis (FSGS) • Weight gain (from fluid retention) • IGA nephropathy • Foamy urine • Lupus • Poor appetite • Diabetes • High blood cholesterol • Certain infections such as Hepatitis B and C, HIV, others HOW IS IT TESTED? HOW IS IT TREATED? • Physical exam: • Depending on the disease and person’s Visible signs and symptoms overall health, dietary changes and medicines are used to: • Blood and urine tests: - Lower excess salt and fluids in the body Signs of kidney damage and - Lower loss of protein in the urine other diseases - Lower cholesterol in the blood • Imaging tests and/or • Certain medicines that suppress or “calm” kidney biopsy: the immune system can be used. Signs of kidney disease • Sometimes, the dose might need to be • Genetic tests: changed, or a different medicine might Inherited diseases that are be used. linked with kidney disease • In some cases, nephrotic syndrome can lead to kidney failure, which is treated with dialysis or a kidney transplant. Nephrotic Syndrome what you should know HOW CAN I REDUCE MY RISK? Diet, Exercise, and Lifestyle Changes Medicines • Follow a healthy diet that is low in salt • Before taking any over-the-counter and cholesterol. medicine or supplement, ask your healthcare provider which is safe. -
Unique Proximal Tubular Cell Injury and the Development of Acute
Fujigaki et al. BMC Nephrology (2017) 18:339 DOI 10.1186/s12882-017-0756-6 RESEARCH ARTICLE Open Access Unique proximal tubular cell injury and the development of acute kidney injury in adult patients with minimal change nephrotic syndrome Yoshihide Fujigaki1*, Yoshifuru Tamura2, Michito Nagura2, Shigeyuki Arai2, Tatsuru Ota2, Shigeru Shibata2, Fukuo Kondo3, Yutaka Yamaguchi3 and Shunya Uchida2 Abstract Background: Adult patients with minimal change nephrotic syndrome (MCNS) are often associated with acute kidney injury (AKI). To assess the mechanisms of AKI, we examined whether tubular cell injuries unique to MCNS patients exist. Methods: We performed a retrospective analysis of clinical data and tubular cell changes using the immunohistochemical expression of vimentin as a marker of tubular injury and dedifferentiation at kidney biopsy in 37 adult MCNS patients. AKI was defined by the criteria of the Kidney Disease: Improving Global Outcomes (KDIGO) Clinical Practice Guidelines for AKI. Results: Thirteen patients (35.1%) were designated with AKI at kidney biopsy. No significant differences in age, history of hypertension, chronic kidney disease, diuretics use, proteinuria, and serum albumin were noted between the AKI and non- AKI groups. Urinary N-acetyl-β-D-glucosaminidase (uNAG) and urinary alpha1-microglobulin (uA1MG) as markers of tubular injury were increased in both groups, but the levels were significantly increased in the AKI group compared with the non- AKI group. The incidence of vimentin-positive tubules was comparable between AKI (84.6%) and non-AKI (58.3%) groups, but vimentin-positive tubular area per interstitial area was significantly increased in the AKI group (19.8%) compared with the non-AKI group (6.8%) (p = 0.011). -

Chronic Kidney Disease in South Carolina
Chronic Kidney Disease in South Carolina WHAT IS KIDNEY DISEASE1? KIDNEY DISEASE IN S.C. • Chronic Kidney Disease (CKD) reduces the body’s ability Mortality to filter blood, remove waste and extra water, and keep beneficial electrolytes in balance. • 868 people died from Kidney Disease in 2013 (most recent data available). The mortality rate decreased from • Left untreated, CKD can lead to kidney failure. 19.8 in 2010 to 16.0 in 2013 but still remains above the • When this happens, dialysis or a kidney transplant is the national rate. only option for keeping a person alive. • Deaths from Nephritis, Nephrotic Syndrome, and • Early kidney disease is a silent problem! Nephrosis are the 8th leading cause of death. U.S. STATISTICS • More than 20 million Americans have chronic kidney disease1. • Many more Americans, including anyone with high blood pressure, diabetes, or a family history of kidney disease, are at an increased risk2. • The number of people developing kidney failure has doubled each decade for the last two decades3. • End-Stage Renal Disease (ESRD) resulted in 88,638 deaths in 20124. • Treating Medicare patients aged 65 or older with kidney • Mortality from Kidney Disease for blacks in South disease cost the United States $44.6 billion in 20125. Carolina is more than twice as high as whites. • 47,112 people died from Nephritis, Nephrotic Syndrome, and Nephrosis in 2013 (14.9 per 100,000 population). This was the 9th leading cause of death6. WHO IS AT RISK1? • Diabetes is the most common cause of kidney failure. Approximately 1 out of 3 adults with diabetes has CKD.