Acute Renal Failure Introduction • Incidence Can Range from 7% to 50
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PDI Appendix G Intermediate-Risk Immunocompromised State Ef Ec2
AHRQ QI™ ICD‐10‐CM/PCS Specification Enhanced Version 5.0 1 of 6 Pediatric Quality Indicators Appendices www.qualityindicators.ahrq.gov Pediatric Quality Indicators Appendices APPENDIX G: Intermediate-Risk Immunocompromised State Diagnosis Codes Intermediate-risk immunocompromised state diagnosis codes: (IMMUITD) ICD-9-CM Description ICD-10-CM Description 07022 VIRAL HEPATITIS B W HEPATIC COMA, CHRONIC WO B180 Chronic viral hepatitis B with delta‐agent MENTION OF HEPATITIS DELTA 07023 VIRAL HEPATITIS B W HEPACTIC COMA, CHRONIC W B181 Chronic viral hepatitis B without delta‐agent HEPATITIS DELTA 07044 CHRONIC HEPATITIS C WITH HEPACTIC COMMA B182 Chronic viral hepatitis C 2894 HYPERSPLENISM B520 Plasmodium malariae malaria with nephropathy 28950 DISEASE OF SPLEEN NOS D5702 Hb‐SS disease with splenic sequestration 28951 CHRONIC DIGESTIVE SPLENOMEGALY D57212 Sickle‐cell/Hb‐C disease with splenic sequestration 28952 SPLENIC SEQUESTRATION D57412 Sickle‐cell thalassemia with splenic sequestration 28959 OTHER DISEASE OF SPLEEN, OTHER D57812 Other sickle‐cell disorders with splenic sequestration 4560 ESOPHAGEAL VARICES W BLEEDING D730 Hyposplenism 4561 ESOPHAGEAL VARICES WO MENTION OF BLEEDING D731 Hypersplenism 45620 ESOPHAGEAL VARICES IN DISEASE CLASSIFIED D732 Chronic congestive splenomegaly ELSEWHERE, W BLEEDING 45621 ESOPHAGEAL VARICES IN DISEASE CLASSIFIED D733 Abscess of spleen ELSEWHERE, WO MENTION OF BLEEDING 5723 PORTAL HYPERTENSION D735 Infarction of spleen 5728 OTHER SEQUELAE OF CHRONIC LIVER DISEASE D7389 Other diseases of spleen 5735 -

Extrarenal Complications of the Nephrotic Syndrome
Kidney International, Vol. 33 (/988), pp. 1184—1202 NEPHROLOGY FORUM Extrarenal complications of the nephrotic syndrome Principal discussant: DAVID B. BERNARD The University Hospital and Boston University Sc/zoo!ofMedicine, Boston, Massachusetts present and equal. The temperature was 100°F. The blood pressure was 110/70 mm Hg in the right arm with the patient supine and standing. The Editors patient had no skin rashes, peteehiae, clubbing, or jaundice. Examina- JORDANJ. COHEN tion of the head and neck revealed intact cranial nerves and normal fundi. Ears, nose, and throat were normal. The jugular venous pressure Jot-IN T. HARRtNOTON was not increased. No lymph glands were palpable in the neck or JEROME P. KASSIRER axillae, and the trachea was midline, cardiac examination was normal. NICOLA05 E. MAmAs Examination of the lungs revealed coarse rales at the right base but no other abnormalities. Abdominal examination revealed aseites, but no Editor abdominal guarding, tenderness, or rigidity. The liver and spleen were Managing not palpable and no masses were present. The urine contained 4± CHERYL J. ZUSMAN protein; microscopic examination revealed free fat droplets, many oval fat bodies, and numerous fatty casts. Five to 10 red blood cells were seen per high-power field, but no red blood cell casts were present. A Universityof'Chicago Pritzker School of Medicine 24-hr urine collection contained 8 g of protein. The BUN was 22 mg/dl; creatinine, 2.0 mg/dl; and electrolytes were and normal. Serum total calcium was 7.8 mg/dl, and the phosphorus was 4.0 Taf is University School of' Medicine mg/dl. -

An Unusual Occurrence of Erythrocytosis in a Child with Nephrotic Syndrome and Advanced Chronic Kidney Disease
Case Report An Unusual Occurrence of Erythrocytosis in a Child with Nephrotic Syndrome and Advanced Chronic Kidney Disease Ratna Acharya 1 and Kiran Upadhyay 2,* 1 Division of General Pediatrics, Department of Pediatrics, University of Florida, Gainesville, FL 32610, USA; racharya@ufl.edu 2 Division of Pediatric Nephrology, Department of Pediatrics, University of Florida, Gainesville, FL 32610, USA * Correspondence: kupadhyay@ufl.edu; Tel.: +1-352-273-9180 Abstract: Background: Anemia is common in patients with nephrotic syndrome (NS) for various reasons. Furthermore, anemia can occur in patients with chronic kidney disease (CKD) predominantly owing to inappropriately low erythropoietin (EPO) production relative to the degree of anemia. However, erythrocytosis is uncommon in patients with NS and advanced CKD who are not treated with exogenous erythropoietin stimulating agents, and when present, will necessitate exploration of the other etiologies. Case summary: Here, we describe an 8-year-old girl with erythrocytosis in association with NS and advanced CKD. The patient was found to have erythrocytosis during the evaluation for hypertensive urgency. She also had nephrotic range proteinuria without edema. Serum hemoglobin and hematocrit were 17 gm/dL and 51%, respectively, despite hydration. Renal function test showed an estimated glomerular filtration rate of 30 mL/min/1.73 m2. There was mild iron deficiency anemia with serum iron saturation of 18%. Serum EPO level was normal. Urine EPO was not measured. Renal biopsy showed evidence of focal segmental glomerulosclerosis. Genetic testing for NS showed mutations in podocyte genes: NUP93, INF2, KANK1, and ACTN4. Gene Citation: Acharya, R.; Upadhyay, K. sequence analysis of genes associated with erythrocytosis showed no variants in any of these genes. -
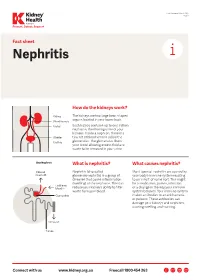
Nephritis Fact Sheet
Last Reviewed March 2017 Page 1 Prevent, Detect, Support. Fact sheet Nephritis How do the kidneys work? The kidneys are two large bean-shaped organs located in your lower back. Each kidney contains up to one million nephrons, the filtering units of your kidneys. Inside a nephron, there is a tiny set of blood vessels called the glomerulus. The glomerulus filters your blood allowing excess fluid and waste to be removed in your urine. What is nephritis? What causes nephritis? Nephritis (also called Most types of nephritis are caused by glomerulonephritis) is a group of your body’s immune system reacting diseases that cause inflammation to an ‘insult’ of some sort. This might (swelling) of the nephrons. This can be a medication, poison, infection reduce your kidney’s ability to filter or a change in the way your immune waste from your blood. system behaves. Your immune system makes antibodies to attack bacteria or poisons. These antibodies can damage your kidneys and nephrons, causing swelling and scarring. Connect with us www.kidney.org.au Freecall 1800 454 363 Kidney Health Australia Nephritis Last Reviewed March 2017 Prevent, Detect, Support. Page 2 What are the different types of nephritis? There are many different types of Different types of nephritis include: Nephrotic syndrome: Damage to the nephritis. It can vary from a mild, nephrons causes them to leak large Focal nephritis: Less than a half of non-damaging condition to a serious amounts of protein into your urine your nephrons have scarring, and problem causing kidney failure. Some but little blood. Losing this protein blood and a small amount of protein types of nephritis appear mild at means your body does not have are found in your urine. -

Nephrotic Syndrome What You Should Know
Nephrotic Syndrome what you should know WHAT IS NEPHROTIC SYNDROME? • Tiny filtering units (glomeruli) in the kidney are damaged or not working. • Protein normally kept in your body, leaks into the urine. Signs and symptoms include: Many diseases can cause it: • High urine protein (proteinuria) • Minimal change disease (MCD) • Swelling (edema) around the eyes, • Membranous glomerulonephritis face, feet, ankles, and/or belly • Focal segmental glomerulosclerosis (FSGS) • Weight gain (from fluid retention) • IGA nephropathy • Foamy urine • Lupus • Poor appetite • Diabetes • High blood cholesterol • Certain infections such as Hepatitis B and C, HIV, others HOW IS IT TESTED? HOW IS IT TREATED? • Physical exam: • Depending on the disease and person’s Visible signs and symptoms overall health, dietary changes and medicines are used to: • Blood and urine tests: - Lower excess salt and fluids in the body Signs of kidney damage and - Lower loss of protein in the urine other diseases - Lower cholesterol in the blood • Imaging tests and/or • Certain medicines that suppress or “calm” kidney biopsy: the immune system can be used. Signs of kidney disease • Sometimes, the dose might need to be • Genetic tests: changed, or a different medicine might Inherited diseases that are be used. linked with kidney disease • In some cases, nephrotic syndrome can lead to kidney failure, which is treated with dialysis or a kidney transplant. Nephrotic Syndrome what you should know HOW CAN I REDUCE MY RISK? Diet, Exercise, and Lifestyle Changes Medicines • Follow a healthy diet that is low in salt • Before taking any over-the-counter and cholesterol. medicine or supplement, ask your healthcare provider which is safe. -
Unique Proximal Tubular Cell Injury and the Development of Acute
Fujigaki et al. BMC Nephrology (2017) 18:339 DOI 10.1186/s12882-017-0756-6 RESEARCH ARTICLE Open Access Unique proximal tubular cell injury and the development of acute kidney injury in adult patients with minimal change nephrotic syndrome Yoshihide Fujigaki1*, Yoshifuru Tamura2, Michito Nagura2, Shigeyuki Arai2, Tatsuru Ota2, Shigeru Shibata2, Fukuo Kondo3, Yutaka Yamaguchi3 and Shunya Uchida2 Abstract Background: Adult patients with minimal change nephrotic syndrome (MCNS) are often associated with acute kidney injury (AKI). To assess the mechanisms of AKI, we examined whether tubular cell injuries unique to MCNS patients exist. Methods: We performed a retrospective analysis of clinical data and tubular cell changes using the immunohistochemical expression of vimentin as a marker of tubular injury and dedifferentiation at kidney biopsy in 37 adult MCNS patients. AKI was defined by the criteria of the Kidney Disease: Improving Global Outcomes (KDIGO) Clinical Practice Guidelines for AKI. Results: Thirteen patients (35.1%) were designated with AKI at kidney biopsy. No significant differences in age, history of hypertension, chronic kidney disease, diuretics use, proteinuria, and serum albumin were noted between the AKI and non- AKI groups. Urinary N-acetyl-β-D-glucosaminidase (uNAG) and urinary alpha1-microglobulin (uA1MG) as markers of tubular injury were increased in both groups, but the levels were significantly increased in the AKI group compared with the non- AKI group. The incidence of vimentin-positive tubules was comparable between AKI (84.6%) and non-AKI (58.3%) groups, but vimentin-positive tubular area per interstitial area was significantly increased in the AKI group (19.8%) compared with the non-AKI group (6.8%) (p = 0.011). -

A Clinical and Pathological Study of Schistosomal Nephritis*
Bull. Org. mond. Sante 1972, 47, 549-557 Bull. Wld Hlth Org. A clinical and pathological study of schistosomal nephritis* M. S. SABBOUR,1 W. EL-SAID,' & I. ABOU-GABAL3 In a Cairo clinic 17 of41patients with chronicpyelonephritis secondary to urinary schisto- somiasis presented with classicalfeatures of the nephrotic syndrome, two-thirds being hyper- tensive and the majority having glomerular filtration rates within the normal range. Hyper- cholesterolaemia was found in one-third of the patients. Urinary sediments from these patients contained a preponderance of pus cells, red cells, granular casts, or pus casts. In addition to patches ofpyelonephritis, the glomeruli showed diffuse andfocal glomerulo- sclerosis. Electron microscopy revealed basement-membrane-like deposits in the hypertro- phied axial endothelial cells and electron-dense deposits along the glomerular basement membrane. This variety of nephrotic syndrome associated with schistosomal pyelonephritis was the most common cause of nephrotic syndrome seen in the clinic. During the last few years, we have had the impres- urine analysis. A modified Addis technique (El-Said, sion that patients with urinary schistosomiasis and 1971) was used to count the exact number of pus secondary bacterial pyelonephritis develop a neph- cells excreted per hour in urine. rotic syndrome. The majority of patients admitted Only confirmed cases of chronic pyelonephritis to the renal unit are suffering from chronic pyelo- were included in this study, doubtful cases being nephritis secondary to urinary schistosomiasis (Abou- excluded. Patients with, in addition to the pyelo- Gabal et al., 1970), and a considerable proportion nephritis, other lesions that could give rise to the of them have varying degrees of generalized oedema. -

Proteinuria and Nephrotic Syndrome
Proteinuria and Nephrotic Syndrome Rebecca Hjorten, MD Division of Nephrology Speaker Disclosures • Relevant Financial Relationships: No disclosure. • Relevant Nonfinancial Relationships: No disclosure. • I have no actual or potential conflict of interest in relation to this program/presentation. Division of NephrologyDivision of Nephrology Urine Dip Concern for Positive for Urine Positive for Glomerulonephritis Protein Protein AND Blood (GN) …PIGN, MPGN, IgA, HSP Lupus, ANCA vasculitis, Urine Positive for Anti-GBM Asymptomatic Protein AND NORMAL Concerning Ex. Nephrotic Syndrome False Positive Symptoms Non-Significant Levels Persistent of Urine Protein Asymptomatic Consider Proteinuria Further Orthostatic Proteinuria Evaluation and Referral to Transient Proteinuria Pediatric Nephrology Division of Nephrology Urine Dip Concern for Positive for Urine Positive for Glomerulonephritis Protein Protein AND Blood (GN) …PIGN, MPGN, IgA, HSP Lupus, ANCA vasculitis, Urine Positive for Anti-GBM Asymptomatic Protein AND NORMAL Concerning Ex. Nephrotic Syndrome False Positive Symptoms Non-Significant Levels Persistent of Urine Protein Asymptomatic Consider Proteinuria Further Orthostatic Proteinuria Evaluation and Referral to Transient Proteinuria Pediatric Nephrology Division of Nephrology Objectives • Asymptomatic Proteinuria without Hematuria • Identification of transient and orthostatic proteinuria • Initial workup and referral or persistent proteinuria • Nephrotic syndrome • Early recognition of nephrotic syndrome • Initiation of management • -

Albumin and Furosemide Combination for Management of Edema in Nephrotic Syndrome: a Review of Clinical Studies
Cells 2015, 4, 622-630; doi:10.3390/cells4040622 OPEN ACCESS cells ISSN 2073-4409 www.mdpi.com/journal/cells Review Albumin and Furosemide Combination for Management of Edema in Nephrotic Syndrome: A Review of Clinical Studies Margaret Duffy, Shashank Jain, Nicholas Harrell, Neil Kothari and Alluru S. Reddi * Department of Medicine, Rutgers New Jersey Medical School, 185 South Orange Avenue, Newark, NJ 07103, USA; E-Mails: [email protected] (M.D.); [email protected] (S.J.); [email protected] (N.H.); [email protected] (N.K.) * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: 973-972-6072. Academic Editor: Christoph Englert Received: 7 August 2015 / Accepted: 30 September 2015 / Published: 7 October 2015 Abstract: The treatment of edema in patients with nephrotic syndrome is generally managed by dietary sodium restriction and loop diuretics. However, edema does not improve in some patients despite adequate sodium restriction and maximal dose of diuretics. In such patients, combination of albumin and a loop diuretic may improve edema by diuresis and natriuresis. The response to this combination of albumin and a diuretic has not been observed in all studies. The purpose of this review is to discuss the physiology of diuresis and natriuresis of this combination therapy, and provide a brief summary of various studies that have used albumin and a loop diuretic to improve diuretic-resistant edema. Also, the review suggests various reasons for not observing similar results by various investigators. Keywords: nephrotic syndrome; albumin and diuretic; diuresis; natriuresis; edema management 1. Introduction Edema is a common clinical symptom in patients with nephrotic syndrome. -

Nephrotic Nephritic Syndrome (1)
[1] LECTURES THREE AND FOUR PATHOLOGY OF THE NEPHROTIC, NEPHRITIC AND CHRONIC KIDNEY DISEASE BY DR. AMMAR AL RIKABI, PROFESSOR M.O. ALSOHAIBANI AND DR. HALA KFOURY DEPARTMENT OF PATHOLOGY KING KHALID UNIVERSITY HOSPITAL - Important points Contents: è Female Notes è Male Notes - Explanation - Evaluation of glomerular disease (Terminology & Techniques). - Glomerular Diseases: Nephro'c Syndrome: Nephri'c Syndrome: Other Glomerular Diseases: 1| Minimal Change Disease. 1| Posstreptococcal 1| IgA nephropathy. 2| Focal Segmental Glomerulonephris. Golmerulosclerosis 2| MembranoproliFerave 3| Membranous 2| Rapidly Progressive Glomerulonephris. Gomerulonephris . Glomerulonephris. 4| Diabe'c Nephropathy. 5| Renal Amyloidosis. 3| Good Pasture Syndrome. 6| Lupus Nephropathy. - Renal Failure. - Azotemia. 2 EVALUATION OF GLOMERULAR DISEASE (c) Generalized edema results from decreased plasma colloid or oncotic pressure. (without Red 1] Terminology: The following terms are used to Blood Cells nor White Blood Cells in the urine) describe the extent of glomerular injury: (d) Hyperlipidemia and hyperchomsterolemia are caused by increased hepatic lipoprotein • Diffuse, all glomeruli are affected synthesis. • Focal, some glomeruli are affected. • Segmental, part of one glomerulus is affected. Why does this occur? Global, the entirety of one glomerulus is affected. • Due to the fusion of the foot processes (podocytes) leading to an increase in the permeability of the basement membrane. This 2] Techniques used for studying of leads to protein leakage Ex: albumin. glomerular diseases: 1. Light microscopy: using routine (haematoxylin and eosin) and special stains. M inimal change disease - MCD 2. Immunofluorescence: antibodies tagged (lipoid nephrosis) is seen most often in young (labelled) with a fluorchrome are used to children but can also occur in older children and localize immunoreactants in the glomerulus. -

A Study to Assess the Prevalence of Hypertension in Children with Nephrotic Syndrome
International Journal of Contemporary Pediatrics Manasa M et al. Int J Contemp Pediatr. 2019 Nov;6(6):2340-2345 http://www.ijpediatrics.com pISSN 2349-3283 | eISSN 2349-3291 DOI: http://dx.doi.org/10.18203 /2349-3291.ijcp20194184 Original Research Article A study to assess the prevalence of hypertension in children with nephrotic syndrome Manasa M.1, Anitha S. Prabhu1*, Santhosh Pai2, Kiran Raj H.3 1Department of Pediatrics, 2Department of Nephrology, Yenapoya Medical College Hospital, Mangalore, Karnataka, India 3Department of Pediatrics, Srinivas Institute of Medical Science and Research Centre, Mukka, Mangalore, Karnataka, India Received: 23 August 2019 Revised: 31 August 2019 Accepted: 04 September 2019 *Correspondence: Dr. Anitha S. Prabhu, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Background: Hypertension is been one of the most common co morbidity of this disease. It was mostly attributed to sodium retention, which is a major clinical feature of nephrotic syndrome. These mechanisms likely have a role in the development of hypertension in nephrotic syndrome, where hypertension may be difficult to control, and provide new therapeutic options for the management of blood pressure in the setting of nephrotic syndrome. Objective of study the prevalence of hypertension in children with NS and also the number of antihypertensive required to control it. Method: A Retrospective study of the hospital records of 100 children diagnosed with nephrotic syndrome admitted to Pediatric and Nephrology Ward at YMCH was accessed. -

Approach to Persistent Microscopic Hematuria in Children
Review Article Approach to Persistent Microscopic Hematuria in Children Mahmoud Kallash1 and Michelle N. Rheault 2 Abstract Persistent isolated microscopic hematuria is relatively common in pediatric practice, affecting around 0.25% of children. Isolated microscopic hematuria can be caused by a myriad of potentially benign or serious causes, including urologic issues; kidney stones; glomerular diseases, including disorders of the glomerular basement membrane; hematologic abnormalities; and others. The challenge for the pediatrician or pediatric nephrologist is to distinguish children with potentially progressive forms of kidney disease versus other causes while minimizing cost and inconvenience for the child and family. This manuscript will review the multiple potential causes of microscopic hematuria and provide a framework for the initial evaluation and monitoring of such patients. KIDNEY360 1: 1014–1020, 2020. doi: https://doi.org/10.34067/KID.0003222020 Introduction longer than 6 months identified normal findings in Microscopic hematuria is common in children, and it is 44%, thin GBMs in 22%, Alport syndrome in 12%, and present in 4.1% of school age children (1). Microscopic IgA nephropathy (IgAN) in 11% (4). In contrast, a sim- hematuria that persists on repeated evaluations is less ilar study in China demonstrated normal findings in common, with only 0.25% of children having blood 71%, thin GBMs in 3.2%, Alport syndrome in 1.4%, and in four consecutive urinalyses (UAs) (1). Of children IgAN in 16%, suggesting that practice and referral with microscopic hematuria, only 16.2% of them also patterns or race/ethnicity may influence findings (5). had proteinuria; thus, the majority of children identi- The challenge for the pediatrician or pediatric nephrol- fied with hematuria have isolated hematuria (1).