Pathway-Focused Gene Interaction Analysis Reveals the Regulation Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Building Bonds Between NHGRI and NICHD • NICHD Has Four ABMGG Boarded Clinical Geneticists • Drs
Building Bonds Between NHGRI NICHD Diana W. Bianchi, M.D. Director, NICHD November 8, 2017 A Vision for NICHD’s Future What’s In a Name? NICHD 18% Other Institutes 82% Eunice Kennedy Shriver National Institute of Child Health and Human Development History of Our Mission ". We will look to the National Institute of Child Health and Human Development for a concentrated attack on the unsolved health problems of children and of mother-infant relationships. This legislation will encourage imaginative research into the complex processes of human development from conception to old age. For the first time, we will have an institute to promote studies directed at the entire life process rather than toward specific diseases or illnesses." —John F. Kennedy, October 17, 1962 My Vision for NICHD-I • Define “our brand” (what is our focus?) • Communicate the message • Listen to the Voice of the Patient • Integrate obstetrics and pediatrics research at NICHD; take the long view (DoHaD) • Advocate for personalized medicine in pediatrics, obstetrics and rehabilitative medicine My Vision for NICHD-II • Stress the importance of data science and sharing to leverage our investments • Analyze best way to identify trainees most likely to succeed • Catalyze innovation • Emphasize the “A” (for “Advice”) in the Advisory Council • Build bridges between other NIH Institutes – especially with NHGRI Ensure Representation of NICHD Populations in Trans-NIH Initiatives • Pregnant women can be enrolled in Phase I • Adults with intellectual disabilities can be enrolled once consent issues have been clarified • Children to be enrolled in Phase II Building Bonds Melissa Parisi MD PhD Medical Genetics Branch: Prenatal Genomics and Therapy Section • New Lab at NHGRI • Focus on Prenatal Treatment of Down syndrome • Incidental Findings Following Prenatal DNA Screening Building Bonds Between NHGRI and NICHD • NICHD has four ABMGG boarded clinical geneticists • Drs. -
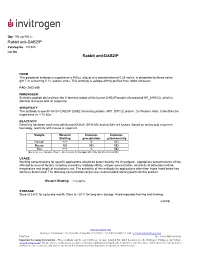
Rabbit Anti-DAB2IP Rabbit Anti-DAB2IP
Qty: 100 μg/400 μL Rabbit anti-DAB2IP Catalog No. 487300 Lot No. Rabbit anti-DAB2IP FORM This polyclonal antibody is supplied as a 400 µL aliquot at a concentration of 0.25 mg/mL in phosphate buffered saline (pH 7.4) containing 0.1% sodium azide. This antibody is epitope-affinity purified from rabbit antiserum. PAD: ZMD.689 IMMUNOGEN Synthetic peptide derived from the C-terminal region of the human DAB2IP protein (Accession# NP_619723), which is identical to mouse and rat sequence. SPECIFICITY This antibody is specific for the DAB2IP (DAB2 interacting protein, AIP1, DIP1/2) protein. On Western blots, it identifies the target band at ~110 kDa. REACTIVITY Reactivity has been confirmed with human DU145, SK-N-MC and rat B49 cell lysates. Based on amino acid sequence homology, reactivity with mouse is expected. Sample Western Immuno- Immuno- Blotting precipitation cytochemistry Human +++ 0 ND Mouse ND ND ND Rat +++ 0 ND (Excellent +++, Good++, Poor +, No reactivity 0, Not applicable N/A, Not Determined ND) USAGE Working concentrations for specific applications should be determined by the investigator. Appropriate concentrations will be affected by several factors, including secondary antibody affinity, antigen concentration, sensitivity of detection method, temperature and length of incubations, etc. The suitability of this antibody for applications other than those listed below has not been determined. The following concentration ranges are recommended starting points for this product. Western Blotting: 1-3 μg/mL STORAGE Store at 2-8°C for up to one month. Store at –20°C for long-term storage. Avoid repeated freezing and thawing. (cont’d) www.invitrogen.com Invitrogen Corporation • 542 Flynn Rd • Camarillo • CA 93012 • Tel: 800.955.6288 • E-mail: [email protected] PI487300 (Rev 10/08) DCC-08-1089 Important Licensing Information - These products may be covered by one or more Limited Use Label Licenses (see the Invitrogen Catalog or our website, www.invitrogen.com). -

Identification and Characterization of RHOA-Interacting Proteins in Bovine Spermatozoa1
BIOLOGY OF REPRODUCTION 78, 184–192 (2008) Published online before print 10 October 2007. DOI 10.1095/biolreprod.107.062943 Identification and Characterization of RHOA-Interacting Proteins in Bovine Spermatozoa1 Sarah E. Fiedler, Malini Bajpai, and Daniel W. Carr2 Department of Medicine, Oregon Health & Sciences University and Veterans Affairs Medical Center, Portland, Oregon 97239 ABSTRACT Guanine nucleotide exchange factors (GEFs) catalyze the GDP for GTP exchange [2]. Activation is negatively regulated by In somatic cells, RHOA mediates actin dynamics through a both guanine nucleotide dissociation inhibitors (RHO GDIs) GNA13-mediated signaling cascade involving RHO kinase and GTPase-activating proteins (GAPs) [1, 2]. Endogenous (ROCK), LIM kinase (LIMK), and cofilin. RHOA can be RHO can be inactivated via C3 exoenzyme ADP-ribosylation, negatively regulated by protein kinase A (PRKA), and it and studies have demonstrated RHO involvement in actin-based interacts with members of the A-kinase anchoring (AKAP) cytoskeletal response to extracellular signals, including lyso- family via intermediary proteins. In spermatozoa, actin poly- merization precedes the acrosome reaction, which is necessary phosphatidic acid (LPA) [2–4]. LPA is known to signal through for normal fertility. The present study was undertaken to G-protein-coupled receptors (GPCRs) [4, 5]; specifically, LPA- determine whether the GNA13-mediated RHOA signaling activated GNA13 (formerly Ga13) promotes RHO activation pathway may be involved in acrosome reaction in bovine through GEFs [4, 6]. Activated RHO-GTP then signals RHO caudal sperm, and whether AKAPs may be involved in its kinase (ROCK), resulting in the phosphorylation and activation targeting and regulation. GNA13, RHOA, ROCK2, LIMK2, and of LIM-kinase (LIMK), which in turn phosphorylates and cofilin were all detected by Western blot in bovine caudal inactivates cofilin, an actin depolymerizer, the end result being sperm. -

Genetic and Genomic Analysis of Hyperlipidemia, Obesity and Diabetes Using (C57BL/6J × TALLYHO/Jngj) F2 Mice
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Nutrition Publications and Other Works Nutrition 12-19-2010 Genetic and genomic analysis of hyperlipidemia, obesity and diabetes using (C57BL/6J × TALLYHO/JngJ) F2 mice Taryn P. Stewart Marshall University Hyoung Y. Kim University of Tennessee - Knoxville, [email protected] Arnold M. Saxton University of Tennessee - Knoxville, [email protected] Jung H. Kim Marshall University Follow this and additional works at: https://trace.tennessee.edu/utk_nutrpubs Part of the Animal Sciences Commons, and the Nutrition Commons Recommended Citation BMC Genomics 2010, 11:713 doi:10.1186/1471-2164-11-713 This Article is brought to you for free and open access by the Nutrition at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Nutrition Publications and Other Works by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. Stewart et al. BMC Genomics 2010, 11:713 http://www.biomedcentral.com/1471-2164/11/713 RESEARCH ARTICLE Open Access Genetic and genomic analysis of hyperlipidemia, obesity and diabetes using (C57BL/6J × TALLYHO/JngJ) F2 mice Taryn P Stewart1, Hyoung Yon Kim2, Arnold M Saxton3, Jung Han Kim1* Abstract Background: Type 2 diabetes (T2D) is the most common form of diabetes in humans and is closely associated with dyslipidemia and obesity that magnifies the mortality and morbidity related to T2D. The genetic contribution to human T2D and related metabolic disorders is evident, and mostly follows polygenic inheritance. The TALLYHO/ JngJ (TH) mice are a polygenic model for T2D characterized by obesity, hyperinsulinemia, impaired glucose uptake and tolerance, hyperlipidemia, and hyperglycemia. -

Supplementary Table 1: Adhesion Genes Data Set
Supplementary Table 1: Adhesion genes data set PROBE Entrez Gene ID Celera Gene ID Gene_Symbol Gene_Name 160832 1 hCG201364.3 A1BG alpha-1-B glycoprotein 223658 1 hCG201364.3 A1BG alpha-1-B glycoprotein 212988 102 hCG40040.3 ADAM10 ADAM metallopeptidase domain 10 133411 4185 hCG28232.2 ADAM11 ADAM metallopeptidase domain 11 110695 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 195222 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 165344 8751 hCG20021.3 ADAM15 ADAM metallopeptidase domain 15 (metargidin) 189065 6868 null ADAM17 ADAM metallopeptidase domain 17 (tumor necrosis factor, alpha, converting enzyme) 108119 8728 hCG15398.4 ADAM19 ADAM metallopeptidase domain 19 (meltrin beta) 117763 8748 hCG20675.3 ADAM20 ADAM metallopeptidase domain 20 126448 8747 hCG1785634.2 ADAM21 ADAM metallopeptidase domain 21 208981 8747 hCG1785634.2|hCG2042897 ADAM21 ADAM metallopeptidase domain 21 180903 53616 hCG17212.4 ADAM22 ADAM metallopeptidase domain 22 177272 8745 hCG1811623.1 ADAM23 ADAM metallopeptidase domain 23 102384 10863 hCG1818505.1 ADAM28 ADAM metallopeptidase domain 28 119968 11086 hCG1786734.2 ADAM29 ADAM metallopeptidase domain 29 205542 11085 hCG1997196.1 ADAM30 ADAM metallopeptidase domain 30 148417 80332 hCG39255.4 ADAM33 ADAM metallopeptidase domain 33 140492 8756 hCG1789002.2 ADAM7 ADAM metallopeptidase domain 7 122603 101 hCG1816947.1 ADAM8 ADAM metallopeptidase domain 8 183965 8754 hCG1996391 ADAM9 ADAM metallopeptidase domain 9 (meltrin gamma) 129974 27299 hCG15447.3 ADAMDEC1 ADAM-like, -

S41467-020-18249-3.Pdf
ARTICLE https://doi.org/10.1038/s41467-020-18249-3 OPEN Pharmacologically reversible zonation-dependent endothelial cell transcriptomic changes with neurodegenerative disease associations in the aged brain Lei Zhao1,2,17, Zhongqi Li 1,2,17, Joaquim S. L. Vong2,3,17, Xinyi Chen1,2, Hei-Ming Lai1,2,4,5,6, Leo Y. C. Yan1,2, Junzhe Huang1,2, Samuel K. H. Sy1,2,7, Xiaoyu Tian 8, Yu Huang 8, Ho Yin Edwin Chan5,9, Hon-Cheong So6,8, ✉ ✉ Wai-Lung Ng 10, Yamei Tang11, Wei-Jye Lin12,13, Vincent C. T. Mok1,5,6,14,15 &HoKo 1,2,4,5,6,8,14,16 1234567890():,; The molecular signatures of cells in the brain have been revealed in unprecedented detail, yet the ageing-associated genome-wide expression changes that may contribute to neurovas- cular dysfunction in neurodegenerative diseases remain elusive. Here, we report zonation- dependent transcriptomic changes in aged mouse brain endothelial cells (ECs), which pro- minently implicate altered immune/cytokine signaling in ECs of all vascular segments, and functional changes impacting the blood–brain barrier (BBB) and glucose/energy metabolism especially in capillary ECs (capECs). An overrepresentation of Alzheimer disease (AD) GWAS genes is evident among the human orthologs of the differentially expressed genes of aged capECs, while comparative analysis revealed a subset of concordantly downregulated, functionally important genes in human AD brains. Treatment with exenatide, a glucagon-like peptide-1 receptor agonist, strongly reverses aged mouse brain EC transcriptomic changes and BBB leakage, with associated attenuation of microglial priming. We thus revealed tran- scriptomic alterations underlying brain EC ageing that are complex yet pharmacologically reversible. -

Quantitative Proteomics Identify DAB2 As a Cardiac Developmental Regulator That Inhibits WNT/Β-Catenin Signaling
Quantitative proteomics identify DAB2 as a cardiac developmental regulator that inhibits WNT/β-catenin signaling Peter Hofsteena,b,c,1, Aaron M. Robitaillec,d,1, Daniel Patrick Chapmana,b, Randall T. Moonc,d,e,2, and Charles E. Murrya,b,c,f,g,2 aDepartment of Pathology, University of Washington, Seattle, WA 98109; bCenter for Cardiovascular Biology, University of Washington, Seattle, WA 98109; cInstitute for Stem Cell and Regenerative Medicine, University of Washington, Seattle, WA 98109; dDepartment of Pharmacology, University of Washington, Seattle, WA 98109; eHoward Hughes Medical Institute, Chevy Chase, MD 20815; fDepartment of Bioengineering, University of Washington, Seattle, WA 98109; and gDivision of Cardiology, Department of Medicine, University of Washington, Seattle, WA 98109 Contributed by Randall T. Moon, December 11, 2015 (sent for review September 19, 2015; reviewed by Loren J. Field and Sean P. Palecek) To reveal the molecular mechanisms involved in cardiac lineage endocardial-like endothelial cells to differentiate toward the cardiac determination and differentiation, we quantified the proteome of lineage (3). Thus, understanding which proteins are involved in pro- human embryonic stem cells (hESCs), cardiac progenitor cells (CPCs), moting or repressing the WNT/β-catenin signaling pathway is crucial and cardiomyocytes during a time course of directed differentiation for resolving the ambiguities associated with cardiac development. by label-free quantitative proteomics. This approach correctly iden- Here, using label-free quantitation (LFQ) proteomics, we tified known stage-specific markers of cardiomyocyte differentiation, measured protein expression patterns during a time course of including SRY-box2 (SOX2), GATA binding protein 4 (GATA4), and hESC-derived cardiomyocyte differentiation. LFQ proteomics is myosin heavy chain 6 (MYH6). -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

A Novel Resveratrol Analog: Its Cell Cycle Inhibitory, Pro-Apoptotic and Anti-Inflammatory Activities on Human Tumor Cells
A NOVEL RESVERATROL ANALOG : ITS CELL CYCLE INHIBITORY, PRO-APOPTOTIC AND ANTI-INFLAMMATORY ACTIVITIES ON HUMAN TUMOR CELLS A dissertation submitted to Kent State University in partial fulfillment of the requirements for the degree of Doctor of Philosophy by Boren Lin May 2006 Dissertation written by Boren Lin B.S., Tunghai University, 1996 M.S., Kent State University, 2003 Ph. D., Kent State University, 2006 Approved by Dr. Chun-che Tsai , Chair, Doctoral Dissertation Committee Dr. Bryan R. G. Williams , Co-chair, Doctoral Dissertation Committee Dr. Johnnie W. Baker , Members, Doctoral Dissertation Committee Dr. James L. Blank , Dr. Bansidhar Datta , Dr. Gail C. Fraizer , Accepted by Dr. Robert V. Dorman , Director, School of Biomedical Sciences Dr. John R. Stalvey , Dean, College of Arts and Sciences ii TABLE OF CONTENTS LIST OF FIGURES……………………………………………………………….………v LIST OF TABLES……………………………………………………………………….vii ACKNOWLEDGEMENTS….………………………………………………………….viii I INTRODUCTION….………………………………………………….1 Background and Significance……………………………………………………..1 Specific Aims………………………………………………………………………12 II MATERIALS AND METHODS.…………………………………………….16 Cell Culture and Compounds…….……………….…………………………….….16 MTT Cell Viability Assay………………………………………………………….16 Trypan Blue Exclusive Assay……………………………………………………...18 Flow Cytometry for Cell Cycle Analysis……………..……………....……………19 DNA Fragmentation Assay……………………………………………...…………23 Caspase-3 Activity Assay………………………………...……….….…….………24 Annexin V-FITC Staining Assay…………………………………..…...….………28 NF-kappa B p65 Activity Assay……………………………………..………….…29 -

Frequent Loss of Heterozygosity Targeting the Inactive X Chromosome in Melanoma
6476 Vol. 9, 6476–6482, December 15, 2003 Clinical Cancer Research Frequent Loss of Heterozygosity Targeting the Inactive X Chromosome in Melanoma James O. Indsto,1 Najah T. Nassif,2 INTRODUCTION Richard F. Kefford,1 and Graham J. Mann1 Chromosomal deletions and amplification events are fre- 1Westmead Institute for Cancer Research, University of Sydney at quent in advanced neoplasms and provide evidence for the Westmead Millennium Institute, Westmead, New South Wales, existence and location of putative tumor suppressor genes Australia, and 2Department of Cell and Molecular Biology, University (TSGs) and oncogenes. In melanoma, 9p and 10q deletions are of Technology, Sydney, New South Wales, Australia most frequent, and losses on 6q, 11q, 1p, 15p, 17q, and 18q are also frequently found (1, 2). However, no studies have focused on the X chromosome. In the human female, random inactiva- ABSTRACT tion of one copy of an X chromosome by hypermethylation is an After previous preliminary observations of paradoxical early event in embryogenesis, resulting in most tissues being a deletion events affecting the inactive X chromosome in mel- mosaic in terms of X inactivation status. Neoplasms, being anoma, we have surveyed the X chromosome for deletions clonal expansions of single precursor cells, usually share a using 23 polymorphic microsatellite markers in 28 inform- common X inactivation status. This can be conveniently assayed ative (female XX) metastatic melanomas. Ten tumors (36%) using the methylation-sensitive restriction enzyme HpaII, which showed at least one loss of heterozygosity (LOH) event, and has a recognition site within the highly polymorphic exon 1 in two cases an entire chromosome showed LOH at all CAG repeat (ARTR) in the androgen receptor (AR) gene. -

Transcriptome Analysis of Human Diabetic Kidney Disease
ORIGINAL ARTICLE Transcriptome Analysis of Human Diabetic Kidney Disease Karolina I. Woroniecka,1 Ae Seo Deok Park,1 Davoud Mohtat,2 David B. Thomas,3 James M. Pullman,4 and Katalin Susztak1,5 OBJECTIVE—Diabetic kidney disease (DKD) is the single cases, mild and then moderate mesangial expansion can be leading cause of kidney failure in the U.S., for which a cure has observed. In general, diabetic kidney disease (DKD) is not yet been found. The aim of our study was to provide an considered a nonimmune-mediated degenerative disease unbiased catalog of gene-expression changes in human diabetic of the glomerulus; however, it has long been noted that kidney biopsy samples. complement and immunoglobulins sometimes can be de- — tected in diseased glomeruli, although their role and sig- RESEARCH DESIGN AND METHODS Affymetrix expression fi arrays were used to identify differentially regulated transcripts in ni cance is not clear (4). 44 microdissected human kidney samples. The DKD samples were The understanding of DKD has been challenged by multi- significant for their racial diversity and decreased glomerular ple issues. First, the diagnosis of DKD usually is made using filtration rate (~20–30 mL/min). Stringent statistical analysis, using clinical criteria, and kidney biopsy often is not performed. the Benjamini-Hochberg corrected two-tailed t test, was used to According to current clinical practice, the development of identify differentially expressed transcripts in control and diseased albuminuria in patients with diabetes is sufficient to make the glomeruli and tubuli. Two different Web-based algorithms were fi diagnosis of DKD (5). We do not understand the correlation used to de ne differentially regulated pathways. -

Network-Based Genetic Profiling, and Therapeutic Target Identification Of
bioRxiv preprint doi: https://doi.org/10.1101/480632; this version posted November 29, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Network-based genetic profiling, and therapeutic target identification of Thyroid Cancer 1st Md. Ali Hossain 2nd Tania Akter Asa 3rd Julian Quinn 4rdMd. Mijanur Rahman Dept. of CSE Dept. of EEE Bone biology divisions Dept. of CSE MIU, Jahangirnagar University Islamic University Garvan Institute of Medical Research JKKNIU Dhaka, Bangladesh Kushtia, Bangladesh Sydney, Australia Bangladesh ali:cse:bd@gmail:com tania:eee:iu@gmail:com j:quinn@garvan:org:au mijan cse@yahoo:com 5th Fazlul Huq 6th Mohammad Ali Moni Biomedical Sciences, Faculty of Medicine and Health Biomedical Sciences, Faculty of Medicine and Health The University of Sydney The University of Sydney Sydney, Australia Sydney, Australia fazlul:huq@sydney:edu:au mohammad:moni@sydney:edu:au Abstract—Molecular mechanisms that underlie the pathogene- I. INTRODUCTION sis and progression of malignant thyroid cancer (TC) are poorly understood. In this study, we employed network-based integrative Thyroid cancer (TC) is the most common endocrine ma- analyses of TC lesions to identify key molecules that are possible lignant disease [24], and although it has a relatively low hub genes and proteins in molecular pathways active in TC. We thus studied a microarray gene expression dataset (GSE82208, mortality rate compared to most other common metastatic n=52) that compared TC to benign thyroid tumours (follicular diseases its incidence is rising and is now the fifth most thyroid adenomas) in order to identify differentially expressed common cancer disease in women, notably affecting those genes (DEGs) in TC.