A Novel Resveratrol Analog: Its Cell Cycle Inhibitory, Pro-Apoptotic and Anti-Inflammatory Activities on Human Tumor Cells
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Microdeletions in 16P11.2 and 13Q31.3 Associated with Developmental Delay and Generalized Overgrowth
Microdeletions in 16p11.2 and 13q31.3 associated with developmental delay and generalized overgrowth A.M. George1, J. Taylor2 and D.R. Love1 1Diagnostic Genetics, LabPlus, Auckland City Hospital, Auckland, New Zealand 2Northern Regional Genetic Service, Auckland City Hospital, Auckland, New Zealand Corresponding author: D.R. Love E-mail: [email protected] Genet. Mol. Res. 11 (3): 3133-3137 (2012) Received November 28, 2011 Accepted July 18, 2012 Published September 3, 2012 DOI http://dx.doi.org/10.4238/2012.September.3.1 ABSTRACT. Chromosome microarray analysis of patients with developmental delay has provided evidence of small deletions or duplications associated with this clinical phenotype. In this context, a 7.1- to 8.7-Mb interstitial deletion of chromosome 16 is well documented, but within this interval a rare 200-kb deletion has recently been defined that appears to be associated with obesity, or developmental delay together with overgrowth. We report a patient carrying this rare deletion, who falls into the latter clinical category, but who also carries a second very rare deletion in 13q31.3. It remains unclear if this maternally inherited deletion acts as a second copy number variation leading to pathogenic variation, or is non-causal and the true modifiers are yet to be determined. Key words: Developmental delay; Obesity; Overgrowth; GPC5; SH2B1 Genetics and Molecular Research 11 (3): 3133-3137 (2012) ©FUNPEC-RP www.funpecrp.com.br A.M. George et al. 3134 INTRODUCTION Current referrals for chromosome microarray analysis (CMA) are primarily for de- termining the molecular basis of developmental delay and autistic spectrum disorder in child- hood. -

Wo 2010/075007 A2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 1 July 2010 (01.07.2010) WO 2010/075007 A2 (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C12Q 1/68 (2006.01) G06F 19/00 (2006.01) kind of national protection available): AE, AG, AL, AM, C12N 15/12 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) International Application Number: DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/US2009/067757 HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (22) International Filing Date: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, 11 December 2009 ( 11.12.2009) ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (25) Filing Language: English SE, SG, SK, SL, SM, ST, SV, SY, TJ, TM, TN, TR, TT, (26) Publication Language: English TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 12/3 16,877 16 December 2008 (16.12.2008) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, ZM, (71) Applicant (for all designated States except US): DODDS, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, W., Jean [US/US]; 938 Stanford Street, Santa Monica, TM), European (AT, BE, BG, CH, CY, CZ, DE, DK, EE, CA 90403 (US). -

Genome-Wide Analysis of DNA Methylation Differences in Muscle and Fat from Monozygotic Twins Discordant for Type 2 Diabetes
Genome-Wide Analysis of DNA Methylation Differences in Muscle and Fat from Monozygotic Twins Discordant for Type 2 Diabetes Rasmus Ribel-Madsen1,2*, Mario F. Fraga3, Stine Jacobsen1, Jette Bork-Jensen1, Ester Lara4, Vincenzo Calvanese4, Agustin F. Fernandez5, Martin Friedrichsen1, Birgitte F. Vind6, Kurt Højlund6, Henning Beck-Nielsen6, Manel Esteller7, Allan Vaag1,8, Pernille Poulsen9 1 Steno Diabetes Center, Gentofte, Denmark, 2 Section of Metabolic Genetics, The Novo Nordisk Foundation Center for Basic Metabolic Research, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark, 3 Department of Immunology and Oncology, National Centre for Biotechnology, CNB-CSIC, Madrid, Spain, 4 Department of Cancer Epigenetics, Spanish National Cancer Research Centre, Madrid, Spain, 5 Cancer Epigenetics Laboratory, Instituto Universitario de Oncologia del Principado de Asturias, HUCA, Universidad de Oviedo, Oviedo, Spain, 6 Department of Endocrinology, Odense University Hospital, Odense, Denmark, 7 Cancer Epigenetics and Biology Program (PEBC), Bellvitge Biomedical Research Institute (IDIBELL), L’Hospitalet de Llobregat, Barcelona, Spain, 8 Department of Endocrinology, Rigshospitalet, Copenhagen, Denmark, 9 Novo Nordisk A/S, Søborg, Denmark Abstract Background: Monozygotic twins discordant for type 2 diabetes constitute an ideal model to study environmental contributions to type 2 diabetic traits. We aimed to examine whether global DNA methylation differences exist in major glucose metabolic tissues from these twins. Methodology/Principal Findings: Skeletal muscle (n = 11 pairs) and subcutaneous adipose tissue (n = 5 pairs) biopsies were collected from 53–80 year-old monozygotic twin pairs discordant for type 2 diabetes. DNA methylation was measured by microarrays at 26,850 cytosine-guanine dinucleotide (CpG) sites in the promoters of 14,279 genes. -

Universidade Estadual De Campinas Instituto De Biologia
UNIVERSIDADE ESTADUAL DE CAMPINAS INSTITUTO DE BIOLOGIA VERÔNICA APARECIDA MONTEIRO SAIA CEREDA O PROTEOMA DO CORPO CALOSO DA ESQUIZOFRENIA THE PROTEOME OF THE CORPUS CALLOSUM IN SCHIZOPHRENIA CAMPINAS 2016 1 VERÔNICA APARECIDA MONTEIRO SAIA CEREDA O PROTEOMA DO CORPO CALOSO DA ESQUIZOFRENIA THE PROTEOME OF THE CORPUS CALLOSUM IN SCHIZOPHRENIA Dissertação apresentada ao Instituto de Biologia da Universidade Estadual de Campinas como parte dos requisitos exigidos para a obtenção do Título de Mestra em Biologia Funcional e Molecular na área de concentração de Bioquímica. Dissertation presented to the Institute of Biology of the University of Campinas in partial fulfillment of the requirements for the degree of Master in Functional and Molecular Biology, in the area of Biochemistry. ESTE ARQUIVO DIGITAL CORRESPONDE À VERSÃO FINAL DA DISSERTAÇÃO DEFENDIDA PELA ALUNA VERÔNICA APARECIDA MONTEIRO SAIA CEREDA E ORIENTADA PELO DANIEL MARTINS-DE-SOUZA. Orientador: Daniel Martins-de-Souza CAMPINAS 2016 2 Agência(s) de fomento e nº(s) de processo(s): CNPq, 151787/2F2014-0 Ficha catalográfica Universidade Estadual de Campinas Biblioteca do Instituto de Biologia Mara Janaina de Oliveira - CRB 8/6972 Saia-Cereda, Verônica Aparecida Monteiro, 1988- Sa21p O proteoma do corpo caloso da esquizofrenia / Verônica Aparecida Monteiro Saia Cereda. – Campinas, SP : [s.n.], 2016. Orientador: Daniel Martins de Souza. Dissertação (mestrado) – Universidade Estadual de Campinas, Instituto de Biologia. 1. Esquizofrenia. 2. Espectrometria de massas. 3. Corpo caloso. -

AN INVESTIGATION of the ROLE of PAK6 in TUMORIGENESIS By
AN INVESTIGATION OF THE ROLE OF PAK6 IN TUMORIGENESIS by JoAnn Roberts A Thesis Submitted to the Faculty of The Charles E. Schmidt College of Medicine In Partial Fulfillment of the Requirements for the Degree of Master of Science Florida Atlantic University Boca Raton, Florida August 2012 ACKNOWLEDGMENTS This material is based upon work supported by the National Science Foundation under Grant No. DGE: 0638662. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the author(s) and do not necessarily reflect the views of the National Science Foundation. I would like to thank and acknowledge my thesis advisor, Dr. Michael Lu, for his support and guidance throughout the writing of this thesis and design of experiments in this manuscript. I would also like to thank my colleagues for assistance in various trouble-shooting circumstances. Last, but certainly not least, I would like to thank my family and friends for their support in the pursuit of my graduate studies. iii ABSTRACT Author: JoAnn Roberts Title: An Investigation of the Role of PAK6 in Tumorigenesis Institution: Florida Atlantic University Thesis Advisor: Dr. Michael Lu Degree: Master of Science Year: 2012 The function and role of PAK6, a serine/threonine kinase, in cancer progression has not yet been clearly identified. Several studies reveal that PAK6 may participate in key changes contributing to cancer progression such as cell survival, cell motility, and invasiveness. Based on the membrane localization of PAK6 in prostate and breast cancer cells, we speculated that PAK6 plays a role in cancer progression cells by localizing on the membrane and modifying proteins linked to motility and proliferation. -

Src-Dependent DBL Family Members Drive Resistance to Vemurafenib in Human Melanoma Charlotte R
Published OnlineFirst August 15, 2019; DOI: 10.1158/0008-5472.CAN-19-0244 Cancer Translational Science Research Src-Dependent DBL Family Members Drive Resistance to Vemurafenib in Human Melanoma Charlotte R. Feddersen1, Jacob L. Schillo1, Afshin Varzavand2, Hayley R. Vaughn1, Lexy S. Wadsworth1, Andrew P. Voigt1, Eliot Y. Zhu1, Brooke M. Jennings2, Sarah A. Mullen2, Jeremy Bobera2, Jesse D. Riordan1, Christopher S. Stipp2,3, and Adam J. Dupuy1,3 Abstract The use of selective BRAF inhibitors (BRAFi) has pro- signaling axis capable of driving resistance to both current duced remarkable outcomes for patients with advanced and next-generation BRAFis. However, we show that the cutaneous melanoma harboring a BRAFV600E mutation. SRC inhibitor, saracatinib, canblocktheDBL-drivenresis- Unfortunately, the majority of patients eventually develop tance. Our work highlights the utility of our straightforward drug-resistant disease. We employed a genetic screening genetic screening method in identifying new drug combina- approach to identify gain-of-function mechanisms of BRAFi tions to combat acquired BRAFi resistance. resistance in two independent melanoma cell lines. Our screens identified both known and unappreciated drivers of Significance: A simple, rapid, and flexible genetic screen- BRAFi resistance, including multiple members of the DBL ing approach identifies genes that drive resistance to MAPK family. Mechanistic studies identified a DBL/RAC1/PAK inhibitors when overexpressed in human melanoma cells. Introduction characterized (7). Thus, unexplained cases of resistance to MAPK inhibition (MAPKi) in human melanoma represent an important Melanoma is the deadliest form of skin cancer, with around unmet clinical need. 90,000 diagnoses of invasive disease and approximately 10,000 Mechanisms of vemurafenib resistance have been studied in deaths per year (1). -

Autism Multiplex Family with 16P11.2P12.2 Microduplication Syndrome in Monozygotic Twins and Distal 16P11.2 Deletion in Their Brother
European Journal of Human Genetics (2012) 20, 540–546 & 2012 Macmillan Publishers Limited All rights reserved 1018-4813/12 www.nature.com/ejhg ARTICLE Autism multiplex family with 16p11.2p12.2 microduplication syndrome in monozygotic twins and distal 16p11.2 deletion in their brother Anne-Claude Tabet1,2,3,4, Marion Pilorge2,3,4, Richard Delorme5,6,Fre´de´rique Amsellem5,6, Jean-Marc Pinard7, Marion Leboyer6,8,9, Alain Verloes10, Brigitte Benzacken1,11,12 and Catalina Betancur*,2,3,4 The pericentromeric region of chromosome 16p is rich in segmental duplications that predispose to rearrangements through non-allelic homologous recombination. Several recurrent copy number variations have been described recently in chromosome 16p. 16p11.2 rearrangements (29.5–30.1 Mb) are associated with autism, intellectual disability (ID) and other neurodevelopmental disorders. Another recognizable but less common microdeletion syndrome in 16p11.2p12.2 (21.4 to 28.5–30.1 Mb) has been described in six individuals with ID, whereas apparently reciprocal duplications, studied by standard cytogenetic and fluorescence in situ hybridization techniques, have been reported in three patients with autism spectrum disorders. Here, we report a multiplex family with three boys affected with autism, including two monozygotic twins carrying a de novo 16p11.2p12.2 duplication of 8.95 Mb (21.28–30.23 Mb) characterized by single-nucleotide polymorphism array, encompassing both the 16p11.2 and 16p11.2p12.2 regions. The twins exhibited autism, severe ID, and dysmorphic features, including a triangular face, deep-set eyes, large and prominent nasal bridge, and tall, slender build. The eldest brother presented with autism, mild ID, early-onset obesity and normal craniofacial features, and carried a smaller, overlapping 16p11.2 microdeletion of 847 kb (28.40–29.25 Mb), inherited from his apparently healthy father. -

Chromosomal Assignment of the Genes for Human Aldehyde Dehydrogenase-1 and Aldehyde Dehydrogenase-2 LILY C
Am J Hum Genet 38:641-648, 1986 Chromosomal Assignment of the Genes for Human Aldehyde Dehydrogenase-1 and Aldehyde Dehydrogenase-2 LILY C. Hsu,', AKIRA YOSHIDA,' AND T. MOHANDAS2 SUMMARY Chromosomal assignment of the genes for two major human aldehyde dehydrogenase isozymes, that is, cytosolic aldehyde dehydrogenase-1 (ALDH1) and mitochondrial aldehyde dehydrogenase-2 (ALDH2) were determined. Genomic DNA, isolated from a panel of mouse- human and Chinese hamster-human hybrid cell lines, was digested by restriction endonucleases and subjected to Southern blot hybridiza- tion using cDNA probes for ALDH1 and for ALDH2. Based on the distribution pattern of ALDH1 and ALDH2 in cell hybrids, ALDHI was assigned to the long arm of human chromosome 9 and ALDH2 to chromosome 12. INTRODUCTION Two major and at least two minor aldehyde dehydrogenase isozymes exist in human and other mammalian livers. One of the major isozymes, designated as ALDH 1, or E1, is of cytosolic origin, and another major isozyme, designated as ALDH2 or E2, is of mitochondrial origin. The two isozymes are different from each other with respect to their kinetic properties, sensitivity to disulfiram inactivation, and protein structure [1-5]. Remarkable racial differences be- tween Caucasians and Orientals have been found in these isozymes. Approxi- mately 50% of Orientals have a variant form of ALDH2 associated with dimin- ished activity, while virtually all Caucasians have the wild-type active ALDH2 Received July 10, 1985; revised September 23, 1985. This work was supported by grant AA05763 from the National Institutes of Health. ' Department of Biochemical Genetics, Beckman Research Institute of the City of Hope, Duarte, CA 91010. -

The Characterization of Human Adenylate Kinases 7 and 8
The characterization of human adenylate kinases 7 and 8 demonstrates differences in kinetic parameters and structural organization among the family of adenylate kinase isoenzymes Christakis Panayiotou, Nicola Solaroli, Yunjian Xu, Magnus Johansson, Anna Karlsson To cite this version: Christakis Panayiotou, Nicola Solaroli, Yunjian Xu, Magnus Johansson, Anna Karlsson. The char- acterization of human adenylate kinases 7 and 8 demonstrates differences in kinetic parameters and structural organization among the family of adenylate kinase isoenzymes. Biochemical Journal, Port- land Press, 2011, 433 (3), pp.527-534. 10.1042/BJ20101443. hal-00558097 HAL Id: hal-00558097 https://hal.archives-ouvertes.fr/hal-00558097 Submitted on 21 Jan 2011 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Biochemical Journal Immediate Publication. Published on 16 Nov 2010 as manuscript BJ20101443 The characterization of human adenylate kinases 7 and 8 demonstrates differences in kinetic parameters and structural organization among the family of adenylate kinase isoenzymes -

Molecular Docking Investigation of the Amantadine Binding to the Enzymes Upregulated Or Downregulated in Parkinson's Disease
ADMET & DMPK 8(2) (2020) 149-175; doi: http://dx.doi.org/10.5599/admet.854 Open Access : ISSN : 1848-7718 http://www.pub.iapchem.org/ojs/index.php/admet/index Original scientific paper Molecular docking investigation of the amantadine binding to the enzymes upregulated or downregulated in Parkinson’s disease 1,2 Mihaela Ileana Ionescu 1Department of Microbiology, Iuliu Hațieganu University of Medicine and Pharmacy, 6 Louis Pasteur, 400349, Cluj- Napoca, Romania, [email protected] 2Department of Microbiology, County Emergency Clinical Hospital, 400006, Cluj-Napoca, Romania E-mail: [email protected]; Received: May 15, 2020; Revised: June 01, 2020; Published: June 15, 2020 Abstract Parkinson’s disease (PD) is a progressive neurodegenerative disease. Levodopa in combination with amantadine has a demonstrated efficacy in motility impairment. An extensive investigation of some enzymes described to be upregulated or downregulated in PD was made – adenylate kinase (AK), adenine phosphoribosyltransferase (APRT), ectonucleoside triphosphate diphosphohydrolase 1 (ENTPD1), nucleoside-diphosphate kinase 3 (NDK3), purine nucleoside phosphorylase 1 (PNP1), and ecto-5’- nucleotidase (NT5E). Also, creatine kinase (CK) was included in the study because it is one of the main enzymes involved in the regulation of the nucleotide ratio in energy metabolism. To date, there is no proven link between amantadine treatment of PD and these enzymes. Because there are many AKs isoforms modified in PD, the AK was the first investigated. The molecular docking experiments allow the analysis of the selective binding of amantadine – unionized (with –NH2 group) and ionized form (with – + NH3 group) – to the AKs’ isoforms implicated in PD. Using available X-ray 3D structures of human AKs in closed-conformation, it was demonstrated that there are notable differences between the interactions of the two forms of amantadine for the zebrafish AK1 (5XZ2), human AK2 (2C9Y), human AK5 (2BWJ), and AK from B.stearothermophilus. -

1 Supporting Information for a Microrna Network Regulates
Supporting Information for A microRNA Network Regulates Expression and Biosynthesis of CFTR and CFTR-ΔF508 Shyam Ramachandrana,b, Philip H. Karpc, Peng Jiangc, Lynda S. Ostedgaardc, Amy E. Walza, John T. Fishere, Shaf Keshavjeeh, Kim A. Lennoxi, Ashley M. Jacobii, Scott D. Rosei, Mark A. Behlkei, Michael J. Welshb,c,d,g, Yi Xingb,c,f, Paul B. McCray Jr.a,b,c Author Affiliations: Department of Pediatricsa, Interdisciplinary Program in Geneticsb, Departments of Internal Medicinec, Molecular Physiology and Biophysicsd, Anatomy and Cell Biologye, Biomedical Engineeringf, Howard Hughes Medical Instituteg, Carver College of Medicine, University of Iowa, Iowa City, IA-52242 Division of Thoracic Surgeryh, Toronto General Hospital, University Health Network, University of Toronto, Toronto, Canada-M5G 2C4 Integrated DNA Technologiesi, Coralville, IA-52241 To whom correspondence should be addressed: Email: [email protected] (M.J.W.); yi- [email protected] (Y.X.); Email: [email protected] (P.B.M.) This PDF file includes: Materials and Methods References Fig. S1. miR-138 regulates SIN3A in a dose-dependent and site-specific manner. Fig. S2. miR-138 regulates endogenous SIN3A protein expression. Fig. S3. miR-138 regulates endogenous CFTR protein expression in Calu-3 cells. Fig. S4. miR-138 regulates endogenous CFTR protein expression in primary human airway epithelia. Fig. S5. miR-138 regulates CFTR expression in HeLa cells. Fig. S6. miR-138 regulates CFTR expression in HEK293T cells. Fig. S7. HeLa cells exhibit CFTR channel activity. Fig. S8. miR-138 improves CFTR processing. Fig. S9. miR-138 improves CFTR-ΔF508 processing. Fig. S10. SIN3A inhibition yields partial rescue of Cl- transport in CF epithelia. -
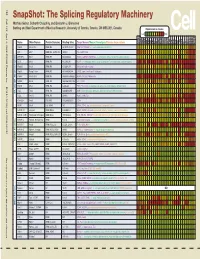
Snapshot: the Splicing Regulatory Machinery Mathieu Gabut, Sidharth Chaudhry, and Benjamin J
192 Cell SnapShot: The Splicing Regulatory Machinery Mathieu Gabut, Sidharth Chaudhry, and Benjamin J. Blencowe 133 Banting and Best Department of Medical Research, University of Toronto, Toronto, ON M5S 3E1, Canada Expression in mouse , April4, 2008©2008Elsevier Inc. Low High Name Other Names Protein Domains Binding Sites Target Genes/Mouse Phenotypes/Disease Associations Amy Ceb Hip Hyp OB Eye SC BM Bo Ht SM Epd Kd Liv Lu Pan Pla Pro Sto Spl Thy Thd Te Ut Ov E6.5 E8.5 E10.5 SRp20 Sfrs3, X16 RRM, RS GCUCCUCUUC SRp20, CT/CGRP; −/− early embryonic lethal E3.5 9G8 Sfrs7 RRM, RS, C2HC Znf (GAC)n Tau, GnRH, 9G8 ASF/SF2 Sfrs1 RRM, RS RGAAGAAC HipK3, CaMKIIδ, HIV RNAs; −/− embryonic lethal, cond. KO cardiomyopathy SC35 Sfrs2 RRM, RS UGCUGUU AChE; −/− embryonic lethal, cond. KO deficient T-cell maturation, cardiomyopathy; LS SRp30c Sfrs9 RRM, RS CUGGAUU Glucocorticoid receptor SRp38 Fusip1, Nssr RRM, RS ACAAAGACAA CREB, type II and type XI collagens SRp40 Sfrs5, HRS RRM, RS AGGAGAAGGGA HipK3, PKCβ-II, Fibronectin SRp55 Sfrs6 RRM, RS GGCAGCACCUG cTnT, CD44 DOI 10.1016/j.cell.2008.03.010 SRp75 Sfrs4 RRM, RS GAAGGA FN1, E1A, CD45; overexpression enhances chondrogenic differentiation Tra2α Tra2a RRM, RS GAAARGARR GnRH; overexpression promotes RA-induced neural differentiation SR and SR-Related Proteins Tra2β Sfrs10 RRM, RS (GAA)n HipK3, SMN, Tau SRm160 Srrm1 RS, PWI AUGAAGAGGA CD44 SWAP Sfrs8 RS, SWAP ND SWAP, CD45, Tau; possible asthma susceptibility gene hnRNP A1 Hnrnpa1 RRM, RGG UAGGGA/U HipK3, SMN2, c-H-ras; rheumatoid arthritis, systemic lupus