Spine and Peripheral Nerves
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dick Tracy.” MAX ALLAN COLLINS —Scoop the DICK COMPLETE DICK ® TRACY TRACY
$39.99 “The period covered in this volume is arguably one of the strongest in the Gould/Tracy canon, (Different in Canada) and undeniably the cartoonist’s best work since 1952's Crewy Lou continuity. “One of the best things to happen to the Brutality by both the good and bad guys is as strong and disturbing as ever…” comic market in the last few years was IDW’s decision to publish The Complete from the Introduction by Chester Gould’s Dick Tracy.” MAX ALLAN COLLINS —Scoop THE DICK COMPLETE DICK ® TRACY TRACY NEARLY 550 SEQUENTIAL COMICS OCTOBER 1954 In Volume Sixteen—reprinting strips from October 25, 1954 THROUGH through May 13, 1956—Chester Gould presents an amazing MAY 1956 Chester Gould (1900–1985) was born in Pawnee, Oklahoma. number of memorable characters: grotesques such as the He attended Oklahoma A&M (now Oklahoma State murderous Rughead and a 467-lb. killer named Oodles, University) before transferring to Northwestern University in health faddist George Ozone and his wild boys named Neki Chicago, from which he was graduated in 1923. He produced and Hokey, the despicable "Nothing" Yonson, and the amoral the minor comic strips Fillum Fables and The Radio Catts teenager Joe Period. He then introduces nightclub photog- before striking it big with Dick Tracy in 1931. Originally titled Plainclothes Tracy, the rechristened strip became one of turned policewoman Lizz, at a time when women on the the most successful and lauded comic strips of all time, as well force were still a rarity. Plus for the first time Gould brings as a media and merchandising sensation. -

5 Expos Lesclat Dels Classics L
L’esclat dels clàssics Còmics i tebeos (1900-1950) DIPUTACIÓ DE VALÈNCIA EXPOSICIONS/EXPOSICIONES Textos Vicent Sanchis, Enric Melego, Valeria Suárez President de la Diputació de València/Presidente de la “L’esclat dels clàssics: Contrastos entre els grans mestres de Diputació de València la historieta nord-americana (1900-1945)” Traducció a l’anglés dels textos/Traducción al inglés de los Antoni Francesc Gaspar Ramos textos Comissari/Comisario Begoña García Soler Diputat de l’Àrea de Cultura/Diputado del Área de Cultura Enric Melego i Trilles Xavier Rius i Torres Coordinació tècnica/Coordinación técnica Muntatge/Montaje María José Navarro Josearte SL MUSEU VALENCIÀ DE LA IL·LUSTRACIÓ I DE LA Disseny expositiu/Diseño expositivo Pintura MODERNITAT (MUVIM) Alejandro Muñoz Ariño Teodosio Caballero Rodas Enmarcat/Enmarcado Director Disseny gràfic/Diseño gráfico Pilar Torrijos Rafael Company i Mateo Valeria Suárez Conde Transport/Transporte Subdirectora Textos Art i clar Carmen Ninet Vicent Sanchis, Enric Melego, Alejandro Muñoz, Valeria Suárez Il·luminació/Iluminación Cap d’exposicions/Jefe de exposiciones Grupo Luz Amador Griñó Traducció a l’anglés dels textos/Traducción al inglés de los textos Assegurances/Seguros Cap d’Investigació i Gestió Cultural/Jefe de investigación Begoña García Soler Generalli y gestión cultural Marc Borràs i Barberà Correcció de textos/Corrección de textos Fons procedents de col·leccions privades Unitat de Normalització Lingüística de la Diputació de Fondos procedentes de colecciones privadas Cap de protocol i -

Loac Essentials Volume 1 Baron Bean (Library of American Comics Essentials) Pdf, Epub, Ebook
LOAC ESSENTIALS VOLUME 1 BARON BEAN (LIBRARY OF AMERICAN COMICS ESSENTIALS) PDF, EPUB, EBOOK George Herriman | 328 pages | 04 Dec 2012 | Idea & Design Works | 9781613774427 | English | United States Loac Essentials Volume 1 Baron Bean (Library Of American Comics Essentials) PDF Book Add links. This comic strip —related article is a stub. This book reprints the entire first year of daily comics. In The Family Upstairs the artist used the bottom part of each panel to narrate the stories of the Dingbats' pet, Krazy Kat, and a mouse named Ignatz, whose adventures were unrelated to those of the Dingbats. The unfortunate feline is in love with Ignatz, who does not reciprocate his feelings or her? Included inthis volume is the first year. In the late s, Sidney Smith developed a formula of the daily strip thatwould make The Gumps one of the most popular comics of thes and himself one of the richest …. Please update this article to reflect recent events or newly available information. The adventures take place in the kingdom of Moo, featuring Oop, his girlfriend Oola, and Dinny the dinosaur. Utgiven This item is not in stock. The strip's subtleties and surrealism never made it very popular with the public en masse, but it had an enthusiastic following among artistic and intellectual circles. The Amazing Spider-Man. But the artist's most ardent supporter was William Randolph Hearst. Here for the first time since the story made headlines across America in the spring of we reprint the saga that Hogan's Alley magazine called "One of the Ten Biggest Events in Comics History"-a tale that has lost none of its power to captivate readers in the 21st Century. -

Riverside Quarterly V4#4
239 RIVERSIDE QUARTERLY March 1971 Vol. 4, No. 4 RQMISCELLANY Editors: Leland Sapiro, Jim Harmon, David Lunde, Bill Blackbeard, Redd Boggs, Jon White. Send poetry to David Lunde, 1179 Central Ave, Dunkirk, NY 14048, A TALE OF TWO CITIES all other correspondence to 40 University Sta., Regina, Canada. Listed here, in chronological order, are just the essentials: Eurcon I, Trieste, 12-16 July, 1971; supporting membership is #4 and atten’lng membership is 57, the latter including admis table of contents sion to the S-F Film Festival. Write to Paulo Cossato, D-4000 RQ Miscellany.................................................... 239 Wittlaer, Wittgatt-85, West Germany. Animism and Magic in Tolkien's "The Lord of the Rings" Noreascon (29th World S-F Convention), Boston, 3-6 Sept., .................Patrick J. Callahan...240 1971; respective costs are 54 and 56. Send queries to Anthony Room 402 ................................... ..Steven Saffer................... 250 Lewis, 33 Unity Ave, Belmont, MA 02178. Concerning Horses; Concerning Apes....Stephen Scobie..................258 Song for a Child at Winter Solstice...Angus M. Taylor...............263 The Flowers of Spring "CURATOR OF THE COMICS" Frostop Pam and the Lost Lady Mining Company Our new columnist was subject for a one-page interview in the ..................................................Peter W. Warren.............264 10 December San Francisco Examiner, from which I quote: Afternoon.................................................................... Kenneth Decker.................265 Bill Blackbeard...is founder-director of the...Academy The God Figure in Dystopian Fiction...Mary S. Weinkauf............266 of Comic Art Z-2076 Golden Gate, San Francisco 94115./ , . a treasure house filled with examples of that unique Ameri The Gernsback "Magazines" No One Knows can cultural phenomenon known as the comic strip. -

Los Creadores De La Narrativa Gráfica
NARRATIVA GRÁFICA Los creadores de la narrativa gráfica 01. Los inicios .................................................................................................................................................2 Winsor McCay [1869·1934].......................................................................................................................2 George Joseph Herriman [1880·1944]......................................................................................................3 02. Los syndicates...........................................................................................................................................4 Clift Sterret..................................................................................................................................................5 La permanencia de las series.....................................................................................................................6 Chic Young .................................................................................................................................................7 Elzie Crisler Segar [1894·1938] .................................................................................................................7 Chester Gould.............................................................................................................................................8 03. Animales antropomorfos.........................................................................................................................9 -

Nieuwigheden Anderstalige Strips 2012 Week 2
NIEUWIGHEDEN ANDERSTALIGE STRIPS 2012 WEEK 2 Engelstalig: Avengers Academy: Will We Use This in the Real World? 19,99 (Mike McKone & Christos Gage – Marvel) Batman: The Return of Bruce Wayne 19,99 (Grant Morrison – DC Comics) Ender’s Game: Ultimate Collection 29,99 (Orson Scott Card – Marvel) Generation Hope: Schism 16,99 (Salvador Espin & Kieron Gillen – Marvel) Hulk 34,99 (Ron Garney & John Byrne – Marvel) Spawn: Origins Collection 13 14,99 (Diverse auteurs – Todd McFarlane Productions) X-Men: Age of X 24,99 (Diverse auteurs – Marvel) Manga – Engelstalig: Gantz 20 12,99 (Hiroya Oku – Dark Horse Manga) Naruto 54 9,99 (Masashi Kishimoto – Viz Media) Negima Omnibus 3 19,99 (Ken Akamatsu – Kodansha Comics) Shonen Jump 108: February 2012 4,99 WEEK 3 Engelstalig: Ghost Rider: Ultimate Collection 34,99 (Mark Texeira & Daniel Way – Marvel) Steve Canyon 1: 1947-1948 49,99 (Milton Caniff / IDW Publishing) The Unwritten 5: On To Genesis 14,99 (Peter Gross & Mike Carey – Vertigo) Wolverine: Contagion 19,99 (Juan Ryp & Charlie Huston – Marvel) Manga – Engelstalig: Naruto: The Official Character Data Book 14,99 (Masashi Kishimoto – Viz Media) Wandering Son: Volume 2 19,99 (Shimura Takako – Fantagraphics Books) WEEK 4 Engelstalig: Daken vs X-23: Collision 19,99 (Will Conrad & Daniel Way – Marvel) Marvel Firsts 1: The 1970s 29,99 (Diverse auteurs – Marvel) Marvel Point One II 24,99 (Diverse auteurs – Marvel) The New Defenders vol. 1 29,99 (Diverse auteurs – Marvel) The Twelve vol. 1 16,99 (Chris Weston & J. Michael Straczynski – Marvel) WEEK 5 Engelstalig: -

Magazines V17N9.Qxd
July COF C1:Customer 6/7/2012 1:32 PM Page 1 ORDERS DUE th 18JUL 2012 JUL E E COMIC H H T T SHOP’S CATALOG 07 JULY COF Apparel Shirt Ad:Layout 1 6/7/2012 12:16 PM Page 1 CAPTAIN AMERICA/IRON MAN” DUAL NATURE” GREY T-SHIRT Available only PREORDER NOW! from your local comic shop! BACK STAR WARS: “DARTH LUKE CAGE & POWER ADVENTURE TIME: VADER’S LAST STAND” MAN YELLOW T-SHIRT “WIGGLY LEGS COSTUME” WHITE T-SHIRT PREORDER NOW! WHITE T-SHIRT PREORDER NOW! PREORDER NOW! COF Gem Page July:gem page v18n1.qxd 6/7/2012 10:33 AM Page 1 THE SHAOLIN COWBOY GHOST #0 ADVENTURE MAGAZINE TP DARK HORSE COMICS DARK HORSE COMICS TALON #0 DC COMICS STIEG LARSSON’S THE GIRL WITH THE STAR TREK: THE NEXT DRAGON TATTOO VOL. 1 HC GENERATION: HIVE #1 DC COMICS/VERTIGO IDW PUBLISHING GUARDING THE GLOBE #1 IMAGE COMICS ULTIMATE COMICS HAPPY! #1 ULTIMATES #16 IMAGE COMICS MARVEL COMICS COF FI page:FI 6/7/2012 11:20 AM Page 1 FEATURED ITEMS COMICS & GRAPHIC NOVELS New Crusaders: Rise of the Heroes #1G ARCHIE COMIC PUBLICATIONS Crossed: Wish You Were Here Volume 1 TP/HC G HALLOWEEN COMICSFEST G Halloween Mini Comics Mega Bundle 2012 PREVIEWS PUBLICATIONS 1 COMICS & GRAPHIC NOVELS 1 Sonic The Hedgehog: The Complete Comic Encyclopedia TP G ARCHIE COMICS Fashion Beast #1 G AVATAR PRESS The Simpsons‘ Treehouse of Horror #18 G BONGO COMICS The Lookouts: Riddle #1 G CRYPTOZOIC ENTERTAINMENT Peter Cannon: Thunderbolt #1 G D. -

Bandes Dessinées
29 MAI 2015 = PARIS = DROUOT BANDES DESSINÉES EXPERTS Roland BURET Alexis CHEVALIER = = ALBUMS PLANCHES JOUETS Becassine = n° 397 Lionel Santa Car n° 334 Visuel de couverture Mickey Train = n° 333 Franquin = n° 240 BANDES DESSINÉES Vente aux Enchères Publiques PARIS = HÔTEL DROUOT = Salle 11 9, rue Drouot = 75009 Paris Tél. : 01 48 00 20 11 VENDREDI 29 MAI 2015 = 13h30 Tirages de Tête Portfolios Mangas Editions étrangères Albums dédicacés Périodiques Comics Cartes Postales Sérigraphies Albums rares Petits Formats Récits Complets Jeux et Jouets Figurines Planches et dessins - Autour de « Charlie Hebdo ». EXPERTS Roland BURET 6, passage Verdeau = 75009 Paris Tél. : 06 80 66 50 36 = Fax : 01 42 46 00 75 [email protected] Alexis CHEVALIER Librairie Le Pélican Noir Tél. : 06 09 28 13 25 [email protected] Expositions publiques : Paris = Hôtel Drouot = salle 11 Jeudi 28 mai de 11h à 18h Vendredi 29 mai de 11h à 12h Catalogue et photos en ligne sur www.tessier-sarrou.com S.A.R.L. = Agrément 2001-014 8, rue Saint-Marc = 75002 Paris Tél. : 01 40 13 07 79 = Fax : 01 42 33 61 94 E-mail : [email protected] Moebius = n° 228 Moebius = n° 226 Barbier = n° 222 Lot n° 230 Gotlib, Greg, Herriman, Jacovitti... = n° 211 Moebius / Giraud = n° 10 Moebius = n° 226 VENTE LE 29 MAI à 13h30 TIRAGES LIMITÉS & TIRAGES de TÊTES 1 Lot de 4 volumes en tirage limité, dont Crepax Arno et Jodorowsky : L’enfant-tronc (1985 – édition Jonas numérotée et signée) - Bati : Megadorma (Portable Aedena, n. et s. 1986) - Cattaneo : Entropie, mon amour (1997 ed. -
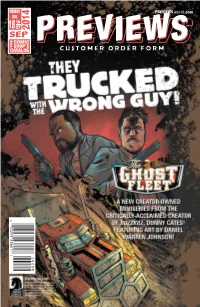
Customer Order Form
ORDERS PREVIEWS world.com DUE th 18 SEP 2014 SEP COMIC THE SHOP’S PREVIEWSPREVIEWS CATALOG CUSTOMER ORDER FORM CUSTOMER 601 7 Sep14 Cover ROF and COF.indd 1 8/7/2014 9:52:40 AM Sep14 Future Dudes_ROF.indd 1 8/7/2014 9:06:06 AM RESURRECTIONISTS ODYC #1 #1 IMAGE COMICS DARK HORSE COMICS GOTHAM BY MIDNIGHT #1 DC COMICS ITTY BITTY COMICS: TOOTH & CLAW #1 THE MASK #1 IMAGE COMICS DARK HORSE COMICS SHADOW SHOW #1 IDW PUBLISHING WONDER WOMAN SPIDER-VERSE #1 #36 MARVEL COMICS DC COMICS Sep14 Gem Page ROF COF.indd 1 8/7/2014 1:16:41 PM FEATURED ITEMS COMIC BOOKS & GRAPHIC NOVELS Dark Gods #1 l Avatar Press Deep State #1 l BOOM! Studios Capture Creatures #1 l BOOM! STUDIOS Django/Zorro #1 l D.E./Dynamite Entertainment John Carter: Warlord of Mars #1 l D.E./Dynamite Entertainment 1 The Overstreet Guide to Grading Comics SC l Gemstone The Life After Volume 1 TP l Oni Press 1 Doctor Who: The Tenth Doctor Volume 1: Revolution of Terror HC l Titan Comics Doctor Who: The Eleventh Doctor Volume 1: After Life HC l Titan Comics All You Need Is Kill 2-in-1 GN l Viz Media Grimm Fairy Tales: Cinderella #1 l Zenescope Entertainment BOOKS The Art of Robert E. McGinnis HC l Art Books Walter Baumhofer HC l Art Books 2 The Art of the Simon and Kirby Studio l Comics MAGAZINES Marvel Chess Collection #21: Wasp White Pawn l Eaglemoss Marvel Chess Collection #22: Viper Black Queen l Eaglemoss Marvel Fact Files Special #5: Deadpool l Eaglemoss Horrorhound #50 l Horror 2 TRADING CARDS Topps 2014 Strata Football Trading Cards l Topps Company Star Trek Aliens Trading Cards -
Customer Order Form
#358 | JUL18 PREVIEWS world.com ORDERS DUE JUL 18 THE COMIC SHOP’S CATALOG PREVIEWSPREVIEWS CUSTOMER ORDER FORM CUSTOMER 601 7 Jul18 Cover ROF and COF.indd 1 6/7/2018 4:07:20 PM Celebrate Halloween at your local comic shop! Get Free Comics the Saturday before Halloween!” HalloweenComicFest.com /halloweencomicfests @Halloweencomic halloweencomicfest HCF17 STD_generic_SeeHeadline_OF.indd 1 6/7/2018 3:58:11 PM BATMAN/THE MAXX #1 BULLY WARS #1 IDW PUBLISHING IMAGE COMICS HEROES IN CRISIS #1 DC COMICS MAN-EATERS #1 ICEMAN #1 IMAGE COMICS MARVEL COMICS BATMAN: DAMNED #1 DC COMICS STRANGER THINGS #1 JAMES BOND: DARK HORSE COMICS ORIGIN #1 DYNAMITE ENTERTAINMENT STAR TREK VS. TRANSFORMERS #1 MYSTERY SCIENCE IDW PUBLISHING LOW ROAD THEATER 3000 #1 WEST #1 DARK HORSE COMICS BOOM! STUDIOS Jul18 Gem Page ROF COF.indd 1 6/7/2018 3:59:27 PM FEATURED ITEMS COMIC BOOKS & GRAPHIC NOVELS 1 Strangers In Paradise XXV Volume 1: The Chase TP l ABSTRACT STUDIOS Moth & Whisper #1 l AFTERSHOCK COMICS Spookhouse 2 #1 l ALBATROSS FUNNYBOOKS Hatchet: Vengeance #1 l AMERICAN MYTHOLOGY PRODUCTIONS Backstagers & The Ghost Light Illustrated Novel HC l AMULET BOOKS 1 Archie 1941 #1 l ARCHIE COMIC PUBLICATIONS DC Comics Heroines: 100 Greatest Moments HC l CHARTWELL BOOKS La Muerta Lives! TP/HC l COFFIN COMICS The Art of Walt Disney’s Mickey Mouse Hc l DISNEY EDITIONS Iron Maiden: Legacy of the Beast TP l HEAVY METAL MAGAZINE The Art and Humor of Johnny Hart HC l HERMES PRESS Star Trek: Encyclopedia of Starfleet Starships 2151-2293 l HERO COLLECTOR Horrorhound #73 l HORRORHOUND -

Nieuwigheden Anderstalige Strips 2018
NIEUWIGHEDEN ANDERSTALIGE STRIPS 2018 WEEK 1 ENGELSTALIG: Blue Beetle - Rebirth 2: Hard Choices (€ 16,99) (Scott Kolins & Keith Giffen - DC) B.P.R.D. Hell on Earth Omnibus HC 1 (€ 34,99) (Guy Davis & Mike Mignola - Dark Horse) Doctor Strange 4: Mr. Misery (€ 19,99) (Frazer Irving & Jason Aaron - Marvel) Elsewhere 1 (€ 9,99) (Sumeyye Kesgin & Jay Faerber - Image) Injustice: Ground Zero 1 (€ 16,99) (Pop Mhan & Brian Buccellato - DC) Robin 5: War of the Dragons (€ 24,99) (Tim Grummett & Chuck Dixon - DC) Saga 8 (€ 14,99) (Fiona Staples & Brian K. Vaughan - Image) Spider-Man / Deadpool 4: Serious Business (€ 15,99) (Will Robson & Joshua Corin - Marvel) The Art of Magic the Gathering: Ixalan (€ 39,99) (Diverse tekenaars - Viz Media) Vampirella 1: Forbidden Fruit (€ 19,99) (Jimmy Broxton & Paul Cornell - Dynamite) MANGA ENGELSTALIG: Anonymous Noise 6 (€ 9,99) (Ryoko Fukuyama - Viz Media) Attack on Titan: Before the Fall 12 (€ 10,99) (Satoshi Shiki & Ryo Suzukaze - Kodansha) Blue Exorcist 18 (€ 9,99) (Kazue Kato - Viz Media) Drifters 5 (€ 13,99) (Kohta Hirano - Dark Horse Manga) Naruto: Chibi Sasuke’s Sharingan Legend 2 (€ 9,99) (Kenji Taira & Masashi Kishimoto - Viz Media) Neon Genesis Evangelion: Legend of the Piko Piko Middle School Students 2 (€ 11,99) (Yushi Kawata & Yukito - Dark Horse Manga) The Water Dragon’s Bride 4 (€ 9,99) (Rei Toma - Viz Media) Unmagical Girl 1 (€ 12,99) (Mammaru Uetsuki & Ryouchi Yokoyama - Seven Seas) 7th Garden 7 (€ 9,99) (Mitsu Izumi - Viz Media) WEEK 2 ENGELSTALIG: Batman - Rebirth 2: Rise of the Demon (€ 16,99) (Bernard Chang & Dan Jurgens - DC) Batman: Shadow of the Bat 3 (€ 24,99) (Bob Smith & Alan Grant - DC) Descender 5: Rise of the Robots (€ 16,99) (Dustin Nguyen & Jeff Lemire - Image) Farscape Omnibus 1 (€ 39,99) (Joe Corroney & Rockne S. -

Corporate Registry Registrar's Periodical Template
Service Alberta ____________________ Corporate Registry ____________________ Registrar’s Periodical REGISTRAR’S PERIODICAL, MAY 15, 2012 SERVICE ALBERTA Corporate Registrations, Incorporations, and Continuations (Business Corporations Act, Cemetery Companies Act, Companies Act, Cooperatives Act, Credit Union Act, Loan and Trust Corporations Act, Religious Societies’ Land Act, Rural Utilities Act, Societies Act, Partnership Act) 0713822 B.C. LTD. Other Prov/Territory Corps 1664177 ALBERTA LTD. Numbered Alberta Registered 2012 APR 12 Registered Address: #400 1111 Corporation Incorporated 2012 APR 10 Registered 11TH AVENUE SW, CALGARY ALBERTA, T2R Address: #300, 2912 MEMORIAL DRIVE S.E., 0G5. No: 2116710498. CALGARY ALBERTA, T2A 6R1. No: 2016641777. 0843008 B.C. LTD. Other Prov/Territory Corps 1666355 ALBERTA LTD. Numbered Alberta Registered 2012 APR 12 Registered Address: P.O. BOX Corporation Incorporated 2012 APR 10 Registered 473, NW 19-21-14-W4, DUCHESS ALBERTA, T0J Address: 128 BAYSIDE LANDING SW, AIRDRIE 0Z0. No: 2116710506. ALBERTA, T4B 3E3. No: 2016663557. 0933341 B.C. LTD. Other Prov/Territory Corps 1667789 ALBERTA LTD. Numbered Alberta Registered 2012 APR 11 Registered Address: BOX Corporation Incorporated 2012 APR 03 Registered 7649, 5108 53 STREET, DRAYTON VALLEY Address: 27 PANATELLA ROW NW, CALGARY ALBERTA, T7A 1S2. No: 2116707387. ALBERTA, T3K 0V5. No: 2016677896. 0937049 B.C. LTD. Other Prov/Territory Corps 1668479 ALBERTA LTD. Numbered Alberta Registered 2012 APR 04 Registered Address: SUITE Corporation Incorporated 2012 APR 02 Registered 204, 205-9TH AVENUE S.E., CALGARY ALBERTA, Address: 3702 DOVER RIDGE DRIVE SE, CALGARY T2G 0R3. No: 2116696374. ALBERTA, T2B 2C8. No: 2016684793. 0937751 B.C. LTD. Other Prov/Territory Corps 1668482 ALBERTA LTD.