Bhutan Parliamentarian's Forum for Ncds.Indd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Engthen the Financial Management System the General Auditing Rules and Regulations (GARR) Was Issued in 1989
Annual Audit Report 2004 Part I Background By virtue of the Kashos and the provisions contained in the General Auditing Rules and Regulations of Bhutan (GARR), the Royal Audit Authority (RAA), the Supreme Audit Institution (SAI) of Bhutan is responsible for audit of public sector agencies and reporting its findings. In 1961, the 16th Session of the National Assembly of Bhutan formed a committee of Accounts and Audit in response to the need for establishing accountability. The Committee would comprise of one representative of the King and one representative each from the Cabinet, People and the Monk Body all nominated by the King. The Royal Government issued the first edition of the Financial Manual in 1963. The manual provided for the organization of the Development Wing of the government and the Accounts and Audit for the Development Wing. The Accounts and Audit Wing maintained the books of accounts, conducted budgetary controls of revenues and expenditures, and undertook periodic audit and inspection of accounts and records. In October 1969 the 31st Session of the National Assembly based on a motion proposed by the King to delegate the auditing authority voted for the appointment of Royal Auditors to conduct the audit of accounts and records of the Royal Government. Consequently, the four Royal Auditors were appointed on 16th April 1970 under a Royal Kasho. The Kasho defined and authorized the jurisdiction of the then Royal Audit Department as primarily responsible for the audit of accounts of the Ministry of Finance, Ministries, the Royal Bhutan Army, the Royal Bhutan Police and His Majesty’s Secretariat. -

Dzongkhag Civil Registration and Census Office, Sarpang Dzongkhag-Wise List of CID Cards Available for Other Dzongkhags)
Dzongkhag Civil Registration and Census Office, Sarpang Dzongkhag-wise list of CID cards available for other Dzongkhags) Note: The list is being shared in the interest of those applicants from other Dzongkhags who have availed CID service from this Dzongkhag administration. Telephone No. 06-365102 (Office) Total:900 Cards 10 July, 2018 1:06 PM Slno Name CID no Gewog Card Received on Total Cards: 10 Bumthang 1 Choki Dema 12001002734 Chokhor 11-06-2018 2 Karma Chophel 10104000179 Ura 11-06-2018 3 Phuntsho 10101001200 Chokhor 11-06-2018 4 Rinchen Peday 10103002174 Tang 11-06-2018 5 Rinchen Tenzin 10102000608 Chumey 11-06-2018 6 Sonam Penjor 10103001845 Tang 11-06-2018 7 Thinley Tenzin 10104000224 Ura 01-05-2018 8 Tshering Dorji 10101003275 Chokhor 11-06-2018 9 Ugyen Dorji 10104001208 Ura 28-10-2017 10 Wangda Dorji 10604000704 Chumey 20-02-2018 Total Cards: 34 Chukha 1 Bhakta Bdr. Ghalley 10211000670 Phuntsholing 12-03-2018 2 Bhimla Kumari Thapa 10211002187 Phuntsholing 11-06-2018 3 Chimi Dorji 10203001379 Bongo 11-06-2018 4 Dawa Lepcha 10211000249 Phuntsholing 31-03-2018 5 Dhan Kumar Raika Mongar 10205003240 Darla 28-10-2017 6 Dik Man Rai 10211000105 Phuntsholing 11-06-2018 7 Dorji Gyeltshen 10206000337 Dungna 11-06-2018 8 Dyal Singh Mongar 10211002208 Phuntsholing 11-06-2018 9 Gangla 10201001187 Sampheling/Bhalujora 12-03-2018 10 Jaga Bir Rai 10211000036 Phuntsholing 11-06-2018 11 Kamal Kumari Thapa 10201001034 Sampheling/Bhalujora 11-06-2018 12 Kunti Maya Dahal 10205000013 Darla 20-10-2017 13 Man Maya Mongar 10211002637 Phuntsholing 11-06-2018 14 Meena Kumari Tamang 10201002478 Phuntsholing Throm 12-03-2018 15 Mon Bdr. -

Construction Development Board
LIST OF PARTICIPANTS FOR REFRESHER COURSE LARGE AND MEDIUM CONTRACTORS FROM 20th - 22nd JANUARY 2020 AT CST, PHUENTSHOLING CID/Work Permit No. Sl# CDB# Name of Firm Class Name of Participant of Participant KENCHO DORJI 1 1043 L Kencho Dorji 102022000997 Construction Private Limited 2 2631 YARKAY Construction L Geeta Gurung 11216001231 YANGKHIL Construction Private 3 2182 L Phuentsho T Norbu 10606001676 Limited DRUK KUNZANG 4 4060 L Passang Dorji 11402000211 Construction Pvt.Ltd LHENDUP NORBU 5 7030 L Sangay Norbu 11105002162 Construction 6 4181 Jadung Engineering Private Limited L Choki Mo 11703002492 7 1081 MINDU Construction Private Limited L Tashi Jigme 10803000757 DHODTER RIGTSEL 8 5116 L Karma tshomo 11101001199 Company Private Limited SONAM JAMTSHO & BROS 9 3248 L Sonam Jamtsho 10606001512 CONSTRUCTIONPVT. LTD. 10 1542 D Lhen Private Limited L Suman Chhetei 11202004922 11 1811 K.D Builders Private Limited L Sudesh Pradhan 11208004258 12 3206 BHUTAN Construction Private Limited L Ngawang Delkar 10711002326 PELJOR LHENDUP 13 6712 L Ugyen Tshewang 11605003208 Construction Private Limited Chaggwong Construction Private 14 1033 L Dechen Yangzom 12008002562 Limited 15 3531 YONGPHEL Builders M chophel 10703002484 16 2920 WANGMO Construction M Sanjana Darjee 10308003433 SANGAY THINLEY 17 1432 M Madan Ghalley 11303000869 Construction 18 1846 PEMA Construction M Pema Rinzin 11703001736 19 1757 CHETHUN Construction M Wangchuk 10603000362 20 3155 C.T Construction M Karma 11501001834 21 7276 DALA Construction M Dawa Tsirang 10807001643 K-RANGRIK 22 3061 M Tashi Choden 11505003436 Construction Company Private Limited 23 4074 2Q Engineering Works Private Limited M Kinzang Dorji 11803001018 RINZIN DORJI 24 1099 M Rinzin Dorji 10605000105 Construction 25 3447 SANGAY D Construction M Sangay Dema 11411000024 LHOJONG Construction Private 26 1862 M Kinley Om 11008000886 Limited 27 1994 LAMA Industry M Anil Lama 10308002127 28 7093 Bumzang Builders M Jangchub Yoeser 10701001503 29 8080 FANTHOG Builders M Pema Choney 12007001145 30 5747 Guardian Construction Pvt. -

Monthly E-Newsletter of the Embassy of India, Thimphu
9/7/2020 BILATERAL: Covid-19 RT-PCR test kits to Bhutan | elink Monthly E-Newsletter of the Embassy of India in Thimphu AUGUST 2020 September 3, 2020 Dear Reader, I am delighted to present the {rst monthly e-newsletter of the Embassy of India in Thimphu! This newsletter will capture our activities in Bhutan, key developments in India and of course, heart- warming stories of community and companionship. August is, of course, a special month for us as we celebrated India's 74th Independence Day. The warm messages we received from Bhutan are an indication of the strong bonds we share, not just at the political level, but also at a personal one. The Government of India launched a slew of development initiatives in August 2020 in the areas of education, agriculture, taxation, and health, all aimed at helping India achieve self- reliance: ‘Aatma Nirbhar Bharat’. We hope you enjoy reading this {rst edition of our monthly e-newsletter. Tashi Delek! Jai Hind! - Ruchira Kamboj, Ambassador of India to Bhutan https://elink.io/p/india-in-bhutan-984c310 1/18 9/7/2020 BILATERAL: Covid-19 RT-PCR test kits to Bhutan | elink indembthimphu.gov.in BILATERAL: Covid-19 RT-PCR test kits to Bhutan 17 August 2020: The Government of India handed over the 6th consignment of medical supplies with 20,000 Covid-19 RT-PCR tests to the Royal Government of Bhutan, at Phuentsholing, to assist Bhutan in {ghting the Covid-19 pandemic. Going forward, India will continue to extend all possible support to Bhutan to minimize the health and economic impact of the COVID-19 pandemic. -
Annual Report 2015-2016
Royal Civil Service Commission Annual Report 2015-2016 ANNUAL REPORT (July 2015 - June 2016) STATE OF THE ROYAL CIVIL SERVICE Royal Civil Service Commission ROYAL GOVERNMENT OF BHUTAN Excellence in Service i Royal Civil Service Commission Annual Report 2015-2016 Excellence in Service ii Excellence in Service Royal Civil Service Commissio n Annual Report 2015-2016 Royal Civil Service Commission Annual Report 2015-2016 Table of Contents List of Abbreviations ................................................................................................................................ i INTRODUCTION ......................................................................................................................................... 1 i. Scope of the Report .......................................................................................................................... 3 ii. Commission Mee ngs ....................................................................................................................... 3 iii. Representa on of Commission in Boards/Commi ees and Lead Role in Reforms ......................... 4 iv. Focal Commissioners for Agencies .................................................................................................... 4 v. Budget Report 2015-2016 ................................................................................................................. 5 PART 1: CIVIL SERVICE STATISTICS - KEY HIGHLIGHTS ....................................................................... 7 1.1 Civil -

The Executive
The Executive VOLUME I NOVEMBER 7, 2018 - NOVEMBER 7, 2019 YEAR IN OFFICE Laying foundation for change 1,000 Golden Days Plus Digital transformation Removal of “cut Teachers, the Narrowing gap Densa Meet: off” for Class X highest paid civil through pay the other servant revision Mines and Cabinet Minerals Bill AM with PM: Getting to know Revising Tourism policy 9 better Tariff revision Private sector Policies development approved committee Laying foundation for change “Climb higher on the shoulders of past achievements - your task is not to fill old shoes or follow a well-trodden path, but to forge a new road leading towards a brighter future.” His Majesty The King Royal Institute of Management August 9, 2019 Contents • Introduction 8 • From the Prime Minister 10 • Initiating change 13 • Country before party 14 • Revisiting our vision 15 • The 12th Plan is critical 18 • The Nine Thrusts 19 • Densa, the other Cabinet 22 • High value, low volume tourism 22 • More focus on health and education 24 • AM with PM: A dialogue with the Prime Minister 25 • Investing in our children 26 • Pay revised to close gap 27 • Rewarding the backbone of education 28 • Taking APA beyond formalities 29 • Block grant empowers LG 30 • Major tax reforms 30 • TVET transforms 31 • Cautious steps in hydro 32 • Encouraging responsible journalism 32 • Private sector-led economy 33 • Meeting pledges 34 • Policies Approved 36 • Guidelines reviewed and adopted 37 • Overhauling health 38 • A fair chance for every Bhutanese child 41 • Education comes first 42 • Grateful -

Medical & Biological Sciences Merit Ranking
Medicine&Biological Sciences 2021 Merit List of Registered Candidates for Medicine & Biological Sciences 2021 (Min. 60% marks each in Physics, Chemistry, Biology and 55% in English) Index Number School Name CID Sex Stream MATHS ENGLISH PHYSICS BIOLOGY Merit Rank Total Marks Total DZONGKHA CHEMISTRY Application Number CHEMISTRY + BIOLOGY ) + BIOLOGY CHEMISTRY Total ( ENGLISH + PHYSICS Total 1 941_2104S02065 Seisa Kokusai High School Nidup Dorji M 11504002968 SCIENCE 94 93 93 94 90 374 464 2 941_2104S00822 12200260018 UGYEN ACADEMY HIGHER SECONDARY SCHOOL Ugyen Thukzom F 10701001905 SCIENCE 90 99 94 81 80 90 363 534 3 941_2104S00311 12200020001 YANGCHENPHUG HIGHER SECONDARY SCHOOL Rekha Chhetri F 11203002997 SCIENCE 89 93 93 73 83 91 358 522 4 941_2104S00198 12200260027 UGYEN ACADEMY HIGHER SECONDARY SCHOOL Ngawang C Gyeltshen M 11407002491 SCIENCE 90 95 94 75 76 355 430 5 941_2104S00560 12200260083 UGYEN ACADEMY HIGHER SECONDARY SCHOOL Tashi Lhendrup Dorji M 10101005811 SCIENCE 88 93 96 75 76 86 353 514 6 941_2104S00092 12200260036 UGYEN ACADEMY HIGHER SECONDARY SCHOOL Rohan Rai M 11205001712 SCIENCE 89 94 94 66 74 83 351 500 7 941_2104S01241 12200160179 NANGKOR CENTRAL SCHOOL Pema Tshomo F 10903001512 SCIENCE 87 93 88 81 82 350 431 8 941_2104S00911 12201390133 KARMA ACADEMY Tandin Choda M 11905001182 SCIENCE 91 89 92 78 78 350 428 9 941_2104S02353 12201390157 KARMA ACADEMY Sonam Tshomo F 10804001035 SCIENCE 87 92 93 79 77 349 428 10 941_2104S01380 12200620015 TENDRUK CENTRAL SCHOOL Roshan Phuyel M 11206002979 SCIENCE 92 88 90 79 78 348 -
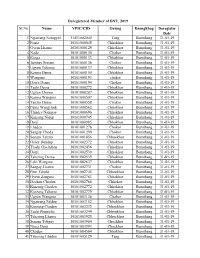
DNT Deregistered List.Xlsx
Deregistered Member of DNT, 2019 Sl.No Name VPIC/CID Gewog Dzongkhag Deregister Date 1 Ngawang Namgyel 11411002040 Tang Bumthang 31-01-19 2 Pema 10101000045 Chhokhor Bumthang 31-01-19 3 Gyem Lhamo 10101000129 Chhokhor Bumthang 31-01-19 4 Nado 10101000130 Chokor Bumthang 31-01-19 5 Kinga 10101000133 Chhokhor Bumthang 31-01-19 6 Jambay Sonam 10101000136 Chokor Bumthang 31-01-19 7 Ugyen Tshomo 10101000137 Chhokhor Bumthang 31-01-19 8 Karma Dema 10101000150 Chhokhor Bumthang 31-01-19 9 Wangmo 10101000193 chokor Bumthang 31-01-19 10 Dawa Dema 10101000194 Chokor Bumthang 31-01-19 11 Tashi Dema 10101000272 Chhokhor Bumthang 31-01-19 12 Ugyen Lhamo 10101000287 Chhokhor Bumthang 31-01-19 13 Karma Wangmo 10101000507 Chhokhor Bumthang 31-01-19 14 Tenzin Dema 10101000558 Chokor Bumthang 31-01-19 15 Pema Wangchuk 10101000562 Chhokhor Bumthang 31-01-19 16 Thinley Namgay 10101000696 Chhokhor Bumthang 31-01-19 17 Kinzang Nidup 10101000745 Chhokhor Bumthang 31-01-19 18 Dorji 10101000985 Chhokhor Bumthang 31-01-19 19 Lhaden 10101001276 Chokor Bumthang 31-01-19 20 Sangay Choda 10101001299 Chokor Bumthang 31-01-19 21 Sonam Tenzin 10101001856 Chhoekhor Bumthang 31-01-19 22 Galey Dendup 10101002372 Chhokhor Bumthang 31-01-19 23 Trashi Gyeltshen 10101002436 Chhokhor Bumthang 31-01-19 24 Dorji 10101002530 Chhokhor Bumthang 31-01-19 25 Tshering Dema 10101002539 Chhokhor Bumthang 31-01-19 26 Leki Wangmo 10101002637 Chhokhor Bumthang 31-01-19 27 Sangay Lhamo 10101002731 Chokor Bumthang 31-01-19 28 Pem Tshoki 10101002745 Chhoekhor Bumthang 31-01-19 29 Gyem Zangmo -
BHUTAN Progress Report – 2014 Global AIDS Response Progress Report
March 2014 BHUTAN Progress Report – 2014 Global AIDS Response Progress Report National HIV/AIDS and STI Prevention and Control Porgramme (NACP), MOH BHUTAN Progress Report – 2014 Table of Contents ABBREVIATIONS ............................................................................................................................................. II FOREWORD ...................................................................................................................................................... IV CHAPTER 1: STATUS AT A GLANCE ........................................................................................................... 1 1.1 METHODOLOGY: THE INCLUSIVENESS OF THE STAKEHOLDERS ........................................................................ 1 1.2 THE STATUS OF THE EPIDEMIC .............................................................................................................................. 1 1.3 POLICY AND PROGRAMMATIC RESPONSE ............................................................................................................. 2 1.4 INDICATOR DATA OVERVIEW ................................................................................................................................. 4 CHAPTER 2: OVERVIEW OF THE AIDS EPIDEMIC ................................................................................ 7 2.1 CONTEXTUAL BACKGROUND ................................................................................................................................... 7 2.1.1 Demography .......................................................................................................................................................... -

Weekly Newsletter
September 15, 2019 The Royal Academy Weekly Newsletter Vol. 1, Issue XXIII Synergy In this Issue: Obstacle course with Wangsel Institute| Sonam Chogyal, Jimi Pfinso and Tenzin Tshering(Grade IX) Dasho Sonam Kinga|Jimmy Pelbar(Grade X) Space Engineer Mrs Yeshey Choden| Nendra Wangchuk A different life| Ugyen Tshering(Grade IX) Interview| Ambassador Ruchira Khamboj (Sangay Choden Grade X) Interview|Ms Tashi Chenzom(Jamyang Ugyen Tshomo Grade X) September 15, 2019 Obstacle course with Wangsel Institute Sonam Chogyal, Jimi Pfinso and Tenzin Tsheringl(Grade IX) On Sunday we had a great time with the students from Wangsel. It was a first for all the students of The Royal Academy as we interacted with our differently abled friends from Wangsel. As the buses from Wangsel arrived we were very excited. We wanted to learn new things and show off what all we have learnt during our Friday learning experiences. The Wangsel students which are in class pp- three also joined the events taking place at our school. The smile on their faces were as bright as sun flower and the way they did the obstacle was in many ways far better than most of us as they always gave their one hundred percent which is in line with our school philosophy “ Be the best you can be”. September 15, 2019 We thoroughly enjoyed our day with them and found many new teamwork skills within us. Communicating with them taught us new things and it also strengthened our sign language skills. They gave it their best. We were able to share thoughts and ideas with them with ease after a few hours with them. -

Statistical Information on Elections in Bhutan in Elections on Information Statistical Information on Elections in Bhutan (2006-2015)
STATISTICAL Statistical Information on Elections in Bhutan INFORMATION on Elections in Bhutan (2006-2015) www.election-bhutan.org.bt (2006-2015) Election Commission of Bhutan, Post Box No. 2008, Olakha, Thimphu, Bhutan Telephone: +975-02-334851/334852, Fax: +975-02-334763 Election Statistics (2006-2015) 2006-2015 Election Commi ssion of Bhutan 1 Election Statistics (2006-2015) © Election Commission of Bhutan No part of this book may be reproduced in any form. Anybody wishing to use the name, photo, cover design, part of material or thereof in any form of this book may do so with due permission or acknowledgement of the Election Commission of Bhutan. For any querry : [email protected] 2 Election Statistics (2006-2015) The Statistical Information on Elections in Bhutan 2006-2015 is the first edition of data being published by the Election Commission of Bhutan (ECB). The book provides comprehensive statistical information of all elections that the Election Commission has conducted since its establishment in 2006 to 2015 including the First and Second Parliamentary Elections in 2008 and 2013, Thromde Elections in 2011, three phases of Local Government Elections in 2012 and series of Re-Elections and Bye-Elections for both Parliamentary and Local Government. This publication will enable readers to get reliable information related to voters, voter turnout, election officials, media coverage of elections and other relevant and available information related to elections in Bhutan. The data and information compiled in this book are based on the information collected from the polling stations, Dzongkhag Election Offices, and the ECB Head Office. The book is expected to be a source of information and serve as a data bank for any users wishing to carry out research and studies on matters related to elections in Bhutan. -

Shortlisted Candidates for Alghanim
SI No Name Gender CID Mobile number Remarks 1 Tshering lhamo Female 10101000033 17881752 Shortlisted 2 Kuenzang Dorji Male 10101000226 17565408 Shortlisted 3 Ugyen Thinley Male 10101002557 17337305 Shortlisted 4 Tshering Dekar Female 10101003966 17780223 Shortlisted 5 Sonam Yangchen Female 10101004118 17383672 Shortlisted 6 Tashi phuntsho Male 10101004507 17565349 Shortlisted 7 Samten Dorji Male 10101004624 17421575 Shortlisted 8 Pema tshoki Female 10101005103 17917647 Shortlisted 9 Karma samten Male 10101005322 17961717 Shortlisted 10 Phuntsho Gyeltshen Male 10102000474 17361913 Shortlisted 11 Jigme namgyel Male 10102001617 17893722 Shortlisted 12 chimi wangmo Female 10102001677 77334397 Shortlisted 13 Tshewang Tenzin Male 10103001762 77790469 Shortlisted 14 Gyem Tshering Male 10103002085 77439156 Shortlisted 15 Zepa lhamo Female 10103002177 17868489 Shortlisted 16 Leki Dema Female 10103002223 77801465 Shortlisted 17 Jigme lhendup Male 10104000783 17523693 Shortlisted 18 Tenzin Chime Female 10104001727 17337911 Shortlisted 19 Sherab Gyeltshen Male 10104001972 17616952 Shortlisted 20 Leela kumari Ghalley Female 10201000101 17718106 Shortlisted 21 Drishti Khampa Female 10201001035 17363336 Shortlisted 22 michael tamang Male 10201002472 77286198 Shortlisted 23 Ngawang Dorji Male 10202001373 17666415 Shortlisted 24 Tshering Dema Female 10203000467 17961747 Shortlisted 25 Wangchuk Bida Female 10203000505 77347809 Shortlisted 26 Sonam Phuntsho Male 10203000926 17327957 Shortlisted 27 Sonam Tobgay Male 10204001081 17704691 Shortlisted 28 Tshering