0268D98d499c00a44e5d919f5d
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Table 1: Adhesion Genes Data Set
Supplementary Table 1: Adhesion genes data set PROBE Entrez Gene ID Celera Gene ID Gene_Symbol Gene_Name 160832 1 hCG201364.3 A1BG alpha-1-B glycoprotein 223658 1 hCG201364.3 A1BG alpha-1-B glycoprotein 212988 102 hCG40040.3 ADAM10 ADAM metallopeptidase domain 10 133411 4185 hCG28232.2 ADAM11 ADAM metallopeptidase domain 11 110695 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 195222 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 165344 8751 hCG20021.3 ADAM15 ADAM metallopeptidase domain 15 (metargidin) 189065 6868 null ADAM17 ADAM metallopeptidase domain 17 (tumor necrosis factor, alpha, converting enzyme) 108119 8728 hCG15398.4 ADAM19 ADAM metallopeptidase domain 19 (meltrin beta) 117763 8748 hCG20675.3 ADAM20 ADAM metallopeptidase domain 20 126448 8747 hCG1785634.2 ADAM21 ADAM metallopeptidase domain 21 208981 8747 hCG1785634.2|hCG2042897 ADAM21 ADAM metallopeptidase domain 21 180903 53616 hCG17212.4 ADAM22 ADAM metallopeptidase domain 22 177272 8745 hCG1811623.1 ADAM23 ADAM metallopeptidase domain 23 102384 10863 hCG1818505.1 ADAM28 ADAM metallopeptidase domain 28 119968 11086 hCG1786734.2 ADAM29 ADAM metallopeptidase domain 29 205542 11085 hCG1997196.1 ADAM30 ADAM metallopeptidase domain 30 148417 80332 hCG39255.4 ADAM33 ADAM metallopeptidase domain 33 140492 8756 hCG1789002.2 ADAM7 ADAM metallopeptidase domain 7 122603 101 hCG1816947.1 ADAM8 ADAM metallopeptidase domain 8 183965 8754 hCG1996391 ADAM9 ADAM metallopeptidase domain 9 (meltrin gamma) 129974 27299 hCG15447.3 ADAMDEC1 ADAM-like, -

CD Markers Are Routinely Used for the Immunophenotyping of Cells
ptglab.com 1 CD MARKER ANTIBODIES www.ptglab.com Introduction The cluster of differentiation (abbreviated as CD) is a protocol used for the identification and investigation of cell surface molecules. So-called CD markers are routinely used for the immunophenotyping of cells. Despite this use, they are not limited to roles in the immune system and perform a variety of roles in cell differentiation, adhesion, migration, blood clotting, gamete fertilization, amino acid transport and apoptosis, among many others. As such, Proteintech’s mini catalog featuring its antibodies targeting CD markers is applicable to a wide range of research disciplines. PRODUCT FOCUS PECAM1 Platelet endothelial cell adhesion of blood vessels – making up a large portion molecule-1 (PECAM1), also known as cluster of its intracellular junctions. PECAM-1 is also CD Number of differentiation 31 (CD31), is a member of present on the surface of hematopoietic the immunoglobulin gene superfamily of cell cells and immune cells including platelets, CD31 adhesion molecules. It is highly expressed monocytes, neutrophils, natural killer cells, on the surface of the endothelium – the thin megakaryocytes and some types of T-cell. Catalog Number layer of endothelial cells lining the interior 11256-1-AP Type Rabbit Polyclonal Applications ELISA, FC, IF, IHC, IP, WB 16 Publications Immunohistochemical of paraffin-embedded Figure 1: Immunofluorescence staining human hepatocirrhosis using PECAM1, CD31 of PECAM1 (11256-1-AP), Alexa 488 goat antibody (11265-1-AP) at a dilution of 1:50 anti-rabbit (green), and smooth muscle KD/KO Validated (40x objective). alpha-actin (red), courtesy of Nicola Smart. PECAM1: Customer Testimonial Nicola Smart, a cardiovascular researcher “As you can see [the immunostaining] is and a group leader at the University of extremely clean and specific [and] displays Oxford, has said of the PECAM1 antibody strong intercellular junction expression, (11265-1-AP) that it “worked beautifully as expected for a cell adhesion molecule.” on every occasion I’ve tried it.” Proteintech thanks Dr. -
HCC and Cancer Mutated Genes Summarized in the Literature Gene Symbol Gene Name References*
HCC and cancer mutated genes summarized in the literature Gene symbol Gene name References* A2M Alpha-2-macroglobulin (4) ABL1 c-abl oncogene 1, receptor tyrosine kinase (4,5,22) ACBD7 Acyl-Coenzyme A binding domain containing 7 (23) ACTL6A Actin-like 6A (4,5) ACTL6B Actin-like 6B (4) ACVR1B Activin A receptor, type IB (21,22) ACVR2A Activin A receptor, type IIA (4,21) ADAM10 ADAM metallopeptidase domain 10 (5) ADAMTS9 ADAM metallopeptidase with thrombospondin type 1 motif, 9 (4) ADCY2 Adenylate cyclase 2 (brain) (26) AJUBA Ajuba LIM protein (21) AKAP9 A kinase (PRKA) anchor protein (yotiao) 9 (4) Akt AKT serine/threonine kinase (28) AKT1 v-akt murine thymoma viral oncogene homolog 1 (5,21,22) AKT2 v-akt murine thymoma viral oncogene homolog 2 (4) ALB Albumin (4) ALK Anaplastic lymphoma receptor tyrosine kinase (22) AMPH Amphiphysin (24) ANK3 Ankyrin 3, node of Ranvier (ankyrin G) (4) ANKRD12 Ankyrin repeat domain 12 (4) ANO1 Anoctamin 1, calcium activated chloride channel (4) APC Adenomatous polyposis coli (4,5,21,22,25,28) APOB Apolipoprotein B [including Ag(x) antigen] (4) AR Androgen receptor (5,21-23) ARAP1 ArfGAP with RhoGAP domain, ankyrin repeat and PH domain 1 (4) ARHGAP35 Rho GTPase activating protein 35 (21) ARID1A AT rich interactive domain 1A (SWI-like) (4,5,21,22,24,25,27,28) ARID1B AT rich interactive domain 1B (SWI1-like) (4,5,22) ARID2 AT rich interactive domain 2 (ARID, RFX-like) (4,5,22,24,25,27,28) ARID4A AT rich interactive domain 4A (RBP1-like) (28) ARID5B AT rich interactive domain 5B (MRF1-like) (21) ASPM Asp (abnormal -

Anti-CD18 / LFA1 Beta Antibody (ARG41484)
Product datasheet [email protected] ARG41484 Package: 100 μl anti-CD18 / LFA1 beta antibody Store at: -20°C Summary Product Description Rabbit Polyclonal antibody recognizes CD18 / LFA1 beta Tested Reactivity Hu, Ms, Rat Tested Application ICC/IF, IHC-P, WB Host Rabbit Clonality Polyclonal Isotype IgG Target Name CD18 / LFA1 beta Antigen Species Human Immunogen Recombinant protein of Human CD18 / LFA1 beta. Conjugation Un-conjugated Alternate Names MF17; LAD; CD antigen CD18; MFI7; MAC-1; Cell surface adhesion glycoproteins LFA-1/CR3/p150,95 subunit beta; LCAMB; Integrin beta-2; Complement receptor C3 subunit beta; LFA-1; CD18 Application Instructions Application table Application Dilution ICC/IF 1:50 - 1:200 IHC-P 1:50 - 1:200 WB 1:500 - 1:2000 Application Note * The dilutions indicate recommended starting dilutions and the optimal dilutions or concentrations should be determined by the scientist. Positive Control Mouse thymus Calculated Mw 85 kDa Observed Size ~ 98 kDa Properties Form Liquid Purification Affinity purified. Buffer PBS (pH 7.3), 0.02% Sodium azide and 50% Glycerol. Preservative 0.02% Sodium azide Stabilizer 50% Glycerol Storage instruction For continuous use, store undiluted antibody at 2-8°C for up to a week. For long-term storage, aliquot and store at -20°C. Storage in frost free freezers is not recommended. Avoid repeated freeze/thaw www.arigobio.com 1/3 cycles. Suggest spin the vial prior to opening. The antibody solution should be gently mixed before use. Note For laboratory research only, not for drug, diagnostic or other use. Bioinformation Gene Symbol ITGB2 Gene Full Name integrin, beta 2 (complement component 3 receptor 3 and 4 subunit) Background This gene encodes an integrin beta chain, which combines with multiple different alpha chains to form different integrin heterodimers. -
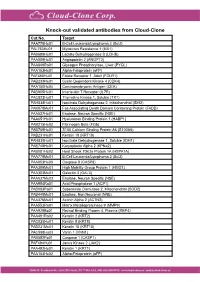
Knock-Out Validated Antibodies from Cloud-Clone Cat.No
Knock-out validated antibodies from Cloud-Clone Cat.No. Target PAA778Hu01 B-Cell Leukemia/Lymphoma 2 (Bcl2) PAL763Hu01 Myxovirus Resistance 1 (MX1) PAB698Hu01 Lactate Dehydrogenase B (LDHB) PAA009Hu01 Angiopoietin 2 (ANGPT2) PAA849Ra01 Glycogen Phosphorylase, Liver (PYGL) PAA153Hu01 Alpha-Fetoprotein (aFP) PAF460Hu01 Folate Receptor 1, Adult (FOLR1) PAB233Hu01 Cyclin Dependent Kinase 4 (CDK4) PAA150Hu04 Carcinoembryonic Antigen (CEA) PAB905Hu01 Interleukin 7 Receptor (IL7R) PAC823Hu01 Thymidine Kinase 1, Soluble (TK1) PAH838Hu01 Isocitrate Dehydrogenase 2, mitochondrial (IDH2) PAK078Mu01 Fas Associating Death Domain Containing Protein (FADD) PAA537Hu01 Enolase, Neuron Specific (NSE) PAA651Hu01 Hyaluronan Binding Protein 1 (HABP1) PAB215Hu02 Fibrinogen Beta (FGb) PAB769Hu01 S100 Calcium Binding Protein A6 (S100A6) PAB231Hu01 Keratin 18 (KRT18) PAH839Hu01 Isocitrate Dehydrogenase 1, Soluble (IDH1) PAE748Hu01 Karyopherin Alpha 2 (KPNa2) PAB081Hu02 Heat Shock 70kDa Protein 1A (HSPA1A) PAA778Mu01 B-Cell Leukemia/Lymphoma 2 (Bcl2) PAA853Hu03 Caspase 8 (CASP8) PAA399Mu01 High Mobility Group Protein 1 (HMG1) PAA303Mu01 Galectin 3 (GAL3) PAA537Mu02 Enolase, Neuron Specific (NSE) PAA994Ra01 Acid Phosphatase 1 (ACP1) PAB083Ra01 Superoxide Dismutase 2, Mitochondrial (SOD2) PAB449Mu01 Enolase, Non Neuronal (NNE) PAA376Mu01 Actinin Alpha 2 (ACTN2) PAA553Ra01 Matrix Metalloproteinase 9 (MMP9) PAA929Bo01 Retinol Binding Protein 4, Plasma (RBP4) PAA491Ra02 Keratin 2 (KRT2) PAC025Hu01 Keratin 8 (KRT8) PAB231Mu01 Keratin 18 (KRT18) PAC598Hu03 Vanin 1 (VNN1) -

Supp Table 6.Pdf
Supplementary Table 6. Processes associated to the 2037 SCL candidate target genes ID Symbol Entrez Gene Name Process NM_178114 AMIGO2 adhesion molecule with Ig-like domain 2 adhesion NM_033474 ARVCF armadillo repeat gene deletes in velocardiofacial syndrome adhesion NM_027060 BTBD9 BTB (POZ) domain containing 9 adhesion NM_001039149 CD226 CD226 molecule adhesion NM_010581 CD47 CD47 molecule adhesion NM_023370 CDH23 cadherin-like 23 adhesion NM_207298 CERCAM cerebral endothelial cell adhesion molecule adhesion NM_021719 CLDN15 claudin 15 adhesion NM_009902 CLDN3 claudin 3 adhesion NM_008779 CNTN3 contactin 3 (plasmacytoma associated) adhesion NM_015734 COL5A1 collagen, type V, alpha 1 adhesion NM_007803 CTTN cortactin adhesion NM_009142 CX3CL1 chemokine (C-X3-C motif) ligand 1 adhesion NM_031174 DSCAM Down syndrome cell adhesion molecule adhesion NM_145158 EMILIN2 elastin microfibril interfacer 2 adhesion NM_001081286 FAT1 FAT tumor suppressor homolog 1 (Drosophila) adhesion NM_001080814 FAT3 FAT tumor suppressor homolog 3 (Drosophila) adhesion NM_153795 FERMT3 fermitin family homolog 3 (Drosophila) adhesion NM_010494 ICAM2 intercellular adhesion molecule 2 adhesion NM_023892 ICAM4 (includes EG:3386) intercellular adhesion molecule 4 (Landsteiner-Wiener blood group)adhesion NM_001001979 MEGF10 multiple EGF-like-domains 10 adhesion NM_172522 MEGF11 multiple EGF-like-domains 11 adhesion NM_010739 MUC13 mucin 13, cell surface associated adhesion NM_013610 NINJ1 ninjurin 1 adhesion NM_016718 NINJ2 ninjurin 2 adhesion NM_172932 NLGN3 neuroligin -

AUSTRALIAN PATENT OFFICE (11) Application No. AU 199875933 B2
(12) PATENT (11) Application No. AU 199875933 B2 (19) AUSTRALIAN PATENT OFFICE (10) Patent No. 742342 (54) Title Nucleic acid arrays (51)7 International Patent Classification(s) C12Q001/68 C07H 021/04 C07H 021/02 C12P 019/34 (21) Application No: 199875933 (22) Application Date: 1998.05.21 (87) WIPO No: WO98/53103 (30) Priority Data (31) Number (32) Date (33) Country 08/859998 1997.05.21 US 09/053375 1998.03.31 US (43) Publication Date : 1998.12.11 (43) Publication Journal Date : 1999.02.04 (44) Accepted Journal Date : 2001.12.20 (71) Applicant(s) Clontech Laboratories, Inc. (72) Inventor(s) Alex Chenchik; George Jokhadze; Robert Bibilashvilli (74) Agent/Attorney F.B. RICE and CO.,139 Rathdowne Street,CARLTON VIC 3053 (56) Related Art PROC NATL ACAD SCI USA 93,10614-9 ANCEL BIOCHEM 216,299-304 CRENE 156,207-13 OPI DAtE 11/12/98 APPLN. ID 75933/98 AOJP DATE 04/02/99 PCT NUMBER PCT/US98/10561 IIIIIIIUIIIIIIIIIIIIIIIIIIIII AU9875933 .PCT) (51) International Patent Classification 6 ; (11) International Publication Number: WO 98/53103 C12Q 1/68, C12P 19/34, C07H 2UO2, Al 21/04 (43) International Publication Date: 26 November 1998 (26.11.98) (21) International Application Number: PCT/US98/10561 (81) Designated States: AL, AM, AT, AU, AZ, BA, BB, BG, BR, BY, CA, CH, CN, CU, CZ, DE, DK, EE, ES, FI, GB, GE, (22) International Filing Date: 21 May 1998 (21.05.98) GH, GM, GW, HU, ID, IL, IS, JP, KE, KG, KP, KR, KZ, LC, LK, LR, LS, LT, LU, LV, MD, MG, MK, MN, MW, MX, NO, NZ, PL, PT, RO, RU, SD, SE, SG, SI, SK, SL, (30) Priority Data: TJ, TM, TR, TT, UA, UG, US, UZ, VN, YU, ZW, ARIPO 08/859,998 21 May 1997 (21.05.97) US patent (GH, GM, KE, LS, MW, SD, SZ, UG, ZW), Eurasian 09/053,375 31 March 1998 (31.03.98) US patent (AM, AZ, BY, KG, KZ, MD, RU, TJ, TM), European patent (AT, BE, CH, CY, DE, DK, ES, Fl, FR, GB, GR, IE, IT, LU, MC, NL, PT, SE), OAPI patent (BF, BJ, CF, (71) Applicant (for all designated States except US): CLONTECH CG, CI, CM, GA, GN, ML, MR, NE, SN, TD, TG). -

1199SEIU Benefit Funds
1199SEIU Benefit Funds The following codes are under management for members who have health benefits covered by 1199SEIU Benefit Funds, administered by eviCore healthcare. Commercial Effective 5/1/14 Claims Policies Effective 7/1/14 Procedure Code Full Description How Code is Managed Effective Date Termination Date Human Platelet Antigen 1 genotyping (HPA-1), ITGB3 (integrin, beta 3 [platelet glycoprotein IIIa], 81105 antigen CD61 [GPIIIa]) (eg, neonatal alloimmune thrombocytopenia [NAIT], post-transfusion purpura), Claim Policies Apply 01/01/18 None gene analysis, common variant, HPA-1a/b (L33P) Human Platelet Antigen 2 genotyping (HPA-2), GP1BA (glycoprotein Ib [platelet], alpha polypeptide 81106 [GPIba]) (eg, neonatal alloimmune thrombocytopenia [NAIT], post-transfusion purpura), gene Claim Policies Apply 01/01/18 None analysis, common variant, HPA-2a/b (T145M) Human Platelet Antigen 3 genotyping (HPA-3), ITGA2B (integrin, alpha 2b [platelet glycoprotein IIb of 81107 IIb/IIIa complex], antigen CD41 [GPIIb]) (eg, neonatal alloimmune thrombocytopenia [NAIT], post- Claim Policies Apply 01/01/18 None transfusion purpura), gene analysis, common variant, HPA-3a/b (I843S) Human Platelet Antigen 4 genotyping (HPA-4), ITGB3 (integrin, beta 3 [platelet glycoprotein IIIa], 81108 antigen CD61 [GPIIIa]) (eg, neonatal alloimmune thrombocytopenia [NAIT], post-transfusion purpura), Claim Policies Apply 01/01/18 None gene analysis, common variant, HPA-4a/b (R143Q) Human Platelet Antigen 5 genotyping (HPA-5), ITGA2 (integrin, alpha 2 [CD49B, alpha 2 -

New Mesh Headings for 2018 Single Column After Cutover
New MeSH Headings for 2018 Listed in alphabetical order with Heading, Scope Note, Annotation (AN), and Tree Locations 2-Hydroxypropyl-beta-cyclodextrin Derivative of beta-cyclodextrin that is used as an excipient for steroid drugs and as a lipid chelator. Tree locations: beta-Cyclodextrins D04.345.103.333.500 D09.301.915.400.375.333.500 D09.698.365.855.400.375.333.500 AAA Domain An approximately 250 amino acid domain common to AAA ATPases and AAA Proteins. It consists of a highly conserved N-terminal P-Loop ATPase subdomain with an alpha-beta-alpha conformation, and a less-conserved C- terminal subdomain with an all alpha conformation. The N-terminal subdomain includes Walker A and Walker B motifs which function in ATP binding and hydrolysis. Tree locations: Amino Acid Motifs G02.111.570.820.709.275.500.913 AAA Proteins A large, highly conserved and functionally diverse superfamily of NTPases and nucleotide-binding proteins that are characterized by a conserved 200 to 250 amino acid nucleotide-binding and catalytic domain, the AAA+ module. They assemble into hexameric ring complexes that function in the energy-dependent remodeling of macromolecules. Members include ATPASES ASSOCIATED WITH DIVERSE CELLULAR ACTIVITIES. Tree locations: Acid Anhydride Hydrolases D08.811.277.040.013 Carrier Proteins D12.776.157.025 Abuse-Deterrent Formulations Drug formulations or delivery systems intended to discourage the abuse of CONTROLLED SUBSTANCES. These may include physical barriers to prevent chewing or crushing the drug; chemical barriers that prevent extraction of psychoactive ingredients; agonist-antagonist combinations to reduce euphoria associated with abuse; aversion, where controlled substances are combined with others that will produce an unpleasant effect if the patient manipulates the dosage form or exceeds the recommended dose; delivery systems that are resistant to abuse such as implants; or combinations of these methods. -

Product Datasheet Integrin Alpha 2B/CD41
Product Datasheet Integrin alpha 2b/CD41 Antibody NBP1-84581 Unit Size: 0.1 ml Store at 4C short term. Aliquot and store at -20C long term. Avoid freeze-thaw cycles. Protocols, Publications, Related Products, Reviews, Research Tools and Images at: www.novusbio.com/NBP1-84581 Updated 7/27/2021 v.20.1 Earn rewards for product reviews and publications. Submit a publication at www.novusbio.com/publications Submit a review at www.novusbio.com/reviews/destination/NBP1-84581 Page 1 of 4 v.20.1 Updated 7/27/2021 NBP1-84581 Integrin alpha 2b/CD41 Antibody Product Information Unit Size 0.1 ml Concentration Concentrations vary lot to lot. See vial label for concentration. If unlisted please contact technical services. Storage Store at 4C short term. Aliquot and store at -20C long term. Avoid freeze-thaw cycles. Clonality Polyclonal Preservative 0.02% Sodium Azide Isotype IgG Purity Immunogen affinity purified Buffer PBS (pH 7.2) and 40% Glycerol Product Description Host Rabbit Gene ID 3674 Gene Symbol ITGA2B Species Human Reactivity Notes Immunogen displays the following percentage of sequence identity for non- tested species: Mouse (85%), Rat (82%) Immunogen This antibody was developed against Recombinant Protein corresponding to amino acids: GATGHNIPQKLSLNAELQLDRQKPRQGRRVLLLGSQQAGTTLNLDLGGKHSPI CHTTMAFLRDEADFRDKLSPIVLSLNVSLPPTEAGMAPAV Product Application Details Applications Western Blot, Simple Western, Immunohistochemistry, Immunohistochemistry- Paraffin Recommended Dilutions Western Blot 0.04-0.4 ug/ml, Simple Western 1:25, Immunohistochemistry 1:2500 - 1:5000, Immunohistochemistry-Paraffin 1:2500 - 1:5000 Application Notes For IHC-Paraffin, HIER pH 6 retrieval is recommended. In Simple Western only 10-15 uL of the recommended dilution is used per data point. -

Integrin and Gene Network Analysis Reveals That ITGA5 and ITGB1 Are Prognostic in Non-Small-Cell Lung Cancer
Journal name: OncoTargets and Therapy Article Designation: Original Research Year: 2016 Volume: 9 OncoTargets and Therapy Dovepress Running head verso: Zheng et al Running head recto: ITGA5 and ITGB1 are prognostic in NSCLC open access to scientific and medical research DOI: http://dx.doi.org/10.2147/OTT.S91796 Open Access Full Text Article ORIGINAL RESEARCH Integrin and gene network analysis reveals that ITGA5 and ITGB1 are prognostic in non-small-cell lung cancer Weiqi Zheng Background: Integrin expression has been identified as a prognostic factor in non-small-cell Caihui Jiang lung cancer (NSCLC). This study was aimed at determining the predictive ability of integrins Ruifeng Li and associated genes identified within the molecular network. Patients and methods: A total of 959 patients with NSCLC from The Cancer Genome Atlas Department of Radiation Oncology, Guangqian Hospital, Quanzhou, Fujian, cohorts were enrolled in this study. The expression profile of integrins and related genes were People’s Republic of China obtained from The Cancer Genome Atlas RNAseq database. Clinicopathological characteristics, including age, sex, smoking history, stage, histological subtype, neoadjuvant therapy, radiation therapy, and overall survival (OS), were collected. Cox proportional hazards regression models as well as Kaplan–Meier curves were used to assess the relative factors. Results: In the univariate Cox regression model, ITGA1, ITGA5, ITGA6, ITGB1, ITGB4, and ITGA11 were predictive of NSCLC prognosis. After adjusting for clinical factors, ITGA5 (odds ratio =1.17, 95% confidence interval: 1.05–1.31) andITGB1 (odds ratio =1.31, 95% confidence interval: 1.10–1.55) remained statistically significant. In the gene cluster network analysis, PLAUR, ILK, SPP1, PXN, and CD9, all associated with ITGA5 and ITGB1, were identified as independent predictive factors of OS in NSCLC. -

Development and Validation of Tumor-Educated Blood Platelets Integrin Alpha 2B
Int. J. Biol. Sci. 2019, Vol. 15 1977 Ivyspring International Publisher International Journal of Biological Sciences 2019; 15(9): 1977-1992. doi: 10.7150/ijbs.36284 Research Paper Development and Validation of Tumor-educated Blood Platelets Integrin Alpha 2b (ITGA2B) RNA for Diagnosis and Prognosis of Non-small-cell Lung Cancer through RNA-seq Shan Xing1#, Tao Zeng2#, Ning Xue3#, Yi He1, Yan-zhen Lai1, Hui-lan Li1, Qi Huang1, Shu-lin Chen1, 1 Wan-li Liu 1. Department of Clinical Laboratory, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Sun Yat-sen University Cancer Center, Guangzhou 510060, P. R. China 2. Department of Clinical Laboratory, The Sixth Affiliated Hospital, Sun Yat-sen University, Guangzhou 510060, P. R. China 3. Department of Clinical Laboratory, Affiliated Tumor Hospital of Zhengzhou University, Henan Tumor Hospital, Zhengzhou 450100, P. R. China # Equal contributors Corresponding authors: Shu-lin Chen: [email protected]; Wan-li Liu: Department of Clinical Laboratory, Sun Yat-Sen University Cancer Center, 651 Dongfeng Road East, Guangzhou 510060, Guangdong Province, China. Email: [email protected]; Telephone: +86-020-87343196; Fax: +86-020-87343196 © The author(s). This is an open access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/). See http://ivyspring.com/terms for full terms and conditions. Received: 2019.05.03; Accepted: 2019.06.17; Published: 2019.07.24 Abstract Background: Currently, there are no molecular biomarkers for the early detection of non-small-cell lung cancer (NSCLC). This study focused on identifying RNAs found on tumor-educated blood platelets (TEPs) for detecting stage I NSCLC.