The Investigation of Highly Pathogenic Viruses in Kazakhstan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Potential Influence of World Heritage Sites Over the Global Citizenship Education in the Republic of Kazakhstan
POTENTIAL INFLUENCE OF WORLD HERITAGE SITES OVER THE GLOBAL CITIZENSHIP EDUCATION IN THE REPUBLIC OF KAZAKHSTAN Manual for teachers of general secondary and high school education programmes National World Heritage Committee under the jurisdiction of the National Commission of the Republic of Kazakhstan for UNESCO and ISESCO Almaty 2017 UDC 371.214 BBC 74.202 P 64 P 64 «Potential Influence of World Heritage Sites over the Global Citizenship Education in the Republic of Kazakhstan. Manual for teachers of general secondary and high school education programmes. K.M. Baipakov, D.A. Voyakin, M.E. Dikan, M.N. Massanov, E.A. Sarsenova, Z.N. Shaigozova. – Almaty: APCEIU, NWHC. 2017. Content ISBN 978-601-06-4672-8 Present publication is a manual for teachers for of general secondary and high school education programmes of the Republic of Kazakhstan and Central Asia. It aims to raise awareness of teachers and students on the issue of local cultural and natural heritage, and Global Citizenship Education 10 Cooperation between Kazakhstan and UNESCO Concept, and to introduce World Heritage and Global Citizenship Education topics to the general Baipakov K.M., Voyakin D.A., Massanov M.N. secondary and high school education programmes of Kazakhstan. For Kazakhstan and Central Asian, it is a first attempt to understand the potential contribution of UNESCO World Heritage Sites 28 World Heritage of Kazakhstan to the Global Citizenship Education. Baipakov K.M., Voyakin D.A., Massanov M.N. Disclaimer Global Citizenship Education While every effort have been made to ensure that the information contained herein is correct at 72 the time of publication, the authors shall not be held liable for any errors, omissions, inaccuracies Dikan M.E., Massanov M.N., Sarsenova E.A. -

Hymenoptera: Chalcidoidea: Pteromalidae)
ZOOSYSTEMATICA ROSSICA, 18(1): 73-82 3 July 2009 Review of Kazakhstan species of the genus Pachyneuron Walker, 1833 (Hymenoptera: Chalcidoidea: Pteromalidae) K.A. DZHANOKMEN K.A. Dzhanokmen, Institute of Zoology, Akademgorodok, 93 Al-Farabi Ave., Almaty 050060, Kazakhstan. Ten species of Pachyneuron are reported from Kazakhstan. Data on distribution and biology are reported for the first time for most of these species. A key to the species is provided. Key words: Hymenoptera, Pachyneuron, Kazakhstan INTRODUCTION Pachyneuron aphidis (Bouché, 1834) (Figs 1-4) Pachyneuron Walker, 1833 is a cosmo- politan genus. Members of the genus are Material examined. Kazakhstan: North Ka- mainly hyperparasites of Homoptera (Aphi- zakhstan Prov., 2 females, near town of Shchu- doidea, Coccoidea and Psylloidea) through chinsk, on Salix sp., 27 July 1976, D.K.; Akmolinsk Hymenoptera (Ichneumonoidea: Braconi- Prov., 4 females, in the vicinity of Zhuravlevka vil- lage, from aphids (unknown species), July 1974, dae, Aphidiinae; Chalcidoidea: Encyrtidae, S.N.; South Kazakhstan Prov., 60 females, 47 males, Aphelinidae), or primary and secondary town of Dzhetysay, from Pterochloroides persicae parasites of the predators of aphidopha- Chol. (Aphididae, Lachninae) on Persica vulgaris gous Diptera (Syrphidae, Chamaemyidae), Mill., 28 Oct. 1977, F.M.; 1 female, same locality, Coleoptera (Coccinellidae), Neuroptera from Aphis fabae Scopoli (Aphididae, Aphidinae) (Chrysopidae), and also of eggs of Lepi- on Rumex confertus Willd., 24 Sept. 1978, F.M.; 3 doptera (Graham, 1969; Bouček, 1965, females, 2 males, same locality, from Hyalopterus 1970, 1977, 1988; Dzhanokmen, 1978, 1984; pruni (Geoffroy) (Aphididae, Aphidinae) on Ar- meniaca vulgaris Lam., 29 May 1976, F.M.; 2 fe- Gafarov, 1979; Noyes, 1998; Gibson, 2001). -
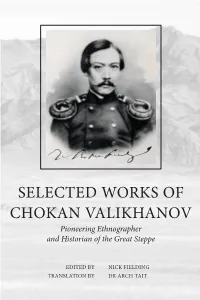
Selected Works of Chokan Valikhanov Selected Works of Chokan Valikhanov
SELECTED WORKS OF CHOKAN VALIKHANOV CHOKAN OF WORKS SELECTED SELECTED WORKS OF CHOKAN VALIKHANOV Pioneering Ethnographer and Historian of the Great Steppe When Chokan Valikhanov died of tuberculosis in 1865, aged only 29, the Russian academician Nikolai Veselovsky described his short life as ‘a meteor flashing across the field of oriental studies’. Set against his remarkable output of official reports, articles and research into the history, culture and ethnology of Central Asia, and more important, his Kazakh people, it remains an entirely appropriate accolade. Born in 1835 into a wealthy and powerful Kazakh clan, he was one of the first ‘people of the steppe’ to receive a Russian education and military training. Soon after graduating from Siberian Cadet Corps at Omsk, he was taking part in reconnaissance missions deep into regions of Central Asia that had seldom been visited by outsiders. His famous mission to Kashgar in Chinese Turkestan, which began in June 1858 and lasted for more than a year, saw him in disguise as a Tashkent mer- chant, risking his life to gather vital information not just on current events, but also on the ethnic make-up, geography, flora and fauna of this unknown region. Journeys to Kuldzha, to Issyk-Kol and to other remote and unmapped places quickly established his reputation, even though he al- ways remained inorodets – an outsider to the Russian establishment. Nonetheless, he was elected to membership of the Imperial Russian Geographical Society and spent time in St Petersburg, where he was given a private audience by the Tsar. Wherever he went he made his mark, striking up strong and lasting friendships with the likes of the great Russian explorer and geographer Pyotr Petrovich Semyonov-Tian-Shansky and the writer Fyodor Dostoyevsky. -

Almaty–Issyk-Kul Alternative Road Economic Impact Assessment
Almaty–Issyk-Kul Alternative Road Economic Impact Assessment Almaty, a vibrant metropolis in Kazakhstan, is only kilometers away from lake Issyk-Kul in the Kyrgyz Republic, renowned for its mountains and moderate summers. However, the two destinations are separated by two magnificent mountain ranges. To bypass these mountains, the existing road stretches over kilometers, leading to long travel times. This economic impact assessment analyzes what impact a more direct road between the two destinations would have for tourism and economic development in both Kazakhstan and the Kyrgyz Republic. The report provides economically viable solutions that, within a supportive policy environment, would lead to strong economic development within the region. About Almaty–Bishkek Economic Corridor The Almaty–Bishkek Economic Corridor (ABEC) is the pilot economic corridor under the Central Asia Regional Economic Cooperation (CAREC) Program. The motivation for ABEC is that Almaty and Bishkek can achieve far more together than either can achieve alone. The two cities are only kilometers apart with relatively high economic density concentrated in services in the cities and agriculture in their hinterlands. Both Kazakhstan and the Kyrgyz Republic have acceded to the Eurasian Economic Union and the World Trade Organization. CAREC corridors and Belt and Road Initiative routes cross ABEC. The historic Silk Route, mountain ranges, and Lake lssyk-Kul underline the potential for tourism. But trade, especially in agricultural goods and services, between the two countries is below potential, and the region does not yet benefit from being one economic space. About the Central Asia Regional Economic Cooperation Program The Central Asia Regional Economic Cooperation (CAREC) Program is a partnership of member countries and development partners working together to promote development through cooperation, leading to accelerated economic growth and poverty reduction. -

Ecosystem Service Assessment of the Ili Delta, Kazakhstan Niels Thevs
Ecosystem service assessment of the Ili Delta, Kazakhstan Niels Thevs, Volker Beckmann, Sabir Nurtazin, Ruslan Salmuzauli, Azim Baibaysov, Altyn Akimalieva, Elisabeth A. A. Baranoeski, Thea L. Schäpe, Helena Röttgers, Nikita Tychkov 1. Territorial and geographical location Ili Delta, Kazakhstan Almatinskaya Oblast (province), Bakanas Rayon (county) The Ili Delta is part of the Ramsar Site Ile River Delta and South Lake Balkhash Ramsar Site 2. Natural and geographic data Basic geographical data: location between 45° N and 46° N as well as 74° E and 75.5° E. Fig. 1: Map of the Ili-Balkhash Basin (Imentai et al., 2015). Natural areas: The Ramsar Site Ile River Delta and South Lake Balkhash Ramsar Site comprises wetlands and meadow vegetation (the modern delta), ancient river terraces that now harbour Saxaul and Tamarx shrub vegetation, and the southern coast line of the western part of Lake Balkhash. Most ecosystem services can be attributed to the wetlands and meadow vegetation. Therefore, this study focusses on the modern delta with its wetlands and meadows. During this study, a land cover map was created through classification of Rapid Eye Satellite images from the year 2014. The land cover classes relevant for this study were: water bodies in the delta, dense reed (total vegetation more than 70%), and open reed and shrub vegetation (vegetation cover of reed 20- 70% and vegetation cover of shrubs and trees more than 70%). The land cover class dense reed was further split into submerged dense reed and non-submerged dense reed by applying a threshold to the short wave infrared channel of a Landsat satellite image from 4 April 2015. -

Итоги SE-2019 Almaty Eng.Cdr
POST - REPORT SuluExpoSuluExpo 20192019 Almaty The 17th INTERNATIONAL EXHIBITION FOR BEAUTY INDUSTRY 4-6 April 2019 EC «АТАКЕНТ», Almaty city, Каzakhstan ОРГАНИЗАТОРЫ: SuluExpo K A Z A K H S T A N www.suluexpo.kz POST - REPORT www.suluexpo.kz This year (4th-6th of April), the beauty exhibition - “SuluExpo” crossed its 17th summer line. Our organizers achieved the significant result when beauty exhibition was recognized and talked not only in Kazakhstan, but also in abroad. Maximize all promotional opportunities, organizers managed to gather in one place more than 70 real-exhibitors including Germany, Turkey, Korea, Russia, Kyrgyzstan, Kazakhstan and a collective exposition of 8 Polish companies! The exhibition was represented by such sections as cosmetology and aesthetic medicine, nail service, decorative cosmetics, hairdressing, face and body care cosmetics, etc. The “SuluExpo” exhibition expands the geography of international exhibitors annually. So this year a collective exposition of 8 leading Polish manufacturers was presented. Under the leadership of JSC Polish Investment and Trade Agency. The exposition included: “Inter Fragrances” - specializes in the production of hair care products of the brand Seboradin; “BIES” - one of the largest and most significant perfume brands in Poland; “Blux Cosmetics” - a manufacturer of high-quality cosmetics and household chemicals; Eveline - a manufacturer of body care cosmetics; Glov is a manufacturer of a unique makeup remover; "Herla" - a leading manufacturer of professional cosmetics for face and body care, premium; “LaQell” - a manufacturer of high quality nail polishes; “Miraculum” - development and sale of modern cosmetics for face and body skin care, perfumes, preparations for depilation and decorative cosmetics. -

A/HRC/13/23/Add.1 General Assembly
United Nations A/HRC/13/23/Add.1 General Assembly Distr.: General 1 February 2010 Original: English Human Rights Council Thirteenth session Agenda item 3 Promotion and Protection of all Human Rights, Civil, Political, Economic, Social and Cultural Rights, including the Right to Development Report of the independent expert on minority issues Addendum Mission to Kazakhstan* ** (6 to 15 July 2009) Summary Kazakhstan has approximately 130 different ethnic groups, many of which have lived on the territory of Kazakhstan for generations. Initiatives taken by the Government in the field of minority issues have undoubtedly helped to ensure stability and respect for diversity and minority rights. These initiatives have included important policies to help preserve minority languages, establish and fund cultural associations for the preservation of ethnic cultures and traditions and the establishment of consultative bodies, the most prominent of which is the Assembly of the People of Kazakhstan. The Assembly of the People, which plays a consultative or advisory role to the President, is a valuable national symbol of the recognition of minorities and the commitment of the State to the preservation of the cultural heritage of minorities. Nine seats in the lower house of Parliament are reserved for members chosen from the Assembly. However, the Assembly lacks the character of a legitimately representative body. Its membership is not constituted on a fully democratic basis and members are not, therefore, clearly accountable to their minority communities. * Late submission. ** The summary of the present report is being circulated in all official languages. The report itself, contained in the annex to the summary, is being circulated in the language of submission and in Russian only. -

Economic and Social Council
UNITED NATIONS E Economic and Social Distr. GENERAL Council TRANS/SC.1/AC.5/2002/1 28 March 2002 Original: ENGLISH ECONOMIC COMMISSION FOR EUROPE INLAND TRANSPORT COMMITTEE Working Party on Road Transport Ad hoc Meeting on the Implementation of the AGR (Eighteenth session, 10-11 June 2002 agenda item 4) CONSIDERATION OF PROPOSALS FOR AMENDMENTS TO ANNEX 1 OF THE AGR Transmitted by Kazakhstan The Ministry of Transport and Communications of the Republic of Kazakhstan, having reviewed the text of the European Agreement on Main International Traffic Arteries (AGR) in the light of amendments 1-8 to the original text, and also the updated version of the map of the international E road network, wishes to make the following observations. Kazakhstan’s Blueprint for road traffic development outlines six main transit corridors: 1. Tashkent - Shymkent - Taraz - Bishkek - Almaty - Khorgos; 2. Shymkent - Kyzylorda - Aktyubinsk - Uralsk - Samara; 3. Almaty - Karagandy - Astana - Petropavlovsk; 4. Astrakhan - Atyrau - Aktau - Turkmen frontier; 5. Omsk - Pavlodar - Semipalatinsk - Maikapshagai; 6. Astana - Kostanay - Chelyabinsk. GE.02- TRANS/SC.1/AC.5/2002/1 page 2 Accordingly, the following amendments and additions are proposed to annex I to the AGR and the draft map of the international road network: 1. E 40. After Kharkov extend as follows: … Lugansk - Volgograd - Astrakhan - Atyrau - Beineu - Kungrad - Nukus - Bukhara - Nawoy - Samarkand - Dzhizak - Tashkent - Shymkent - Taraz - Bishkek - Almaty - Sary-Ozek - Taldykorgan - Usharal - Taskesken - Ayaguz - Georgievka - Ust-Kamenogorsk - Leninogorsk - Ust-Kan. The Leninogorsk - Ust-Kan section should be indicated on the map. 2. E 38 should be extended to Shymkent. The Kyzylorda - Shymkent section should be assigned a dual number (E 123/E 38). -
Download File
The Ministry of culture and sports of the Republic of Kazakhstan State of conservation report the Republic of Kazakhstan "Silk Roads: the Routes Network of Chang’an-Tianshan Corridor (Kazakhstan, China, Kyrgyzstan): theTalgar, Koilyk, Karamergen, Aktobe, Kulan, Kostobe, Ornek sites and the Akyrtas archaeological complex (Kazakhstan territory) Astana, 2017 State of conservation report the Republic of Kazakhstan "Silk Roads: the Routes Network of Chang’an-Tianshan Corridor (Kazakhstan, China, Kyrgyzstan): the Talgar, Koilyk, Karamergen, Aktobe, Kulan, Kostobe, Ornek sites and the Akyrtas archaeological complex (Kazakhstan territory) 2017 2 TABLE OF CONTENTS No. Name page INTRODUCTION 4 I OVERALL STRATEGY OF PRESERVATION OF THE WORLD 6 CULTURAL HERITAGE PROPERTY IN THE REPUBLIC OF KAZAKHSTAN I.1 LEGISLATIVE AND ADMINISTRATIVE MEASURES 7 I.2 FINANCIAL MEASURES, RESEARCH AND TECHNICAL 7 STUDIES I.3 SPECIALIST TRAINING ACTIVITIES 8 II STATE OF CONSERVATION OF THE COMPONENTS IN 9 KAZAKHSTAN OF THE WORLD HERITAGE SITE "SILK ROADS: THE ROUTES NETWORK OF CHANG'AN-TIANSHAN CORRIDOR" II. 1 THE TALGAR SITE (S 01-KZ) 9 ANNEX I 13 PROTOKOL Ref. No. 21-5/05-1557 dated: 27.10.2016 of the visiting meeting on issue of the medieval ancient settlement "Talgar" Chairman: Deputy Prime Minister of the Republic of Kazakhstan I.N. Tasmagambetov (Russian and English) ANNEX II 1. Letter of deputy prime minister of the republic of Kazakhstan No. 15 20-55/1668 dd. September 1, 2016. (Russian and English) 2. Telephone message Ref. No. 11/И-13 dated: 24.10.2016 (Russian 17 and English) 3. Letter No.3968 dd. October 21, 2016 of Head of the Internal Policy 19 Department A. -

THE URBAN INSTITUTE 2100 M STREET,NW WASHINGTON, DC 20037 Maria C
THE URBAN INSTITUTE 2100 M STREET,NW WASHINGTON, DC 20037 Maria C. Andrade-Stern Direct Diaf (202)261 -5396 Senior Contract Administrator FAX: (202)728-0231 [email protected] October 15,2003 Mr. John Lord Contracting Officer USAlDlAlmaty C/OAmerican Embassy 97A Furmanov Street Almaty, Kazakhstan 480091 RE: Contract No. EEU-I-00-99-00015-00,TO No. 81 1 UI Project 06901-01 5,06901 -016,06901 -017, & 06901-01 8 Central Asian Republics Local Government lnitiative Phase II Quarterly Task Order Progress and Cost Report, July to September 2003 Dear Mr. Lord: Please find enclosed Quarterly Task Order Progress and Cost Report, July to September 2003, Central Asian Republics Local Government lnitiative Phase 11. This report is required by Sections F.5 and F.6 of our Local Government Assistance lnitiative Indefinite Quantity Contract. Please direct any technical questions to Mr. Charles Undeland, Chief of Party, at t996-312-66-04-28or e-mail at [email protected]. Questions of a contractual nature should be addressed to me at (202) 261-5396. Sincerely, Maria C. Andrade-Stern Enclosures cc: Ivan Apanasevich (CEN, ASIAIODT) Mike Keshishian (USAIDMI) Charles Undeland (KyrgyzstanlUI) USAlD Development Clearinghouse IAC Deliverables File (06901-01 5 to 018) IAC Chron File QUARTERLY TASK ORDER PROGRESS AND COST REPORT CENTRAL ASIAN REPUBLICS LOCAL GOVERNMENT INITIATIVE PHASE II JULY TO SEPTEMBER 2003 Prepared for Prepared by Charlie Undeland The Urban Institute Central Asian Republics Local Government Initiative Phase I1 United States Agency for International Development Contract No. EEU-I-00-99-00015-00,Task Order No. 81 1 THE URBAN INSTITUTE 2100 M Street, NW Washington, DC 20037 October 2003 (202) 833-7200 UI Project 06901-01 5,06901 -01 6, www.urban.org 06901-01 7 and 06901-01 8 TABLE OF CONTENTS MONTHLY REPORT FOR JULY 2003 ....................................................................................... -

Investor's Atlas 2006
INVESTOR’S ATLAS 2006 Investor’s ATLAS Contents Akmola Region ............................................................................................................................................................. 4 Aktobe Region .............................................................................................................................................................. 8 Almaty Region ............................................................................................................................................................ 12 Atyrau Region .............................................................................................................................................................. 17 Eastern Kazakhstan Region............................................................................................................................................. 20 Karaganda Region ........................................................................................................................................................ 24 Kostanai Region ........................................................................................................................................................... 28 Kyzylorda Region .......................................................................................................................................................... 31 Mangistau Region ........................................................................................................................................................ -

Annual Bulletin of Monitoring of the Climate State and Climate Change in Kazakhstan: 2018
Ministry of Ecology, Geology and Natural Resources of the RK Republican State Enterprise “Kazhydromet” Scientific Research Center ANNUAL BULLETIN OF MONITORING OF THE CLIMATE STATE AND CLIMATE CHANGE IN KAZAKHSTAN: 2018 ºС 2 1 0 -1 -2 -3 2011 1941 1948 1955 1962 1969 1976 1983 1990 1997 2004 2018 Astana, 2019 CONTENTS SUMMARY 3 INTRODUCTION 5 1 REVIEW OF GLOBAL CLIMATE CHANGE AND ITS STATUS IN 2017 8 2 AIR TEMPERATURE 10 2.1 Air temperature anomalies in Kazakhstan in 2018 11 2.2 The changes of the air temperatures observed in Kazakhstan 22 2.3 Tendencies in extremes of surface air temperature 29 3. PRECIPITATION 35 3.1 Anomalies of precipitation in Kazakhstan in 2018 35 3.2 Observed changes in precipitation in Kazakhstan 42 3.3 Trends in precipitation extremes 48 ANNEX 1 51 ANNEX 2 53 SUMMARY Features of climate in 2018 In general, for the globe, 2018 entered the top ten warmest years for the period of instrumental observations (1850-2018), taking 4th place. Global average temperature in 2018 was by 0,99 °C above the preindustrial level (1850-1900). New record values of the heat content in the upper layers of the ocean, as well as the continued increase in global mean sea level, have been established. A decrease in the extent of the Arctic and Antarctic sea ice was noted. In 2018, 74 tropical cyclones were registered, which significantly exceeds their long-term average number (63). Floods, extreme rainfall and extratropical storms have caused hundreds of human lives and the destruction of tens of thousands of homes.