Tafenoquine for Prevention of Malaria
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Stevelinkbjpauthors Reply
King’s Research Portal Link to publication record in King's Research Portal Citation for published version (APA): Stevelink, S., Jones, M. M., Greenberg, N., Rona, R. J., & Fear, N. T. (2019). Mental health outcomes at the end of the British involvement in the Iraq and Afghanistan conflicts: a cohort study - Authors' reply. British Journal of Psychiatry. Citing this paper Please note that where the full-text provided on King's Research Portal is the Author Accepted Manuscript or Post-Print version this may differ from the final Published version. If citing, it is advised that you check and use the publisher's definitive version for pagination, volume/issue, and date of publication details. And where the final published version is provided on the Research Portal, if citing you are again advised to check the publisher's website for any subsequent corrections. General rights Copyright and moral rights for the publications made accessible in the Research Portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognize and abide by the legal requirements associated with these rights. •Users may download and print one copy of any publication from the Research Portal for the purpose of private study or research. •You may not further distribute the material or use it for any profit-making activity or commercial gain •You may freely distribute the URL identifying the publication in the Research Portal Take down policy If you believe that this document breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. -

Rediscovery of Fexinidazole
New Drugs against Trypanosomatid Parasites: Rediscovery of Fexinidazole INAUGURALDISSERTATION zur Erlangung der Würde eines Doktors der Philosophie vorgelegt der Philosophisch-Naturwissenschaftlichen Fakultät der Universität Basel von Marcel Kaiser aus Obermumpf, Aargau Basel, 2014 Originaldokument gespeichert auf dem Dokumentenserver der Universität Basel edoc.unibas.ch Dieses Werk ist unter dem Vertrag „Creative Commons Namensnennung-Keine kommerzielle Nutzung-Keine Bearbeitung 3.0 Schweiz“ (CC BY-NC-ND 3.0 CH) lizenziert. Die vollständige Lizenz kann unter creativecommons.org/licenses/by-nc-nd/3.0/ch/ eingesehen werden. 1 Genehmigt von der Philosophisch-Naturwissenschaftlichen Fakultät der Universität Basel auf Antrag von Prof. Reto Brun, Prof. Simon Croft Basel, den 10. Dezember 2013 Prof. Dr. Jörg Schibler, Dekan 2 3 Table of Contents Acknowledgement .............................................................................................. 5 Summary ............................................................................................................ 6 Zusammenfassung .............................................................................................. 8 CHAPTER 1: General introduction ................................................................. 10 CHAPTER 2: Fexinidazole - A New Oral Nitroimidazole Drug Candidate Entering Clinical Development for the Treatment of Sleeping Sickness ........ 26 CHAPTER 3: Anti-trypanosomal activity of Fexinidazole – A New Oral Nitroimidazole Drug Candidate for the Treatment -

Australian Public Assessment Report for Tafenoquine (As Succinate)
Australian Public Assessment Report for Tafenoquine (as succinate) Proprietary Product Name: Kozenis Sponsor: GlaxoSmithKline Australia Pty Ltd November 2018 Therapeutic Goods Administration About the Therapeutic Goods Administration (TGA) • The Therapeutic Goods Administration (TGA) is part of the Australian Government Department of Health and is responsible for regulating medicines and medical devices. • The TGA administers the Therapeutic Goods Act 1989 (the Act), applying a risk management approach designed to ensure therapeutic goods supplied in Australia meet acceptable standards of quality, safety and efficacy (performance) when necessary. • The work of the TGA is based on applying scientific and clinical expertise to decision- making, to ensure that the benefits to consumers outweigh any risks associated with the use of medicines and medical devices. • The TGA relies on the public, healthcare professionals and industry to report problems with medicines or medical devices. TGA investigates reports received by it to determine any necessary regulatory action. • To report a problem with a medicine or medical device, please see the information on the TGA website <https://www.tga.gov.au>. About AusPARs • An Australian Public Assessment Report (AusPAR) provides information about the evaluation of a prescription medicine and the considerations that led the TGA to approve or not approve a prescription medicine submission. • AusPARs are prepared and published by the TGA. • An AusPAR is prepared for submissions that relate to new chemical entities, generic medicines, major variations and extensions of indications. • An AusPAR is a static document; it provides information that relates to a submission at a particular point in time. • A new AusPAR will be developed to reflect changes to indications and/or major variations to a prescription medicine subject to evaluation by the TGA. -

A Novel Disease Affecting US Veterans
Identifying and Evaluating Sources of Evidence of Quinism: A Novel Disease Affecting U.S. Veterans Remington Nevin, MD, MPH, DrPH Executive Director Neuropsychiatric Quinism • Significant empirical evidence of a common set of symptoms and signs developing after exposure to quinoline drugs – Quinine, quinacrine, clioquinol, primaquine, chloroquine, mefloquine, tafenoquine, and others – 100+ years of case reports, pharmacovigilance reports, and accumulated clinical observations • Significant in vitro and in vivo evidence of a common pathophysiology – Chronic encephalopathy from focal brainstem and limbic neurotoxicity – Idiosyncratic effects at prophylactic doses Nevin RL. Neuropsychiatric Quinism: Chronic Encephalopathy Caused by Poisoning by Mefloquine and Related Quinoline Drugs. In: Ritchie EC, Llorente M, eds. Veteran Psychiatry in the US. Cham, Switzerland: Springer Nature; 2019. doi:10.1007/978-3-030-05384-0. In press. “Psychiatric symptoms such as insomnia, abnormal dreams/nightmares, acute anxiety, depression, restlessness or confusion have to be regarded as prodromal for a more serious event.” Roche UK. Lariam product documentation, June 2018. Emphasis added. Confounding Insomnia Exposure assumed causation Nightmares to Traumas Depression independent causation Anxiety correlation Confounder Confounding Insomnia Exposure assumed causation Nightmares to Traumas Depression actual causation Anxiety correlation Disequilibrium Mefloquine Vertigo Nevin RL. Mefloquine Exposure May Confound Associations and Limit Inference in Military Studies of Posttraumatic Stress Disorder. Military Medicine. 2017;182(11/12):1757. WRMI-2 • “Have you ever taken the weekly drug mefloquine (also known as Lariam®) to prevent malaria?" • If yes, “At any time while taking the drug, did you experience abnormal dreams or nightmares, insomnia, anxiety, depression, restlessness, or confusion?” © 2018 Remington Nevin. Under license to The Quinism Foundation. -
Injectable Anti-Malarials Revisited: Discovery and Development of New Agents to Protect Against Malaria
Macintyre et al. Malar J (2018) 17:402 https://doi.org/10.1186/s12936-018-2549-1 Malaria Journal REVIEW Open Access Injectable anti‑malarials revisited: discovery and development of new agents to protect against malaria Fiona Macintyre1, Hanu Ramachandruni1, Jeremy N. Burrows1, René Holm2,3, Anna Thomas1, Jörg J. Möhrle1, Stephan Duparc1, Rob Hooft van Huijsduijnen1 , Brian Greenwood4, Winston E. Gutteridge1, Timothy N. C. Wells1* and Wiweka Kaszubska1 Abstract Over the last 15 years, the majority of malaria drug discovery and development eforts have focused on new mol- ecules and regimens to treat patients with uncomplicated or severe disease. In addition, a number of new molecular scafolds have been discovered which block the replication of the parasite in the liver, ofering the possibility of new tools for oral prophylaxis or chemoprotection, potentially with once-weekly dosing. However, an intervention which requires less frequent administration than this would be a key tool for the control and elimination of malaria. Recent progress in HIV drug discovery has shown that small molecules can be formulated for injections as native molecules or pro-drugs which provide protection for at least 2 months. Advances in antibody engineering ofer an alternative approach whereby a single injection could potentially provide protection for several months. Building on earlier profles for uncomplicated and severe malaria, a target product profle is proposed here for an injectable medicine providing long-term protection from this disease. As with all of such profles, factors such as efcacy, cost, safety and tolerability are key, but with the changing disease landscape in Africa, new clinical and regulatory approaches are required to develop prophylactic/chemoprotective medicines. -
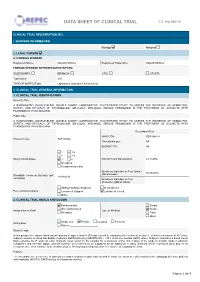
Data Sheet of Clinical Trial C.T
DATA SHEET OF CLINICAL TRIAL C.T. No 048-14 CLINICAL TRIAL REGISTRATION (EC) I. SPONSOR INFORMATION Foreign National 2. LEGAL PERSON 2.1 FOREIGN SPONSOR Registered Name: GlaxoSmithKline Registered Tradename: GlaxoSmithKline FOREIGN SPONSOR REPRESENTATIVE IN PERU SUBSIDIARY: BRANCH: CRO: OTHER: _________ Tradename: N/A TYPE OF INSTITUTION Laboratorio (Industria Farmacéutica) II. CLINICAL TRIAL GENERAL INFORMATION 1. CLINICAL TRIAL IDENTIFICATION Scientific Title: A RANDOMIZED, DOUBLE-BLIND, DOUBLE DUMMY, COMPARATIVE, MULTICENTER STUDY TO ASSESS THE INCIDENCE OF HEMOLYSIS, SAFETY, AND EFFICACY OF TAFENOQUINE (SB-252263, WR238605) VERSUS PRIMAQUINE IN THE TREATMENT OF SUBJECTS WITH PLASMODIUM VIVAX MALARIA Public Title: A RANDOMIZED, DOUBLE-BLIND, DOUBLE DUMMY, COMPARATIVE, MULTICENTER STUDY TO ASSESS THE INCIDENCE OF HEMOLYSIS, SAFETY, AND EFFICACY OF TAFENOQUINE (SB-252263, WR238605) VERSUS PRIMAQUINE IN THE TREATMENT OF SUBJECTS WITH PLASMODIUM VIVAX MALARIA Secundary ID(s): WHO UTN: PER-048-14 Protocol Code: TAF116564 Clinicaltrials.gov: NA EUDRACT N°: NA 1 1-2 2 2-3 Study clinical phase: 3 4 Clinical Trial Total Duration: 24 months No Aplica 0(exploratory trials) Enrolment start date in Peru (Initial) 30/12/2014 Worldwide enrolment start date (dd/ (dd/mm/aaaa): 18/09/2014 mm/aaaa): Enrolment start date in Peru (Posterior) (dd/mm/aaaa): Without starting enrollment In enrollment Peru enrolment status : Enrollment stopped Enrollment closed Other 2. CLINICAL TRIAL GOALS AND DESIGN Randomnized Simple Non randomnized Double Assignation method Type of blinding No aplica Triple Open Single arm Parallel Crossed Factorial Assignation Others: ____________________ Study Design In this prospective, double-blind, double-dummy design, a total of 300 subjects will be randomized to treatment on Day 1, of which a minimum of 50 female subjects must be enrolled that display moderate G6PD deficiency (≥40% - <70% of the site median G6PD value). -

How to Protect Yourself Against Malaria 1 Fig
From our Whitepaper Files: How to > See companion document Protect Yourself Against Malaria World Malaria Risk Chart 2015 Edition Canada 67 Mowat Avenue, Suite 036 Toronto, Ontario M6K 3E3 (416) 652-0137 USA 1623 Military Road, #279 Niagara Falls, New York 14304-1745 (716) 754-4883 New Zealand 206 Papanui Road Christchurch 5 www.iamat.org | [email protected] | Twitter @IAMAT_Travel | Facebook IAMATHealth THE ENEMY area. Of the 460 Anopheles species, approximately 100 can transmit malaria Sunset — the hunt for human blood begins. parasites. From dusk to dawn the female Anopheles, Mosquitoes prey on a variety of hosts — the malaria-carrying mosquito searches for a host humans, monkeys, lizards, birds — carrying to supply her with blood. Blood is an absolute different species of malaria parasites which in necessity for her because it provides the protein turn infect only specific hosts. Of the approxi- needed for the development of her eggs which mately 50 different species of malaria parasites she later deposits in her breeding place. sharing the genetic name Plasmodium, only She has a tiny, elegant body, measuring 5 infect humans: Plasmodium falciparum, from 8 mm to 1 cm. She has dark spots on the killer; Plasmodium vivax; Plasmodium ovale, her wings, three pairs of long, slender legs and Plasmodium malariae and Plasmodium knowlesi. a prominent tubular proboscis with which The latter, a malaria parasite of Old World she draws blood. monkeys, has been identified to infect humans Fig. 1 Female Anopheles mosquito. The Anopheles enters your room at night. in Southeast Asia. In the past this parasite has Image source: World Health Organization You may recognize her by the way she rests been misdiagnosed as Plasmodium malariae. -

The History and Ethics of Malaria Eradication and Control Campaigns in Tropical Africa
Malaria Redux: The History and Ethics of Malaria Eradication and Control Campaigns in Tropical Africa Center for Historical Research Ohio State University Spring 2012 Seminars: Epidemiology in World History Prof. J.L.A. Webb, Jr. Department of History Colby College DRAFT: NOT FOR CITATION 2 During the 1950s, colonial malariologists, in conjunction with experts from the World Health Organization (WHO), set up malaria eradication pilot projects across tropical Africa. They deployed new synthetic insecticides such as DLD, HCH, and DDT, and new antimalarials, such as chloroquine and pyrimethamine, in an effort to establish protocols for eradication. These efforts ‘protected’ some fourteen million Africans. Yet by the early 1960s, the experts concluded that malaria eradication was not feasible, and the pilot projects were disbanded. The projects had achieved extremely low levels of infection for years at a time, but the experts had to accept with regret that their interventions were unable to reduce malaria transmission to zero. The projects had high recurrent costs, and it was understood that they were financially unsustainable. The pilot projects were allowed to lapse. The malaria eradication pilot projects had reduced the rates of infection to levels so low that the ‘protected’ populations lost their acquired immunities to malaria during the years of the projects. In the immediate aftermath of the projects, the Africans were subject to severe malaria, which sometimes afflicted entire communities in epidemic form, until they regained their immunities. How Should We Understand the Ethics of the Early Eradication Efforts? The ethics of malaria control in the 1950s and 1960s seemed self-evident to the interventionists. -

Prevention of Malaria in Travellers (Pdf 59KB)
THEME Travel medicine Prevention of malaria in travellers BACKGROUND Malaria remains endemic in over 100 countries worldwide. Travellers to these countries may be at risk of contracting disease. Assessing risk on an individual basis can be challenging. Trish Batchelor OBJECTIVE MBBS, MPH, FRACGP, is This article identifies the traveller at high risk of contracting malaria, outlines preventive methods, including personal Medical Director, Travel Doctor- protection and chemoprophylaxis if indicated, and summarises the risks and benefits of the most commonly used TMVC, Canberra, Australian chemoprophylactic agents. Capital Territory, and Executive Board Member, International DISCUSSION Society of Travel Medicine. Appropriately assessing the risk of malaria in an individual traveller can be complex. A number of factors beyond the trish.batchelor@traveldoctor. com.au country being visited influence the level of risk. These should be identified and taken into account when discussing malaria prevention with individuals. The traveller should be actively involved in the decision making process in order Tony Gherardin to enhance compliance. High risk individuals should be identified. Personal protection methods should always be MBBS, MPH, FRACGP, is emphasised. If chemoprophylaxis is indicated, the contraindications, advantages and side effects should be discussed. National Medical Adviser, Travel Doctor-TMVC, If in doubt, referral to a specialised travel medicine clinic should be considered. Melbourne, Victoria. The malaria parasite, spread via the bite of an infected Risk for travellers female Anopheles mosquito, remains a significant health threat in over 100 countries worldwide. An The risk of contracting malaria varies significantly from estimated 350–500 million cases occur annually, with traveller to traveller, and this is the challenge of providing over a million sub-Saharan Africans, mainly children, quality advice. -

Chemoprophylaxis of Tropical Infectious Diseases
Pharmaceuticals 2010, 3, 1561-1575; doi:10.3390/ph3051561 OPEN ACCESS pharmaceuticals ISSN 1424-8247 www.mdpi.com/journal/pharmaceuticals Review Chemoprophylaxis of Tropical Infectious Diseases William J. H. McBride School of Medicine and Dentistry, James Cook University, Cairns Base Hospital campus, The Esplanade, Cairns, Queensland 4870, Australia; E-Mail: [email protected]; Tel.: +617-40506530; Fax: +617-40506831 Received: 08 April 2010; in revised form: 28 April 2010 / Accepted: 10 May 2010 / Published: 18 May 2010 Abstract: Travelers to tropical countries are at risk for a variety of infectious diseases. In some cases effective vaccinations are available, but for other infections chemoprophylaxis can be offered. Malaria prevention has become increasingly complex as Plasmodium species become resistant to available drugs. In certain high risk settings, antibiotics can be used to prevent leptospirosis, scrub typhus and other infections. Post-exposure prophylaxis is appropriate for selected virulent infections. In this article the evidence for chemoprophylaxis will be reviewed. Keywords: chemoprophylaxis; malaria; leptospirosis; scrub typhus; diarrhea 1. Introduction Chemoprophylaxis is the administration of drug to prevent the development of a disease. This review will focus on the use of medications to prevent tropical infectious diseases. The use of chemo- prophylactic agents is based on knowledge of the epidemiology and clinical implications of the infectious diseases from which protection is sought. Generally, chemoprophylaxis is taken for diseases that are common, or where the clinical impact of infection is high. Drugs may be taken before exposure (pre-exposure prophylaxis) or after potential exposure to an infectious agent (post-exposure prophylaxis). In addition to the severity and frequency of the disease, the tolerability, toxicity and ecological implications of the medications being used are important considerations in whether drugs are prescribed and taken. -

Mefloquine Poisoning and VA Service Connection
Mefloquine Poisoning and VA Service Connection Presentation to the State Bar of Texas Military and Veterans Law Section March 29, 2019 Salado, Texas Remington Nevin, MD, MPH, DrPH Executive Director Photo credit: Dr. Remington Nevin Photo credits: Dr. Remington Nevin Background • Mefloquine was developed by the U.S. military as an antimalarial drug – Origins in the late 1960s during a Vietnam War-era program • Widespread use in the U.S. military beginning in the early 1990s (e.g. Somalia, SOCOM, OIF/OEF, AFRICOM) – Tens (hundreds?) of thousands of veterans have been exposed • Recently deprioritized for use by DoD – Followed U.S. and international “black box” warnings and recognition of chronic psychiatric and neurologic effects 2013 “Drug of Last Resort” Policy Memorandum “Mefloquine is the drug of last resort for malaria chemoprophylaxis and should only be used in persons with contraindications to chloroquine, doxycycline and atovaquone- proguanil.” Declining Use of Mefloquine within DoD Woodson J. Memorandum. Subject: Notification for Healthcare Providers of Mefloquine Box Warning. August 12, 2013. Emphasis added. “[Mefloquine] may cause long lasting serious mental problems… Some people who have taken [mefloquine] developed serious neuropsychiatric reactions…” Roche UK. Lariam product documentation, June 2018. Emphasis added. “Psychiatric symptoms such as insomnia, abnormal dreams/nightmares, acute anxiety, depression, restlessness or confusion have to be regarded as prodromal for a more serious event.” Roche UK. Lariam product documentation, June 2018. Emphasis added. “In a small number of patients, it has been reported that neuropsychiatric reactions (e.g. depression, dizziness, or vertigo and loss of balance) may persist for months or longer, even after discontinuation of the drug.” Roche UK. -

Press Release Tafenoquine Approved in Peru
PRESS RELEASE TAFENOQUINE APPROVED IN PERU Perú becomes second malaria-endemic country in Latin America to approve single- dose tafenoquine for radical cure of P. vivax malaria • Tafenoquine is the first drug approved for the radical cure (relapse prevention) of P. vivax malaria in more than 60 years. • As a single dose, tafenoquine offers a much shorter treatment regimen compared to current standard of care, with the benefit of increasing patient compliance and helping to advance malaria elimination efforts. Lima, January 2021. GSK and Medicines for Malaria Venture (MMV) announced that the General Directorate of Medicines, Supplies and Drugs (DIGEMID) has issued marketing authorization for single-dose tafenoquine for radical cure (prevention relapse) of Plasmodium vivax (P. vivax) malaria in patients 16 years of age or older receiving chloroquine for acute P. vivax infection (blood-stage). Peru becomes the second malaria endemic country in Latin America after Brazil to approve single dose tafenoquine for the prevention of relapse of P. vivax malaria. As a single-dose treatment, tafenoquine facilitates compliance and thus overcomes one of the major limitations of the only other drug approved for the prevention of relapse of P. vivax malaria, primaquine, which needs to be taken for 7 days. “The history of Peru and malaria are deeply entwined. In the nineteenth century, the famous writer Ricardo Palma, made malaria part of his narratives in the book Tradiciones Peruanas. In the same way, the cinchona tree, formerly known to be effective against malaria and from which quinine is derived, is part of the National Emblem”, said Dr José Sandoval, GSK Peru’s Medical Director.