Biosafety Manual 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Assessing Neurotoxicity of Drugs of Abuse
National Institute on Drug Abuse RESEARCH MONOGRAPH SERIES Assessing Neurotoxicity of Drugs of Abuse 136 U.S. Department of Health and Human Services • Public Health Service • National Institutes of Health Assessing Neurotoxicity of Drugs of Abuse Editor: Lynda Erinoff, Ph.D. NIDA Research Monograph 136 1993 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutes of Health National Institute on Drug Abuse 5600 Fishers Lane Rockville, MD 20857 ACKNOWLEDGMENT This monograph is based on the papers and discussions from a technical review on “Assessing Neurotoxicity of Drugs of Abuse” held on May 20-21, 1991, in Bethesda, MD. The technical review was sponsored by the National Institute on Drug Abuse (NIDA). COPYRIGHT STATUS NIDA has obtained permission from the copyright holders to reproduce certain previously published material as noted in the text. Further reproduction of this copyrighted material is permitted only as part of a reprinting of the entire publication or chapter. For any other use, the copyright holder’s permission is required. All other material in this volume except quoted passages from copyrighted sources is in the public domain and may be used or reproduced without permission from the Institute or the authors. Citation of the source is appreciated. Opinions expressed in this volume are those of the authors and do not necessarily reflect the opinions or official policy of the National Institute on Drug Abuse or any other part of the U.S. Department of Health and Human Services. The U.S. Government does not endorse or favor any specific commercial product or company. -

Medical Management of Biological Casualties Handbook
USAMRIID’s MEDICAL MANAGEMENT OF BIOLOGICAL CASUALTIES HANDBOOK Sixth Edition April 2005 U.S. ARMY MEDICAL RESEARCH INSTITUTE OF INFECTIOUS DISEASES FORT DETRICK FREDERICK, MARYLAND Emergency Response Numbers National Response Center: 1-800-424-8802 or (for chem/bio hazards & terrorist events) 1-202-267-2675 National Domestic Preparedness Office: 1-202-324-9025 (for civilian use) Domestic Preparedness Chem/Bio Helpline: 1-410-436-4484 or (Edgewood Ops Center – for military use) DSN 584-4484 USAMRIID’s Emergency Response Line: 1-888-872-7443 CDC'S Emergency Response Line: 1-770-488-7100 Handbook Download Site An Adobe Acrobat Reader (pdf file) version of this handbook can be downloaded from the internet at the following url: http://www.usamriid.army.mil USAMRIID’s MEDICAL MANAGEMENT OF BIOLOGICAL CASUALTIES HANDBOOK Sixth Edition April 2005 Lead Editor Lt Col Jon B. Woods, MC, USAF Contributing Editors CAPT Robert G. Darling, MC, USN LTC Zygmunt F. Dembek, MS, USAR Lt Col Bridget K. Carr, MSC, USAF COL Ted J. Cieslak, MC, USA LCDR James V. Lawler, MC, USN MAJ Anthony C. Littrell, MC, USA LTC Mark G. Kortepeter, MC, USA LTC Nelson W. Rebert, MS, USA LTC Scott A. Stanek, MC, USA COL James W. Martin, MC, USA Comments and suggestions are appreciated and should be addressed to: Operational Medicine Department Attn: MCMR-UIM-O U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) Fort Detrick, Maryland 21702-5011 PREFACE TO THE SIXTH EDITION The Medical Management of Biological Casualties Handbook, which has become affectionately known as the "Blue Book," has been enormously successful - far beyond our expectations. -
Biosafety Level 1 and Rdna Training
Biosafety Level 1and rDNA Training Office of Biological Safety Biosafety Level 1 and rDNA Training • Difference between Risk Group and Biosafety Level • NIH and UC policy on recombinant DNA • Work conducted at Biosafety Level 1 • UC Code of Conduct for researchers Biosafety Level 1 and rDNA Training What is the difference between risk group and biosafety level? Risk Groups vs Biosafety Level • Risk Groups: Assigned to infectious organisms by global agencies (NIH, CDC, WHO, etc.) • In US, only assigned to human pathogens (NIH) • Biosafety Level (BSL): How the organisms are managed/contained (increasing levels of protection) Risk Groups vs Biosafety Level • RG1: Not associated with disease in healthy adults (non‐pathogenic E. coli; S. cerevisiae) • RG2: Cause diseases not usually serious and are often treatable (S. aureus; Legionella; Toxoplasma gondii) • RG3: Serious diseases that may be treatable (Y. pestis; B. anthracis; Rickettsia rickettsii; HIV) • RG4: Serious diseases with no treatment/cure (Hemorrhagic fever viruses, e.g., Ebola; no bacteria) Risk Groups vs Biosafety Level • BSL‐1: Usually corresponds to RG1 – Good microbiological technique – No additional safety equipment required for biological work (may still need chemical/radiation protection) – Ability to destroy recombinant organisms (even if they are RG1) Risk Groups vs Biosafety Level • BSL‐2: Same as BSL‐1, PLUS… – Biohazard signs – Protective clothing (lab coat, gloves, eye protection, etc.) – Biosafety cabinet (BSC) for aerosols is recommended but not always required – Negative airflow into room is recommended, but not always required Risk Groups vs Biosafety Level • BSL‐3: Same as BSL‐2, PLUS… – Specialized clothing (respiratory protection, Tyvek, etc.) – Directional air flow is required. -

Taipoxin Induces Synaptic Vesicle Exocytosis And
Molecular Pharmacology Fast Forward. Published on February 4, 2005 as DOI: 10.1124/mol.104.005678 Molecular PharmacologyThis article has Fast not beenForward. copyedited Published and formatted. on The February final version 4, may 2005 differ as from doi:10.1124/mol.104.005678 this version. MOL # 5678 Taipoxin induces synaptic vesicle exocytosis and disrupts the interaction of synaptophysin I Downloaded from with VAMP2 molpharm.aspetjournals.org Dario Bonanomi, Maria Pennuto, Michela Rigoni, Ornella Rossetto, Cesare Montecucco and Flavia Valtorta Department of Neuroscience, S. Raffaele Scientific Institute and “Vita-Salute” University, Milan, Italy (D.B., M.P., F.V.); Department of Biomedical Sciences, University of Padova, Italy (M.R., O.R., C.M.) at ASPET Journals on October 1, 2021 1 Copyright 2005 by the American Society for Pharmacology and Experimental Therapeutics. Molecular Pharmacology Fast Forward. Published on February 4, 2005 as DOI: 10.1124/mol.104.005678 This article has not been copyedited and formatted. The final version may differ from this version. MOL # 5678 Running title: Effects of taipoxin on SypI-VAMP2 interactions Address for correspondence: Flavia Valtorta DIBIT 3A3 San Raffaele Scientific Institute via Olgettina 58 20132 Milan, Italy telephone: 39-022643-4826 telefax: 39-022643-4813 e- mail: [email protected] Downloaded from Number of text pages: 29 molpharm.aspetjournals.org Number of tables: = = = Number of figures: 7 Number of references: 33 Number of words in the Abstract: 102 at ASPET Journals on October -

Biological Safety Guide
Biological Safety Guide Biological Safety Office Environmental Health & Safety Division 1405 Goss Lane, CI 1001 Augusta, Georgia 30912 Revised: February 2014 STATEMENT OF AUTHORITY Upon publication of these procedures, the Institutional Biosafety Committee (IBC) of the Georgia Regents University, is hereby authorized to act as agent for the Georgia Regents University in matters of review, control, and mediation arising from the use or proposed use of biological materials, including recombinant DNA, at the Georgia Regents University. A statement of composition of the Institutional Biosafety Committee and a delineation of authority is included in the following pages of this text. Furthermore, it is hereby declared that the Biological Safety Office of the Georgia Regents University derives its authority directly from the Office of the President of the Georgia Regents University in all matters involving biological safety and/or violations of accepted rules of practice as described herein. The Biosafety Officer is hereby granted the authority to immediately suspend a project which is found to be a threat to health, property, or the environment. ____________________________________ __________________ James J. Rush, Jr, Esq Date Chief Integrity Officer Georgia Regents University Georgia Regents University Biosafety Guide-January 2012 Statement of Authority TABLE OF CONTENTS List of Abbreviations .............................................................................. viii Forward ................................................................................................. -

(Oxyuranus) and Brown Snakes (Pseudonaja) Differ in Composition of Toxins Involved in Mammal Poisoning
bioRxiv preprint doi: https://doi.org/10.1101/378141; this version posted July 26, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Venoms of related mammal-eating species of taipans (Oxyuranus) and brown snakes (Pseudonaja) differ in composition of toxins involved in mammal poisoning Jure Skejic1,2,3*, David L. Steer4, Nathan Dunstan5, Wayne C. Hodgson2 1 Department of Biochemistry and Molecular Biology, BIO21 Institute, University of Melbourne, 30 Flemington Road, Parkville, Victoria 3010, Australia 2 Monash Venom Group, Department of Pharmacology, Monash University, 9 Ancora Imparo Way, Clayton, Victoria 3800, Australia 3 Laboratory of Evolutionary Genetics, Division of Molecular Biology, Ruder Boskovic Institute, Bijenicka 54, 10000 Zagreb, Croatia 4 Monash Biomedical Proteomics Facility, Monash University, 23 Innovation Walk, Clayton, Victoria 3800, Australia 5 Venom Supplies Pty Ltd., Stonewell road, Tanunda, South Australia 5352, Australia * Correspondence: [email protected] 1 bioRxiv preprint doi: https://doi.org/10.1101/378141; this version posted July 26, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Abstract Background Differences in venom composition among related snake lineages have often been attributed primarily to diet. Australian elapids belonging to taipans (Oxyuranus) and brown snakes (Pseudonaja) include a few specialist predators as well as generalists that have broader dietary niches and represent a suitable model system to investigate this assumption. Here, shotgun high-resolution mass spectrometry (Q Exactive Orbitrap) was used to compare venom proteome composition of several related mammal-eating species of taipans and brown snakes. -

Alphabetical Listing of Export Restricted Biological Items
Alphabetical Listing of Export Restricted Biological Items There are two sets of regulations for export restricted biological items, the International Traffic in Arms Regulations (ITAR) from Dept. of State and the Export Administration Regulations from Dept. of Commerce. These items require export licenses to all countries. Licensing takes about 6 weeks. Fines are $250,000 to $1,094,010 per violation. See the Export Control website within the Office of Research at: https://research.uci.edu/ref/export-controls/index.html These listed items are controlled for export regardless of quantity or attenuation, genetic elements or genetically modified organisms for such agents or “toxins”, including small quantities or attenuated strains of select biological agents or “toxins” that are excluded from the lists of select biological agents or “toxins” by APHIS, CDC, or DHHS. Under the ITAR, Biological agents and biologically derived substances specifically developed, configured, adapted, or modified for the purpose of increasing their capability to produce casualties in humans or livestock, degrade equipment or damage crops are controlled under CATEGORY XIV—TOXICOLOGICAL AGENTS, INCLUDING CHEMICAL AGENTS, BIOLOGICAL AGENTS, AND ASSOCIATED EQUIPMENT. Please note that there are proposed regulations on this category that if they become final will impact the listing of biologicals. See Part 121 United States Munitions List Category XIV. Certain precursor chemicals, Biosafety gear, and lab equipment are also export restricted see Categories 1 & 2 of the -

AM 1/06 Mont⁄Ě
REVIEW ARTICLE PROTEIN BIOTOXINS OF MILITARY SIGNIFICANCE Jiří Patočka1, Ladislav Středa2 University of Defence, Faculty of Military Health Sciences, Czech Republic: Department of Toxicology1; University of South Bohemia, Faculty of Health and Social Studies, Czech Republic: Department of Radiology and Toxicology1; State Office for Nuclear Safety, Czech Republic: Department for Control of the Prohibition of Chemical Weapons2 Summary: There is a spectrum of several threat agents, ranging from nerve agents and mustard agents to natural substan- ces, such as biotoxins and new, synthetic, bioactive molecules produced by the chemical industry, to the classical biologi- cal warfare agents. The new, emerging threat agents are biotoxins produced by animals, plants, fungi, and bacteria. Many types of organisms produce substances that are toxic to humans. Examples of such biotoxins are botulinum toxin, tetanus toxin, and ricin. Several bioactive molecules produced by the pharmaceutical industry can be even more toxic than are the classical chemical warfare agents. Such new agents, like the biotoxins and bioregulators, often are called mid-spectrum agents. The threat to humans from agents developed by modern chemical synthesis and by genetic engineering also must be considered, since such agents may be more toxic or more effective in causing death or incapacitation than classical war- fare agents. By developing effective medical protection and treatment against the most likely chemical and mid-spectrum threat agents, the effects of such agents in a war scenario or following a terrorist attack can be reduced. Toxin-mediated di- seases have made humans ill for millennia. Unfortunately, the use of biological agents as weapons of terror has now been realized, and separating naturally occurring disease from bioterroristic events has become an important public health goal. -

Environmental Protection Agency § 725.422
Environmental Protection Agency § 725.422 below in paragraphs (d)(2) through Sequence Source Toxin Name (d)(7) of this section, these comparable Bacillus anthracis Edema factor (Factors I II); toxin sequences, regardless of the orga- Lethal factor (Factors II III) nism from which they are derived, Bacillus cereus Enterotoxin (diarrheagenic must not be included in the introduced toxin, mouse lethal factor) genetic material. Bordetella pertussis Adenylate cyclase (Heat-la- (2) Sequences for protein synthesis in- bile factor); Pertussigen (pertussis toxin, islet acti- hibitor. vating factor, histamine sensitizing factor, Sequence Source Toxin Name lymphocytosis promoting factor) Corynebacterium diphtheriae Diphtheria toxin Clostridium botulinum C2 toxin & C. ulcerans Clostridium difficile Enterotoxin (toxin A) Pseudomonas aeruginosa Exotoxin A Clostridium perfringens Beta-toxin; Delta-toxin Shigella dysenteriae Shigella toxin (Shiga toxin, Shigella dysenteriae type I Escherichia coli & other Heat-labile enterotoxins (LT); toxin, Vero cell toxin) Enterobacteriaceae spp. Heat-stable enterotoxins Abrus precatorius, seeds Abrin (STa, ST1 subtypes ST1a Ricinus communis, seeds Ricin ST1b; also STb, STII) Legionella pneumophila Cytolysin (3) Sequences for neurotoxins. Vibrio cholerae & Vibrio Cholera toxin (choleragen) mimicus Sequence Source Toxin Name (6) Sequences that affect membrane Clostridium botulinum Neurotoxins A, B, C1, D, E, integrity. F, G (Botulinum toxins, botulinal toxins) Sequence Source Toxin Name Clostridium tetani Tetanus toxin -

Snake Presynaptic Neurotoxins with Phospholipase A2 Activity Induce Punctate Swellings of Neurites and Exocytosis of Synaptic Vesicles
Research Article 3561 Snake presynaptic neurotoxins with phospholipase A2 activity induce punctate swellings of neurites and exocytosis of synaptic vesicles Michela Rigoni1, Giampietro Schiavo2, Anne E. Weston2, Paola Caccin1, Federica Allegrini1, Maria Pennuto3, Flavia Valtorta3, Cesare Montecucco1 and Ornella Rossetto1,* 1Department of Biomedical Sciences and CNR Institute of Neuroscience, University of Padova, Viale G. Colombo 3, 35121 Padova, Italy 2Molecular NeuroPathoBiology Laboratory, Cancer Research UK, London Research Institute, 61 Lincoln’s Inn Fields, London, WC2A 3PX, UK 3Department of Neuroscience, S. Raffaele Scientific Institute and ‘Vita-Salute’ University, Via Olgettina 58, 20132 Milan, Italy *Author for correspondence (e-mail: [email protected]) Accepted 11 March 2004 Journal of Cell Science 117, 3561-3570 Published by The Company of Biologists 2004 doi:10.1242/jcs.01218 Summary The mechanisms of action of four snake presynaptic observed in neurons, but not in astrocytes. These findings phospholipase A2 neurotoxins were investigated in indicate that these snake presynaptic neurotoxins act with cultured neurons isolated from various parts of the rat by same mechanism and that the observed phenotype brain. Strikingly, physiological concentrations of notexin, results from the fusion of synaptic vesicles with the plasma β-bungarotoxin, taipoxin or textilotoxin induced a dose- membrane not balanced by an adequate membrane dependent formation of discrete bulges at various sites of retrieval. These changes closely resemble those occurring neuronal projections. Neuronal bulging was paralleled by at neuromuscular junctions of intoxicated animals and the redistribution of the two synaptic vesicle markers fully qualify these primary neuronal cultures as pertinent synaptophysin I (SypI) and vesicle-attached membrane models for studying the molecular mode of action of these protein 2 (VAMP2) to the bulges, and by the exposure of neurotoxins. -

Integrating the Neurobiology of Schizophrenia
International REVIEW OF Neurobiology Volume 78 International REVIEW OF Neurobiology Volume 78 SERIES EDITORS RONALD J. BRADLEY Department of Psychiatry, College of Medicine The University of Tennessee Health Science Center Memphis, Tennessee, USA R. ADRON HARRIS Waggoner Center for Alcohol and Drug Addiction Research The University of Texas at Austin Austin, Texas, USA PETER JENNER Division of Pharmacology and Therapeutics GKT School of Biomedical Sciences King’s College, London, UK EDITORIAL BOARD ERIC AAMODT HUDA AKIL PHILIPPE ASCHER MATTHEW J. DURING DONARD S. DWYER DAVID FINK MARTIN GIURFA MICHAEL F. GLABUS PAUL GREENGARD BARRY HALLIWELL NOBU HATTORI JON KAAS DARCY KELLEY LEAH KRUBITZER BEAU LOTTO KEVIN MCNAUGHT MICAELA MORELLI JOSE´ A. OBESO JUDITH PRATT CATHY J. PRICE EVAN SNYDER SOLOMON H. SNYDER JOHN WADDINGTON STEPHEN G. WAXMAN Integrating the Neurobiology of Schizophrenia EDITED BY ANISSA ABI-DARGHAM Department of Psychiatry, Columbia College of Physicians and Surgeons New York State Psychiatric Institute Columbia University, New York, USA OLIVIER GUILLIN Unite´ de Psychiatrie CHU ch. Nicolle Rouen, France AMSTERDAM • BOSTON • HEIDELBERG • LONDON NEW YORK • OXFORD • PARIS • SAN DIEGO SAN FRANCISCO • SINGAPORE • SYDNEY • TOKYO Academic Press is an imprint of Elsevier Academic Press is an imprint of Elsevier 525 B Street, Suite 1900, San Diego, California 92101-4495, USA 84 Theobald’s Road, London WC1X 8RR, UK This book is printed on acid-free paper. Copyright ß 2007, Elsevier Inc. All Rights Reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording, or any information storage and retrieval system, without permission in writing from the Publisher. -
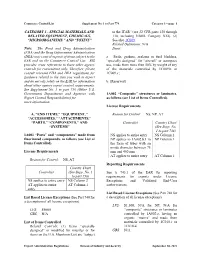
Category 1—Page 1
Commerce Control List Supplement No. 1 to Part 774 Category 1—page 1 CATEGORY 1 - SPECIAL MATERIALS AND to the ITAR” (see 22 CFR parts 120 through RELATED EQUIPMENT, CHEMICALS, 130, including USML Category XXI). (2) “MICROORGANISMS,” AND “TOXINS” See also 1C009. Related Definitions: N/A Note: The Food and Drug Administration Items: (FDA) and the Drug Enforcement Administration (DEA) may control exports of items subject to the a. Seals, gaskets, sealants or fuel bladders, EAR and on the Commerce Control List. BIS “specially designed” for “aircraft” or aerospace provides cross references to these other agency use, made from more than 50% by weight of any controls for convenience only. Therefore, please of the materials controlled by 1C009.b or consult relevant FDA and DEA regulations for 1C009.c; guidance related to the item you wish to export and do not rely solely on the EAR for information b. [Reserved] about other agency export control requirements. See Supplement No. 3 to part 730 (Other U.S. Government Departments and Agencies with 1A002 “Composite” structures or laminates, Export Control Responsibilities) for as follows (see List of Items Controlled). more information. License Requirements A. “END ITEMS,” “EQUIPMENT,” Reason for Control: NS, NP, AT “ACCESSORIES,” “ATTACHMENTS,” “PARTS,” “COMPONENTS,” AND Control(s) Country Chart “SYSTEMS” (See Supp. No. 1 to part 738) 1A001 “Parts” and “components” made from NS applies to entire entry NS Column 2 fluorinated compounds, as follows (see List of NP applies to 1A002.b.1 in NP Column 1 Items Controlled). the form of tubes with an inside diameter between 75 License Requirements mm and 400 mm AT applies to entire entry AT Column 1 Reason for Control: NS, AT Reporting Requirements Country Chart Control(s) (See Supp.