I. General Introduction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Role of Streptococcal and Staphylococcal Exotoxins and Proteases in Human Necrotizing Soft Tissue Infections
toxins Review The Role of Streptococcal and Staphylococcal Exotoxins and Proteases in Human Necrotizing Soft Tissue Infections Patience Shumba 1, Srikanth Mairpady Shambat 2 and Nikolai Siemens 1,* 1 Center for Functional Genomics of Microbes, Department of Molecular Genetics and Infection Biology, University of Greifswald, D-17489 Greifswald, Germany; [email protected] 2 Division of Infectious Diseases and Hospital Epidemiology, University Hospital Zurich, University of Zurich, CH-8091 Zurich, Switzerland; [email protected] * Correspondence: [email protected]; Tel.: +49-3834-420-5711 Received: 20 May 2019; Accepted: 10 June 2019; Published: 11 June 2019 Abstract: Necrotizing soft tissue infections (NSTIs) are critical clinical conditions characterized by extensive necrosis of any layer of the soft tissue and systemic toxicity. Group A streptococci (GAS) and Staphylococcus aureus are two major pathogens associated with monomicrobial NSTIs. In the tissue environment, both Gram-positive bacteria secrete a variety of molecules, including pore-forming exotoxins, superantigens, and proteases with cytolytic and immunomodulatory functions. The present review summarizes the current knowledge about streptococcal and staphylococcal toxins in NSTIs with a special focus on their contribution to disease progression, tissue pathology, and immune evasion strategies. Keywords: Streptococcus pyogenes; group A streptococcus; Staphylococcus aureus; skin infections; necrotizing soft tissue infections; pore-forming toxins; superantigens; immunomodulatory proteases; immune responses Key Contribution: Group A streptococcal and Staphylococcus aureus toxins manipulate host physiological and immunological responses to promote disease severity and progression. 1. Introduction Necrotizing soft tissue infections (NSTIs) are rare and represent a more severe rapidly progressing form of soft tissue infections that account for significant morbidity and mortality [1]. -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA). -

Report from the 26Th Meeting on Toxinology,“Bioengineering Of
toxins Meeting Report Report from the 26th Meeting on Toxinology, “Bioengineering of Toxins”, Organized by the French Society of Toxinology (SFET) and Held in Paris, France, 4–5 December 2019 Pascale Marchot 1,* , Sylvie Diochot 2, Michel R. Popoff 3 and Evelyne Benoit 4 1 Laboratoire ‘Architecture et Fonction des Macromolécules Biologiques’, CNRS/Aix-Marseille Université, Faculté des Sciences-Campus Luminy, 13288 Marseille CEDEX 09, France 2 Institut de Pharmacologie Moléculaire et Cellulaire, Université Côte d’Azur, CNRS, Sophia Antipolis, 06550 Valbonne, France; [email protected] 3 Bacterial Toxins, Institut Pasteur, 75015 Paris, France; michel-robert.popoff@pasteur.fr 4 Service d’Ingénierie Moléculaire des Protéines (SIMOPRO), CEA de Saclay, Université Paris-Saclay, 91191 Gif-sur-Yvette, France; [email protected] * Correspondence: [email protected]; Tel.: +33-4-9182-5579 Received: 18 December 2019; Accepted: 27 December 2019; Published: 3 January 2020 1. Preface This 26th edition of the annual Meeting on Toxinology (RT26) of the SFET (http://sfet.asso.fr/ international) was held at the Institut Pasteur of Paris on 4–5 December 2019. The central theme selected for this meeting, “Bioengineering of Toxins”, gave rise to two thematic sessions: one on animal and plant toxins (one of our “core” themes), and a second one on bacterial toxins in honour of Dr. Michel R. Popoff (Institut Pasteur, Paris, France), both sessions being aimed at emphasizing the latest findings on their respective topics. Nine speakers from eight countries (Belgium, Denmark, France, Germany, Russia, Singapore, the United Kingdom, and the United States of America) were invited as international experts to present their work, and other researchers and students presented theirs through 23 shorter lectures and 27 posters. -

CHAPTER E16 Atlas of Skin Manifestations of Internal Disease CHAPTER E16 Thomas J
CHAPTER e16 Atlas of Skin Manifestations of Internal Disease CHAPTER e16 Thomas J. Lawley Robert A. Swerlick In the practice of medicine, virtually every clinician encounters patients with skin disease. Physicians of all specialties face the daily task of determining the nature and clinical implication of dermatologic disease. In patients with skin eruptions and rashes, the physician must confront the question of whether the cutaneous Atlas of Skin Manifestations Internal Disease process is confined to the skin, representing a pure dermatologic event, or whether it is a manifestation of internal disease relating to the patient’s overall medical condition. Evaluation and accurate diagnosis of skin lesions are also critical given the marked rise in both melanoma and nonmelanoma skin cancer. Dermatologic conditions can be classified and categorized in many different ways, Figure e16-2 Acne rosacea with prominent facial erythema, telangiecta- and in this Atlas, a selected group of inflammatory skin eruptions sias, scattered papules, and small pustules. (Courtesy of Robert Swerlick, and neoplastic conditions are grouped in the following manner: MD; with permission.) (A) common skin diseases and lesions, (B) nonmelanoma skin cancer, (C) melanoma and pigmented lesions, (D) infectious dis- ease and the skin, (E) immunologically mediated skin disease, and (F) skin manifestations of internal disease. COMMON SKIN DISEASES AND LESIONS ( Figs. e16-1 to e16-19) In this section, several common inflamma- tory skin diseases and benign neoplastic and reactive lesions are presented. While most of these dermatoses usually present as a pre- dominantly dermatologic process, underlying systemic associations may be made in some settings. Atopic dermatitis is often present in patients with an atopic diathesis, including asthma and sinusitis. -
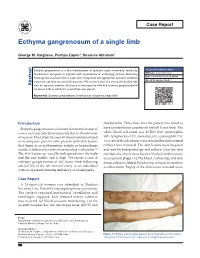
Ecthyma Gangrenosum of a Single Limb
Case Report Ecthyma gangrenosum of a single limb George M. Varghese, Pushpa Eapen1, Susanne Abraham1 Ecthyma gangrenosum is a skin manifestation of systemic sepsis commonly caused by Access this article online Pseudomonas aeruginosa in patients with neutropenia or underlying immune deficiency. Website: www.ijccm.org Although the usual outcome is poor, early recognition and appropriate systemic antibiotic DOI: 10.4103/0972-5229.84898 treatment can lead to successful outcome. We report a case of a previously healthy lady Quick Response Code: Abstract with no apparent immune deficiency or neutropenia who had ecthyma gangrenosum of left lower limb in which the arterial line was placed. Keywords: Ecthyma gangrenosum, Pseudomonas aeruginosa, single limb Introduction thachycardia. Three days later the patient was noted to Ecthyma gangrenosum is a known skin manifestation of have erythematous papules on the left lower limb. The 3 severe systemic infection commonly due to Pseudomonas white blood cell count was 16,500/mm (neutrophils aeruginosa. Most often it is seen in immunocompromised 84%, lymphocytes 12%, monocytes 3%, eosinophils 1%). or neutropenic patients who present with skin lesions Two sets of blood cultures were sent and the intra-arterial that begin as an erythematous nodule or hemorrhagic catheter was removed. The skin lesions were biopsied vesicle, which evolves into a necrotic ulcer with eschar. [1] and sent for histopathology and culture. Over the next The skin lesions are usually widespread over the body few days the skin lesions became blackish with necrotic and the case fatality rate is high. We report a case of areas (arrow) [Figure 1]. The blood, catheter tip, and skin ecthyma gangrenosum of left lower limb following lesion cultures yielded Pseudomonas aeruginosa sensitive arterial line in the left femoral artery in an individual to ceftazidime. -

Skin and Soft Tissue Infections Following Marine Injuries
CHAPTER 6 Skin and Soft Tissue Infections Following Marine Injuries V. Savini, R. Marrollo, R. Nigro, C. Fusella, P. Fazii Spirito Santo Hospital, Pescara, Italy 1. INTRODUCTION Bacterial diseases following aquatic injuries occur frequently worldwide and usually develop on the extremities of fishermen and vacationers, who are exposed to freshwater and saltwater.1,2 Though plenty of bacterial species have been isolated from marine lesions, superficial soft tissue and invasive systemic infections after aquatic injuries and exposures are related to a restricted number of microorganisms including, in alphabetical order, Aeromonas hydrophila, Chromobacterium violaceum, Edwardsiella tarda, Erysipelothrix rhusiopathiae, Myco- bacterium fortuitum, Mycobacterium marinum, Shewanella species, Streptococcus iniae, and Vibrio vulnificus.1,2 In particular, skin disorders represent the third most common cause of morbidity in returning travelers and are usually represented by bacterial infections.3–12 Bacterial skin and soft tissue infectious conditions in travelers often follow insect bites and can show a wide range of clinical pictures including impetigo, ecthyma, erysipelas, abscesses, necro- tizing cellulitis, myonecrosis.3–12 In general, even minor abrasions and lacerations sustained in marine waters should be considered potentially contaminated with marine bacteria.3–12 Despite variability of the causative agents and outcomes, the initial presentations of skin and soft tissue infections (SSTIs) complicating marine injuries are similar to those occurring after terrestrial exposures and usually include erysipelas, impetigo, cellulitis, and necrotizing infections.3 Erysipelas is characterized by fiery red, tender, painful plaques showing well-demarcated edges, and, though Streptococcus pyogenes is the major agent of this pro- cess, E. rhusiopathiae infections typically cause erysipeloid displays.3 Impetigo is initially characterized by bullous lesions and is usually due to Staphylococcus aureus or S. -

Hemolysin CB with Human C5a Receptors Γ Valentine Leukocidin
Differential Interaction of the Staphylococcal Toxins Panton−Valentine Leukocidin and γ -Hemolysin CB with Human C5a Receptors This information is current as András N. Spaan, Ariën Schiepers, Carla J. C. de Haas, of October 1, 2021. Davy D. J. J. van Hooijdonk, Cédric Badiou, Hugues Contamin, François Vandenesch, Gérard Lina, Norma P. Gerard, Craig Gerard, Kok P. M. van Kessel, Thomas Henry and Jos A. G. van Strijp J Immunol 2015; 195:1034-1043; Prepublished online 19 June 2015; Downloaded from doi: 10.4049/jimmunol.1500604 http://www.jimmunol.org/content/195/3/1034 http://www.jimmunol.org/ Supplementary http://www.jimmunol.org/content/suppl/2015/06/19/jimmunol.150060 Material 4.DCSupplemental References This article cites 46 articles, 14 of which you can access for free at: http://www.jimmunol.org/content/195/3/1034.full#ref-list-1 Why The JI? Submit online. by guest on October 1, 2021 • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2015 by The American Association of Immunologists, Inc. -

Cutaneous Manifestations of Infection in the Immunocompromised Host
Cutaneous Manifestations of Infection in the Immunocompromised Host Marc E. Grossman • Lindy P. Fox • Carrie Kovarik Misha Rosenbach Cutaneous Manifestations of Infection in the Immunocompromised Host Second Edition Authors Marc E. Grossman, M.D. Carrie Kovarik, M.D. Professor of Clinical Dermatology Assistant Professor of Dermatology College of Physicians and Surgeons Dermatopathology, and Infectious Diseases Director, Hospital Consultation Service University of Pennsylvania New York Presbyterian Hospital Philadelphia, Pennsylvania, USA Columbia University Medical Center New York, New York, USA Misha Rosenbach, M.D. Assistant Professor of Dermatology Lindy P. Fox, M.D. and Internal Medicine Associate Professor of Clinical Dermatology Director, Dermatology Inpatient Consult Service Director, Hospital Consultation Service University of Pennsylvania University of California, San Francisco Philadelphia, Pennsylvania, USA San Francisco, California, USA ISBN 978-1-4419-1577-1 e-ISBN 978-1-4419-1578-8 DOI 10.1007/978-1-4419-1578-8 Springer New York Dordrecht Heidelberg London Library of Congress Control Number: 2011933837 Springer Science+Business Media, LLC 2012 All rights reserved. Th is work may not be translated or copied in whole or in part without the written permission of the publisher (Springer Science+Business Media, LLC, 233 Spring Street, New York, NY 10013, USA), except for brief excerpts in connection with reviews or scholarly analysis. Use in connection with any form of information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter devel- oped is forbidden. Th e use in this publication of trade names, trademarks, service marks, and similar terms, even if they are not identifi ed as such, is not to be taken as an expression of opinion as to whether or not they are subject to proprietary rights. -

Panton-Valentine Leukocidin: a Review
Reprinted from www.antimicrobe.org Panton-Valentine Leukocidin: A Review Marina Morgan F.R.C.Path. Venkata Meka, M.D. Panton-Valentine leukocidin (PVL) is a bi-component, pore-forming exotoxin produced by some strains of Staphylococcus aureus. Also termed a synergohymenotropic toxin (i.e. acts on membranes through the synergistic activity of 2 non-associated secretory proteins, component S and component F) (9), PVL toxin components assemble into heptamers on the neutrophil membrane, resulting in lytic pores and membrane damage. Injection of purified PVL induces histamine release from human basophilic granulocytes, enzymes (such as β-glucuronidase and lysozyme), chemotactic factors (such as leukotriene B4 and interleukin (IL-) 8), and oxygen metabolites from human neutrophilic granulocytes (5). Intradermal injection of purified PVL in rabbits causes severe inflammatory lesions with capillary dilation, chemotaxis, polymorphonuclear (PMN) infiltration, PMN karyorrhexis, and skin necrosis (17). PVL production is encoded by two contiguous and cotranscribed genes, lukS-PV and lukF-PV, found in a prophage segment integrated in the S. aureus chromosome (9). Traditionally some 2% of S. aureus produce PVL, however in certain groups in close contact with each other, such as military personnel, prisoners, and families of patients with infected skin lesions, skin to skin transmission is common resulting in a far higher carriage rates. Different PVL-positive S. aureus strains carry differing phage sequences, which can move into other strains methicillin and resistant, empowering them with PVl production genes (15). Many patients with PVL-positive necrotizing pneumonia have a preceding illness resembling influenza, with rigors pyrexia and myalgia. Expression of most S. -

Impact of Bacterial Toxins in the Lungs
toxins Review Impact of Bacterial Toxins in the Lungs 1,2,3, , 4,5, 3 2 Rudolf Lucas * y, Yalda Hadizamani y, Joyce Gonzales , Boris Gorshkov , Thomas Bodmer 6, Yves Berthiaume 7, Ueli Moehrlen 8, Hartmut Lode 9, Hanno Huwer 10, Martina Hudel 11, Mobarak Abu Mraheil 11, Haroldo Alfredo Flores Toque 1,2, 11 4,5,12,13, , Trinad Chakraborty and Jürg Hamacher * y 1 Pharmacology and Toxicology, Medical College of Georgia at Augusta University, Augusta, GA 30912, USA; hfl[email protected] 2 Vascular Biology Center, Medical College of Georgia at Augusta University, Augusta, GA 30912, USA; [email protected] 3 Department of Medicine and Division of Pulmonary Critical Care Medicine, Medical College of Georgia at Augusta University, Augusta, GA 30912, USA; [email protected] 4 Lungen-und Atmungsstiftung, Bern, 3012 Bern, Switzerland; [email protected] 5 Pneumology, Clinic for General Internal Medicine, Lindenhofspital Bern, 3012 Bern, Switzerland 6 Labormedizinisches Zentrum Dr. Risch, Waldeggstr. 37 CH-3097 Liebefeld, Switzerland; [email protected] 7 Department of Medicine, Faculty of Medicine, Université de Montréal, Montréal, QC H3T 1J4, Canada; [email protected] 8 Pediatric Surgery, University Children’s Hospital, Zürich, Steinwiesstrasse 75, CH-8032 Zürch, Switzerland; [email protected] 9 Insitut für klinische Pharmakologie, Charité, Universitätsklinikum Berlin, Reichsstrasse 2, D-14052 Berlin, Germany; [email protected] 10 Department of Cardiothoracic Surgery, Voelklingen Heart Center, 66333 -
Dermatology in the ER
DRUG ERUPTIONS and OTHER DISORDERS Lloyd J. Cleaver D.O. , F.A.O.C.D, F.A.A.D. Professor of Dermatology ATSU-Kirksville College of Osteopathic Medicine INTERNAL MEDICINE BOARD REVIEW COURSE I Disclosures No Relevant Financial Relationships DRUG ERUPTIONS Drug Reactions 3 things you need to know 1. Type of drug reaction 2. Statistics What drugs are most likely to cause that type of reaction? 3. Timing How long after the drug was started did the reaction begin? Clinical Pearls Drug eruptions are extremely common Tend to be generalized/symmetric Maculopapular/morbilliform are most common Best Intervention: Stop the Drug! Do not dose reduce Completely remove the exposure How to spot the culprit? Drug started within days to a week prior to rash Can be difficult and take time Tip: can generally exclude all drugs started after onset of rash Drug eruptions can continue for 1-2 weeks after stopping culprit drug LITT’s drug eruption database Drug Eruptions Skin is one of the most common targets for drug reactions Antibiotics and anticonvulsants are most common 1-5% of patients 2% of all drug eruptions are “serious” TEN, DRESS More common in adult females and boys < 3 y/o Not all drugs cause eruptions at same rate: Aminopenicillins: 1.2-8% of exposures TMP-SMX: 2.8-3.7% NSAIDs: 1 in 200 Lamotrigine: 10% Drug Eruptions Three basic rules 1. Stop any unnecessary medications 2. Ask about non-prescription medications Eye drops, suppositories, implants, injections, patches, vitamin and health supplements, friend’s medications -

Multiple Roles of Staphylococcus Aureus Enterotoxins: Pathogenicity, Superantigenic Activity, and Correlation to Antibiotic Resistance
Toxins 2010, 2, 2117-2131; doi:10.3390/toxins2082117 OPEN ACCESS toxins ISSN 2072-6651 www.mdpi.com/journal/toxins Review Multiple Roles of Staphylococcus aureus Enterotoxins: Pathogenicity, Superantigenic Activity, and Correlation to Antibiotic Resistance Elena Ortega, Hikmate Abriouel, Rosario Lucas and Antonio Gálvez * Area de Microbiología, Departamento de Ciencias de la Salud, Facultad de Ciencias Experimentales, Universidad de Jaén, 23071-Jaén, Spain; E-Mails: [email protected] (E.O.); [email protected] (H.A.); [email protected] (R.L.) * Author to whom correspondence should be addressed: E-Mail: [email protected]; Tel.: +34 953 212160; Fax: +34 953 212943. Received: 3 July 2010 / Accepted: 9 August 2010 / Published: 10 August 2010 Abstract: Heat-stable enterotoxins are the most notable virulence factors associated with Staphylococcus aureus, a common pathogen associated with serious community and hospital acquired diseases. Staphylococcal enterotoxins (SEs) cause toxic shock-like syndromes and have been implicated in food poisoning. But SEs also act as superantigens that stimulate T-cell proliferation, and a high correlation between these activities has been detected. Most of the nosocomial S. aureus infections are caused by methicillin-resistant S. aureus (MRSA) strains, and those resistant to quinolones or multiresistant to other antibiotics are emerging, leaving a limited choice for their control. This review focuses on these diverse roles of SE, their possible correlations and the influence in disease progression and therapy. Keywords: enterotoxins; Staphylococcus aureus; superantigens; MRSA; immune response 1. Introduction Staphylococcus aureus is a common pathogen associated with serious community and hospital acquired diseases and has for a long time been considered as a major problem of Public Health [1].