Psychiatric-Mental Health Nurse Practitioner Review and Resource Manual, 4Th Edition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1: Clinical Pharmacokinetics 1
1: CLINICAL PHARMACOKINETICS 1 General overview: clinical pharmacokinetics, 2 Pharmacokinetics, 4 Drug clearance (CL), 6 Volume of distribution (Vd), 8 The half-life (t½), 10 Oral availability (F), 12 Protein binding (PB), 14 pH and pharmacokinetics, 16 1 Clinical pharmacokinetics General overview General overview: clinical pharmacokinetics 1 The ultimate aim of drug therapy is to achieve effi cacy without toxicity. This involves achieving a plasma concentration (Cp) within the ‘therapeutic window’, i.e. above the min- imal effective concentration (MEC), but below the minimal toxic concentration (MTC). Clinical pharmacokinetics is about all the factors that determine variability in the Cp and its time-course. The various factors are dealt with in subsequent chapters. Ideal therapeutics: effi cacy without toxicity Minimum Toxic Concentration (MTC) Ideal dosing Minimum Effective Concentration (MEC) Drug concentration Time The graph shows a continuous IV infusion at steady state, where the dose-rate is exactly appropriate for the patient’s clearance (CL). Inappropriate dosing Dosing too high in relation to the patient’s CL – toxicity likely Minimum Toxic Concentration (MTC) Minimum Effective Concentration (MEC) Dosing too low in relation to the Drug concentration patient’s CL – drug may be ineffective Time Some reasons for variation in CL Low CL High CL Normal variation Normal variation Renal impairment Increased renal blood fl ow Genetic poor metabolism Genetic hypermetabolism Liver impairment Enzyme induction Enzyme inhibition Old age/neonate 2 General overview Clinical Pharmacokinetics Pharmacokinetic factors determining ideal therapeutics If immediate effect is needed, a loading dose (LD) must be given to achieve a desired 1 concentration. The LD is determined by the volume of distribution (Vd). -

HALDOL Brand of Haloperidol Injection (For Immediate Release) WARNING Increased Mortality in Elderly Patients with Dementia
HALDOL® brand of haloperidol injection (For Immediate Release) WARNING Increased Mortality in Elderly Patients with Dementia-Related Psychosis Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. HALDOL Injection is not approved for the treatment of patients with dementia-related psychosis (see WARNINGS). DESCRIPTION Haloperidol is the first of the butyrophenone series of major antipsychotics. The chemical designation is 4-[4-(p-chlorophenyl)-4-hydroxypiperidino] 4’-fluorobutyrophenone and it has the following structural formula: HALDOL (haloperidol) is available as a sterile parenteral form for intramuscular injection. The injection provides 5 mg haloperidol (as the lactate) and lactic acid for pH adjustment between 3.0 – 3.6. -

Use of Ceftaroline Fosamil in Children: Review of Current Knowledge and Its Application
Infect Dis Ther (2017) 6:57–67 DOI 10.1007/s40121-016-0144-8 REVIEW Use of Ceftaroline Fosamil in Children: Review of Current Knowledge and its Application Juwon Yim . Leah M. Molloy . Jason G. Newland Received: November 10, 2016 / Published online: December 30, 2016 Ó The Author(s) 2016. This article is published with open access at Springerlink.com ABSTRACT infections, CABP caused by penicillin- and ceftriaxone-resistant S. pneumoniae and Ceftaroline is a novel cephalosporin recently resistant Gram-positive infections that fail approved in children for treatment of acute first-line antimicrobial agents. However, bacterial skin and soft tissue infections and limited data are available on tolerability in community-acquired bacterial pneumonia neonates and infants younger than 2 months (CABP) caused by methicillin-resistant of age, and on pharmacokinetic characteristics Staphylococcus aureus, Streptococcus pneumoniae in children with chronic medical conditions and other susceptible bacteria. With a favorable and those with invasive, complicated tolerability profile and efficacy proven in infections. In this review, the microbiological pediatric patients and excellent in vitro profile of ceftaroline, its mechanism of action, activity against resistant Gram-positive and and pharmacokinetic profile will be presented. Gram-negative bacteria, ceftaroline may serve Additionally, clinical evidence for use in as a therapeutic option for polymicrobial pediatric patients and proposed place in therapy is discussed. Enhanced content To view enhanced content for this article go to http://www.medengine.com/Redeem/ 1F47F0601BB3F2DD. Keywords: Antibiotic resistance; Ceftaroline J. Yim (&) fosamil; Children; Methicillin-resistant St. John Hospital and Medical Center, Detroit, MI, Staphylococcus aureus; Streptococcus pneumoniae USA e-mail: [email protected] L. -
Orphenadrine Hydrochloride 50Mg/5Ml Oral Solution Rare (Affect More Than 1 in 10,000 People) N Forgetting Things More Than Usual
Uncommon (affect more than 1 in 1000 people) n Constipation Package Leaflet: Information for the user n Greater sensitivity to things around you or feeling nervous n Feeling light-headed and an unusual feeling of excitement (elation) n Difficulty sleeping or feeling tired. Orphenadrine Hydrochloride 50mg/5ml Oral Solution Rare (affect more than 1 in 10,000 people) n Forgetting things more than usual. Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. Reporting of side effects n Keep this leaflet. You may need to read it again. If you get any side effects, talk to your doctor, n If you have any further questions, ask your doctor pharmacist or nurse. This includes any possible side or pharmacist. effects not listed in this leaflet. You can also report n This medicine has been prescribed for you only. side effects directly (see details below). By reporting Do not pass it on to others. It may harm them, even side effects you can help provide more information on if their signs of illness are the same as yours. the safety of this medicine. n If you get any side effects, talk to your doctor or United Kingdom pharmacist. This includes any possible side effects not listed in this Yellow Card Scheme leaflet. See section 4. Website: www.mhra.gov.uk/yellowcard or search for MHRA Yellow Card in the Google Play or What is in this leaflet: Apple App Store. 1. What Orphenadrine Hydrochloride Oral Solution is and what is it used for 2. -

HIGHLIGHTS of PRESCRIBING INFORMATION These Highlights Do
HIGHLIGHTS OF PRESCRIBING INFORMATION • Metabolic Changes: Atypical antipsychotic drugs have been associated with These highlights do not include all the information needed to use metabolic changes that may increase cardiovascular/cerebrovascular risk. CLOZARIL safely and effectively. See full prescribing information for These metabolic changes include: CLOZARIL. o Hyperglycemia and Diabetes Mellitus: Monitor for symptoms of CLOZARIL® (clozapine) tablets, for oral use hyperglycemia including polydipsia, polyuria, polyphagia, and Initial U.S. Approval: 1989 weakness. Monitor glucose regularly in patients with diabetes or at risk for diabetes. (5.9) WARNING: SEVERE NEUTROPENIA; ORTHOSTATIC o Dyslipidemia: Undesirable alterations in lipids have occurred in HYPOTENSION, BRADYCARDIA, AND SYNCOPE; SEIZURE; patients treated with atypical antipsychotics. (5.9) MYOCARDITIS AND CARDIOMYOPATHY; INCREASED o Weight Gain: Significant weight gain has occurred. Monitor weight MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA- gain. (5.9) RELATED PSYCHOSIS • Neuroleptic Malignant Syndrome (NMS): Immediately discontinue and See full prescribing information for complete boxed warning. monitor closely. Assess for co-morbid conditions. (5.10) • Fever: Evaluate for infection and for neutropenia, NMS. (5.11) • Pulmonary Embolism (PE): Consider PE if respiratory distress, chest pain, • Severe Neutropenia: CLOZARIL can cause severe neutropenia, which or deep-vein thrombosis occur. (5.12) can lead to serious and fatal infections. Patients initiating and • Anticholinergic Toxicity: Use cautiously in presence of specific conditions continuing treatment with CLOZARIL must have a baseline blood (e.g., narrow angle glaucoma, use of anticholinergic drugs). (5.13) absolute neutrophil count (ANC) measured before treatment initiation • Interference with Cognitive and Motor Performance: Advise caution when and regular ANC monitoring during treatment (2.1, 5.1). -

Comparing the Effect of Venlafaxine and the Combination of Nortriptyline and Propranolol in the Prevention of Migraine
Comparing the Effect of Venlafaxine and the Combination of Nortriptyline and Propranolol in the Prevention of Migraine Arash Mosarrezaii1, Mohammad Reza Amiri Nikpour1, Ata Jabarzadeh2 1Department of Neurology, Imam Khomeini Hospital, Urmia University of Medical Sciences, Urmia, Iran, 2Medical Student, Urmia University of Medical Sciences, Urmia, Iran Abstract Background: Migraine is a debilitating neurological condition, which can be categorized into episodic and chronic groups based on its clinical pattern. Avoiding the risk factors exacerbating migraine is not enough to reduce the frequency and severity of migraine headaches, and in the case of non-receiving proper drug treatment, episodic migraines have the potential to become chronic, which increases the risk of cardiovascular complications RESEARCH ARTICLE and leaves great impact on the quality of life of patients and increasing the health-care costs. The objective of this research was to compare the effects of venlafaxine (VFL) and nortriptyline and propranolol in preventing migraines. Methods: This research is an interventional study performed on 60 patients with migraine admitted to the neurological clinic. Patients were visited at 3 time intervals. In each stage, the variables of headache frequency, headache severity, nausea, vomiting, and drowsiness were recorded. Data were analyzed using SPSS 23 software. Results: VFL drug with a daily dose of 37.5 mg is not only more tolerable in the long term but also leaves better effect in reducing the frequency and severity of headaches compared to the combination of nortriptyline and propranolol. Conclusion: VFL is an appropriate, effective, and tolerable alternative to migraine treatment. Key words: Migraine, nortriptyline, propranolol, venlafaxine INTRODUCTION Patients with CM are less likely to have full-time job than patients with episodic type, and they are at risk of job igraine is known as a common incapacity, anxiety, chronic pain, and depression 2 times neurological disorder and causes more than patients with episodic migraine. -

Narrow Therapeutic Index
Therapeutic Drug Monitoring Some drugs have a narrow therapeutic index, which means that there is only a small difference between the minimum effective concentrations and the minimum toxic concentrations in the blood. With such drugs, small increases in dose or in blood/serum concentrations could lead to toxic effects. Therapeutic drug monitoring may help to optimise treatment in cases where there is a firm relationship between the toxic/therapeutic effects and drug concentrations in whole blood/serum. A therapeutic interval has been defined for the drugs in the following tables. This is the minimum effective and maximum safe concentration for compliant patients, on stabilised regimens. Levels within these limits should prove satisfactory in most cases. Whole blood or serum drug concentrations are useful for determining patient compliance or for assessing whether or not: 1. adequate concentrations are being achieved or, 2. potentially toxic concentrations are being reached. Depending on clinical conditions, dosage adjustments may be needed when levels are outside the therapeutic interval. Therapeutic drug monitoring can also be useful when changes are made to other medications that could affect serum or whole blood concentrations and lead to a reduction in effectiveness or increased toxicity. Although plasma drug concentrations and the therapeutic interval are useful in evaluating drug therapy, they should not be the only criteria on which treatment is based. Always remember to treat the patient, not the level. Drug concentrations in serum or whole blood are only meaningful if the correct procedures are followed regarding the timing of specimens and selection of sample tube. It is vitally important to note the exact time the sample is taken and when each dose of the drug is given. -

Medication: Amitriptyline 10 Mg
Amitriptyline (Elavil) COMPLEX CHRONIC DISEASES PROGRAM Medication Handout Date: May 15, 2018 Medication: Amitriptyline 10 mg What is Amitriptyline? Amitriptyline belongs to a group of medications called tricyclic antidepressants (TCAs) that were first used to treat depression. It works by altering the levels of certain neuro- transmitters in the brain such as noradrenalin and serotonin. They have since been found to be effective for many different uses such as: pain, helping with sleep quality (but is not a sleeping pill), irritable bowel syndrome (with diarrhea), migraine prevention, and interstitial cystitis. Expected Benefit: Usually takes several weeks to notice a benefit You may not notice a benefit until you get to a dose of 25 mg Watch for possible side effects: This list of side effects is important for you to be aware of; however, it is also important to remember that not all side effects happen to all people. Many of these less serious side effects will improve over the first few days of taking the medications. If you have problems with these side effects talk with your doctor or pharmacist: Dry mouth – this is the most common side; the others are much less frequent Hangover effect – too sleepy in the morning Blurred vision Urinary retention, trouble with urination Tiredness, dizziness that is more than usual Diarrhea or constipation Stopping the medication: Do NOT stop taking this medication suddenly without asking your doctor – this medication is usually decreased slowly (at higher doses) before it is stopped completely How to use this medication: Take this medication with or without food Dosing Schedule: Start with 5 mg (½ tablet) 2 hrs before bed Increase dose according to table below Many patients can only tolerate 20 or 30 mg If you don’t have dry mouth or side effects, you can continue slowly increasing the dose to a maximum of 70 mg You can stay at a lower dose (stop increasing) if you get side effects (usually dry mouth). -
Risk Based Requirements for Medicines Handling
Risk based requirements for medicines handling Including requirements for Schedule 4 Restricted medicines Contents 1. Introduction 2 2. Summary of roles and responsibilities 3 3. Schedule 4 Restricted medicines 4 4. Medicines acquisition 4 5. Storage of medicines, including control of access to storage 4 5.1. Staff access to medicines storage areas 5 5.2. Storage of S4R medicines 5 5.3. Storage of S4R medicines for medical emergencies 6 5.4. Access to storage for S4R and S8 medicines 6 5.5. Pharmacy Department access, including after hours 7 5.6. After-hours access to S8 medicines in the Pharmacy Department 7 5.7. Storage of nitrous oxide 8 5.8. Management of patients’ own medicines 8 6. Distribution of medicines 9 6.1. Distribution outside Pharmacy Department operating hours 10 6.2. Distribution of S4R and S8 medicines 10 7. Administration of medicines to patients 11 7.1. Self-administration of scheduled medicines by patients 11 7.2. Administration of S8 medicines 11 8. Supply of medicines to patients 12 8.1. Supply of scheduled medicines to patients by health professionals other than pharmacists 12 9. Record keeping 13 9.1. General record keeping requirements for S4R medicines 13 9.2. Management of the distribution and archiving of S8 registers 14 9.3. Inventories of S4R medicines 14 9.4. Inventories of S8 medicines 15 10. Destruction and discards of S4R and S8 medicines 15 11. Management of oral liquid S4R and S8 medicines 16 12. Cannabis based products 17 13. Management of opioid pharmacotherapy 18 14. -

Adverse Drug Reactions Sample Chapter
Sample copyright Pharmaceutical Press www.pharmpress.com 5 Drug-induced skin reactions Anne Lee and John Thomson Introduction Cutaneous drug eruptions are one of the most common types of adverse reaction to drug therapy, with an overall incidence rate of 2–3% in hos- pitalised patients.1–3 Almost any medicine can induce skin reactions, and certain drug classes, such as non-steroidal anti-inflammatory drugs (NSAIDs), antibiotics and antiepileptics, have drug eruption rates approaching 1–5%.4 Although most drug-related skin eruptions are not serious, some are severe and potentially life-threatening. Serious reac- tions include angio-oedema, erythroderma, Stevens–Johnson syndrome and toxic epidermal necrolysis. Drug eruptions can also occur as part of a spectrum of multiorgan involvement, for example in drug-induced sys- temic lupus erythematosus (see Chapter 11). As with other types of drug reaction, the pathogenesis of these eruptions may be either immunological or non-immunological. Healthcare professionals should carefully evalu- ate all drug-associated rashes. It is important that skin reactions are identified and documented in the patient record so that their recurrence can be avoided. This chapter describes common, serious and distinctive cutaneous reactions (excluding contact dermatitis, which may be due to any external irritant, including drugs and excipients), with guidance on diagnosis and management. A cutaneous drug reaction should be suspected in any patient who develops a rash during a course of drug therapy. The reaction may be due to any medicine the patient is currently taking or has recently been exposed to, including prescribed and over-the-counter medicines, herbal or homoeopathic preparations, vaccines or contrast media. -

Atomoxetine: a New Pharmacotherapeutic Approach in the Management of Attention Deficit/Hyperactivity Disorder
i26 Arch Dis Child: first published as 10.1136/adc.2004.059386 on 21 January 2005. Downloaded from Atomoxetine: a new pharmacotherapeutic approach in the management of attention deficit/hyperactivity disorder J Barton ............................................................................................................................... Arch Dis Child 2005;90(Suppl I):i26–i29. doi: 10.1136/adc.2004.059386 Atomoxetine is a novel, non-stimulant, highly selective lifespan including a potential requirement for lifelong treatment.4 Because of the limitations of noradrenaline reuptake inhibitor that has been studied for existing treatments and the paradigm shift in use in the treatment of attention deficit/hyperactivity thinking about the management of ADHD, there disorder (ADHD). Data from clinical trials show it to be well is an interest in the development of new pharmacological treatments. tolerated and effective in the treatment of ADHD in children, adolescents, and adults. Improvements were seen ATOMOXETINE HYDROCHLORIDE: A not only in core symptoms of ADHD, but also in broader NOVEL TREATMENT FOR ADHD social and family functioning and self esteem. Once-daily Atomoxetine is the first non-stimulant to be approved for the treatment of ADHD and the first dosing of atomoxetine has been shown to be effective in drug to be licensed for the treatment of ADHD in providing continuous symptom relief. Atomoxetine does adults.5 Atomoxetine was licensed in the US in not appear to have abuse potential and is associated with November 2002 and in the UK in May 2004. At the time of writing, it is under consideration for a benign side effect profile. The development of licensing by the regulatory authorities in a atomoxetine thus represents an important advance in the number of other countries. -
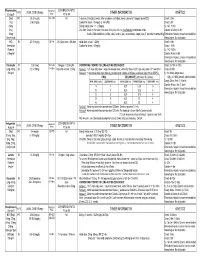
Medication Conversion Chart
Fluphenazine FREQUENCY CONVERSION RATIO ROUTE USUAL DOSE (Range) (Range) OTHER INFORMATION KINETICS Prolixin® PO to IM Oral PO 2.5-20 mg/dy QD - QID NA ↑ dose by 2.5mg/dy Q week. After symptoms controlled, slowly ↓ dose to 1-5mg/dy (dosed QD) Onset: ≤ 1hr 1mg (2-60 mg/dy) Caution for doses > 20mg/dy (↑ risk EPS) Cmax: 0.5hr 2.5mg Elderly: Initial dose = 1 - 2.5mg/dy t½: 14.7-15.3hr 5mg Oral Soln: Dilute in 2oz water, tomato or fruit juice, milk, or uncaffeinated carbonated drinks Duration of Action: 6-8hr 10mg Avoid caffeinated drinks (coffee, cola), tannics (tea), or pectinates (apple juice) 2° possible incompatibilityElimination: Hepatic to inactive metabolites 5mg/ml soln Hemodialysis: Not dialyzable HCl IM 2.5-10 mg/dy Q6-8 hr 1/3-1/2 po dose = IM dose Initial dose (usual): 1.25mg Onset: ≤ 1hr Immediate Caution for doses > 10mg/dy Cmax: 1.5-2hr Release t½: 14.7-15.3hr 2.5mg/ml Duration Action: 6-8hr Elimination: Hepatic to inactive metabolites Hemodialysis: Not dialyzable Decanoate IM 12.5-50mg Q2-3 wks 10mg po = 12.5mg IM CONVERTING FROM PO TO LONG-ACTING DECANOATE: Onset: 24-72hr (4-72hr) Long-Acting SC (12.5-100mg) (1-4 wks) Round to nearest 12.5mg Method 1: 1.25 X po daily dose = equiv decanoate dose; admin Q2-3wks. Cont ½ po daily dose X 1st few mths Cmax: 48-96hr 25mg/ml Method 2: ↑ decanoate dose over 4wks & ↓ po dose over 4-8wks as follows (accelerate taper for sx of EPS): t½: 6.8-9.6dy (single dose) ORAL DECANOATE (Administer Q 2 weeks) 15dy (14-100dy chronic administration) ORAL DOSE (mg/dy) ↓ DOSE OVER (wks) INITIAL DOSE (mg) TARGET DOSE (mg) DOSE OVER (wks) Steady State: 2mth (1.5-3mth) 5 4 6.25 6.25 0 Duration Action: 2wk (1-6wk) Elimination: Hepatic to inactive metabolites 10 4 6.25 12.5 4 Hemodialysis: Not dialyzable 20 8 6.25 12.5 4 30 8 6.25 25 4 40 8 6.25 25 4 Method 3: Admin equivalent decanoate dose Q2-3wks.