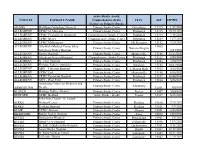
HOSPITAL UNCOMPENSATED CARE PAYMENT and REIMBURSEMENTS for EXTRAORDINARY EXPENSE REPORT
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2022 CASPR Program Summary Chart
AACPM, Office of Graduate Services 9/28/2021 2022 CASPR Program Summary Chart CPME APPROVAL STIPEND PROGRAM NAME PROGRAM FEE Type # Approved # Funded Year One Year Two Year Three Year Four 0514 AdventHealth East Orlando $0.00 PMSR/RRA: 3 3 $55,162 $57,262 $59,342 CRIP: Section 1 0146 Adventist Health White Memorial $0.00 PMSR/RRA: 2 2 $62,487 $63,885 $66,631 CRIP: Section 2 0371 Advocate Christ Medical Center PMSR/RRA: 3 3 $62,000 $63,000 $65,000 CRIP: Unsure 0337 Advocate Illinois Masonic Medical Center and $0.00 PMSR/RRA: 3 3 $53,665 $63,000 $65,000 CRIP: Unsure 0701 Albert Einstein Medical Center PMSR/RRA: 1 1 $59,635 $61,311 $62,723 CRIP: Section 1 0348 AMITA Health Saint Joseph Hospital Chicago $0.00 PMSR/RRA: 5 5 $58,269 $60,485 $62,597 CRIP: Section 2 0349 AMITA Health Saints Mary and Elizabeth Medi $0.00 PMSR/RRA: 1 1 $59,434 $61,695 $63,849 CRIP: Section 2 0445 Ascension Genesys Hospital $0.00 PMSR/RRA: 2 2 $53,974 $56,431 $58,205 CRIP: Section 2 0453 Ascension Macomb Oakland Hospital $0.00 PMSR/RRA: 3 3 $54,619 $55,192 $55,746 CRIP: Section 2 0450 Ascension Providence Hospital Southfield Ca $0.00 PMSR/RRA: 3 3 $53,532 $54,084 $54,636 CRIP: Section 2 0452 Ascension St. John Hospital $0.00 PMSR/RRA: 4 4 $53,532 $54,084 $53,581 CRIP: Section 2 0354 Ascension St. Vincent Hospital Indianapolis $0.00 PMSR/RRA: 4 4 $57,288 $57,769 $58,906 CRIP: Section 2 0361 Ascension Wisconsin Hospital $0.00 PMSR/RRA: 3 3 $62,740 $63,850 $64,970 CRIP: Section 2 0456 Aultman Alliance Community Hospital $0.00 PMSR/RRA: 3 3 $53,350 $54,120 $55,000 CRIP: -

Designated Acute Care Hospital Stroke Centers 180424
Acute Stroke -ready; Comprehensive stroke COUNTY FACILITY NAME CITY ZIP Center or Primary Stroke Center? MONTGOMERY Abington Memorial Hospital Comprehensive stroke Center Abington 19001 ALLEGHENY Allegheny General Hospital Comprehensive Stroke Center Pittsburgh 15212 CUMBERLAND Carlisle Regional Medical Center Primary Stroke Center Carlisle 17015 FRANKLIN Chambersburg Hospital Primary Stroke Center Chambersburg 17201 CHESTER Chester County Hospital – Chester County Primary Stroke Center West Chester 19380 CAMBRIA Conemaugh Memorial Medical Center Primary Stroke Center Johnstown 15905 BLAIR Conemaugh Nason Medical Center Acute Stroke -ready Roaring Spring 16673 BUCKS Doylestown Hospital Primary Stroke Center Doylestown 18901 MONTGOMERY Einstein Medical Center Montgomery Primary Stroke Center East Norriton 19403 LANCASTER Ephrata Community Hospital Primary Stroke Center Ephrata 17522 WESTMORELAND Excela Health Frick Hospital Primary Stroke Center Westmoreland 15666 WESTMORELAND Excela Health Latrobe Hospital Primary Stroke Center Latrobe 15650 WESTMORELAND Excela Health Westmoreland Hospital Primary Stroke Center Greensburg 15601 LACKAWANNA Geisinger Community Medical Center – Scranton - Lackawanna County Primary Stroke Center Scranton 18510 MONTOUR Geisinger Medical Center – Montour County Primary Stroke Center Danville 17822 LUZERNE Geisinger Wyoming Valley Medical Center, Wilkes-Barre – Luzerne County Primary Stroke Center Wilkes Barre 18711 ADAMS Gettysburg Hospital Primary Stroke Center Gettysburg 17325 CARBON Gnadden Huetten Memorial -

HMO Proactive Tiered Network Hospital List
Save with Keystone HMO Proactive, our most popular plans Keystone HMO Proactive health plans are our most popular for good reason: You get access to high-quality care and save money. Not only do you pay less for your monthly premiums, but you can save even more by choosing doctors and hospitals in Tier 1 – Preferred. Save with Tier 1 – Preferred Tier 1 – Preferred includes more than 50 percent of the network. Keystone HMO Proactive offers the same essential health benefits as our other health plans, including doctor visits, Tier 1 – Preferred hospital stays, prescription drug coverage, blood tests, and X-rays. The difference is its tiered provider network, which gives you the option to pay less for care by choosing Tier 1 –Preferred providers. Here are the most important things to know about Keystone HMO Proactive: • You can visit any doctor or hospital in the Independence Blue Cross network once you have a referral. Tier 2 – Enhanced Tier 3 – Standard • You will select a PCP to coordinate your care and refer you to specialists. • Some services cost the same no matter what provider you Save even more choose — like preventive care, emergency room visits, and Keystone HMO Silver Proactive Select and Keystone HMO Silver urgent care. Proactive Value: These lower-premium options are only available • When you use doctors and hospitals in Tier 1 – Preferred, when you purchase directly from Independence Blue Cross. you pay the lowest out-of-pocket costs. Keystone HMO Silver Proactive Value includes a deductible for • The choice is always yours. You can choose Tier 1 providers Tiers 1 – 3 for some services. -

Public Health the Hospital of the Fox Chase Cancer
PUBLIC HEALTH management corporation THE HOSPITAL OF THE FOX CHASE CANCER CENTER COMMUNITY HEALTH NEEDS ASSESSMENT PREPARED FOR: THE HOSPITAL OF THE FOX CHASE CANCER CENTER PREPARED BY: PUBLIC HEALTH MANAGEMENT CORPORATION 260 SOUTH BROAD STREET, 18TH FLOOR PHILADELPHIA, PA 19102 APRIL 2013 PUBLIC HEALTH management corporation TABLE OF CONTENTS I. INTRODUCTION ................................................................................................................................. 1 ABOUT THE HOSPITAL OF THE FOX CHASE CANCER CENTER ......................................................................... 1 PURPOSE AND METHODOLOGY ............................................................................................................... 1 COMMUNITY DEFINITION ....................................................................................................................... 6 COMMUNITY DEMOGRAPHICS ................................................................................................................ 8 EXISTING HEALTH CARE RESOURCES ...................................................................................................... 12 II. PROCESS AND METHODS ................................................................................................................. 13 DATA ACQUISITION AND ANALYSIS ........................................................................................................ 13 COMMUNITY REPRESENTATIVES ........................................................................................................... -

Acute-Care-Hospitals-Alphabetic.Pdf
Acute Care Hospitals Facility Name Facility # Facility Name Facility # Abington Health Center - Warminster 1410-09 Barnabas Health Jersey City Medical Center 2312-70 Campus(Warminster Hospital) Barnes-Kasson Hospital 1241-58 Abington Health-Lansdale Hospital 1432-46 Barnesville Hospital - Barnesville 1012-72 Abington Memorial Hospital 1001-46 Bath VA Medical Center 1062-71 Acuity Specialty Hospital of New Jersey (LTAC) 2310-70 (within Atlanticare Reg. Med.Ctr. Atlantic City Bayhealth Hospital, Sussex Campus 1012-68 Campu Bayshore Community Hospital 1039-70 AHN Harmar Neighborhood Hospital 1465-02 Beebe Medical Center - Lewes, DE 1003-68 AHN Hempfield Neighborhood Hospital 1130-65 Bellevue Hospital Center- New York, NY 1012-71 AHN McCandless Neighborhood Hospital 1464-02 Belmont Community Hospital (The Bellaire City 1002-72 AHN Neighborhood Hospital - Brentwood 1463-02 Hospital) Akron General Medical Center 1033-72 Belmont Hospital Bel Air 1026-72 Albany Medical Center Hospital - Albany, NY 1043-71 Benedictine Hospital 1001-71 Aliquippa Community Hospital (UPMC Beaver 1002-04 Berwick Hospital Center 1013-19 Valley Hospital) Beth Israel Hospital - Newark 1035-70 Allegheny General Hospital 1184-02 Beth Israel Med Ctr-Petrie Division (Manhattan) 1057-71 Allegheny Valley Hospital (Alle-Kiski Medical 1124-02 Center) Bloomsburg Hospital 1016-19 Anne Arundel Medical Center 1035-69 Bluefield Regional Medical Center 1029-73 Ardern Hill Hospital - Goshen 1017-71 Blythedale Children's Hospital 1063-71 Aria Health - Bucks County (formerly Delaware -
Ready; Comprehensive Stroke Center
Acute Stroke -ready; COUNTY FACILITY NAME Comprehensive stroke CITY ZIP EXPIRES Center; or Primary Stroke ADAMS WellSpan Gettysburg Hospital Primary Stroke Center Gettysburg 17325 1/22/2024 ALLEGHENY UPMC St. Margaret Primary Stroke Center Pittsburgh 15215 10/20/2022 ALLEGHENY UPMC Presbyterian Shadyside Comprehensive Stroke Center Pittsburgh 15213 7/18/2021 ALLEGHENY UPMC Mercy Comprehensive Stroke Center Pittsburgh 15219 12/7/2021 ALLEGHENY UPMC McKeesport Primary Stroke Center Mc Keesport 15132 7/20/2021 ALLEGHENY Alle-Kiski Medical Center d/b/a/ 15065 Primary Stroke Center Natrona Heights Allegheny Valley Hospital 3/14/2021 ALLEGHENY Forbes Hospital Primary Stroke Center Monroeville 15146 11/17/2022 ALLEGHENY Allegheny General Hospital Comprehensive Stroke Center Pittsburgh 15212 3/20/2021 ALLEGHENY St. Clair Hospital Primary Stroke Center Pittsburgh 15243 2/24/2023 ALLEGHENY Heritage Valley - Swickley Primary Stroke Center Swickley 15143 10/17/2021 ALLEGHENY AHN - Jefferson Hospital Primary Stroke Center Jefferson Hills 15025 3/13/2023 ALLEGHENY UPMC East Primary Stroke Center Monroeville 15146 6/16/2023 ALLEGHENY UPMC Passavant Hospital Primary Stroke Center Pittsburgh 15237 10/28/2022 ALLEGHENY AHN - West Penn Primary Stroke Center Pittsburgh 15224 5/26/2021 Armstrong Center for Medicine and Primary Stroke Center Kittanning ARMSTRONG Health 16201 3/8/2022 BEAVER Heritage Valley - Beaver Primary Stroke Center Beaver 15009 10/4/2021 BEDFORD UPMC Bedford Acute Stroke - Ready Everett 15537 6/25/2021 Penn State Health - St. Joseph BERKS Medical Center Primary Stroke Center Reading 19610 7/24/2022 BERKS Reading Hospital Primary Stroke Center Reading 19611 9/9/2021 BLAIR UPMC Altoona Primary Stroke Center Altoona 16601 5/15/2023 BRADFORD Robert Packer Hospital Primary Stroke Center Sayre 18840 12/5/2022 BUCKS Doylestown Hospital Primary Stroke Center Doylestown 18901 3/5/2021 BUCKS Grand View Hospital Primary Stroke Center Sellersville 18960 11/4/2022 BUCKS St. -

Accredited Primary Stroke Centers
Accredited Primary Stroke Centers County Facility Name City Zip Montgomery Abington Memorial Hospital Abington 19001 Armstrong ACMH – Armstrong County Kittanning 16201 Philadelphia Albert Einstein Med. Center Philadelphia 19141 Allegheny Allegheny General Hospital Pittsburgh 15212 Bucks Aria Health – Bucks County Campus – Bucks County Langhorne 19047 Philadelphia Aria Health – Frankford Campus – Philadelphia County Philadelphia 19124 Philadelphia Aria Health – Torresdale Campus – Philadelphia County Philadelphia 19114 Chester Brandywine Hospital Coatesville 19320 Mercer Co., NJ Capital Health Medical Center – Hopewell New Jersey – Mercer Co., New Jersey Pennington NJ 8534 Mercer Co., NJ Capital Health Regional Medical Center – Trenton New Jersey – Mercer Co., NJ Trenton NJ 8638 Franklin Chambersburg Hospital Chambersburg 17201 Chester Chester County Hospital – Chester County West Chester 19380 Philadelphia Chestnut Hill Hospital Philadelphia 19118 Cambria Conemaugh Memorial Medical Center Johnstown 15905 Delaware Crozer Chester Medical Center, Taylor Ridley Park 19078 Delaware Crozer Chester Medical Center, Upland Upland 19013 Delaware Delaware County Memorial Hospital Drexel Hill 19026 Bucks Doylestown Hospital Doylestown 18901 Northampton Easton Hospital Easton 18042 Montgomery Einstein Medical Center Montgomery East Norriton 19403 Lancaster Ephrata Community Hospital Ephrata 17522 Union Evangelical Community Hospital Lewisburg 17837 Allegheny Forbes Hospital Monroeville 15146 Lackawanna Geisinger Community Medical Center – Scranton -

Keystone HMO Proactive Hospital Tier Placements
Keystone HMO Proactive hospital tier placements Tier 1 – Preferred $ Pennsylvania New Jersey Bucks Montgomery Burlington Aria Health — Bucks County Campus Abington Memorial Hospital Deborah Heart & Lung Center Doylestown Hospital Albert Einstein Medical Center — Virtua Willingboro Hospital Grand View Hospital Montgomery Campus Camden Lower Bucks Hospital Holy Redeemer Hospital and Medical Center Cooper Hospital University Medical Center Rothman Orthopaedic Specialty Hospital Lansdale Hospital St. Luke’s Health Network — Quakertown Campus Suburban Community Hospital Mercer Tower Health — Pottstown Memorial Robert Wood Johnson University Hospital Chester Medical Center at Hamilton Chester County Hospital St. Francis Medical Center Tower Health — Brandywine Hospital Philadelphia Tower Health — Jennersville Regional Hospital Albert Einstein Medical Center Salem Tower Health — Phoenixville Hospital Albert Einstein Medical Center — Memorial Hospital of Salem County Delaware Germantown Campus Warren Crozer-Chester Medical Center Aria Health — Frankford Campus Hackettstown Community Hospital Delaware County Memorial Hospital Aria Health — Torresdale Campus Springfield Hospital Jeanes Hospital Taylor Hospital Roxborough Memorial Hospital Tower Health — Chestnut Hill Hospital Lehigh Wills Eye Hospital St. Luke’s Health Network — Allentown Campus St. Luke’s Health Network — Bethlehem Campus Tier 2 – Enhanced $$ Pennsylvania New Jersey Delaware Philadelphia Camden New Castle Children’s Hospital of Philadelphia Virtua Our Lady of Lourdes Hospital A.I. DuPont Hospital for Children Fox Chase Cancer Center Gloucester St. Christopher’s Hospital for Children Inspira Medical Center — Woodbury Shriner’s Hospital for Children Tier 3 – Standard $$$ Pennsylvania New Jersey Berks Montgomery Burlington Salem St. Joseph Medical Center Main Line Health — Bryn Mawr Virtua Marlton Hospital Inspira Medical Center — Elmer Tower Health — Reading Hospital and Hospital Virtua Memorial Hospital Warren Medical Center Main Line Health — Lankenau Camden St. -

The Hospitals Listed Here Push Hard to Make Sure Their Heart Disease and Stroke Patients Get the Benefits of Up-To-Date Scientific Guidelines-Based Treatment
WHEN HOSPITALS GO THE EXTRA MILE, PATIENTS DO TOO The hospitals listed here push hard to make sure their heart disease and stroke patients get the benefits of up-to-date scientific guidelines-based treatment. How? By actively participating in our healthcare quality programs. We thank them for all they do to get patients back on track. One day, you might too. Learn more at Heart.org/USNWR2015. A BIG THANKS TO OUR SPONSORS We appreciate these sponsors for funding our healthcare quality programs and for respecting our clinical independence. AWARD LEVELS SILVER ACHIEVEMENT These hospitals are recognized for 12 consecutive months of 85% or higher adherence on all achievement measures applicable to atrial fibrillation (AFIB) GOLD PLUS ACHIEVEMENT GOLD ACHIEVEMENT SILVER PLUS ACHIEVEMENT SILVER ACHIEVEMENT These hospitals are recognized for two These hospitals are These hospitals are recognized for These hospitals are or more consecutive years of 85% or recognized for two or more 12 consecutive months of 85% or recognized for 12 consecutive higher adherence on all achievement consecutive years of 85% higher adherence on all achievement months of 85% or higher measures applicable and 75% or higher or higher adherence on all measures applicable and 75% or higher adherence on all achievement adherence with four or more select achievement measures adherence with four or more select measures applicable to heart quality measures in heart failure (HF) applicable to heart failure (HF) quality measures in heart failure (HF) failure (HF) GOLD ACHIEVEMENT -

Save with Keystone HMO Proactive
Save with Keystone HMO Proactive Keystone HMO Proactive health plans use a tiered network, so you save on monthly premiums. Plus, you have the option to save even more on your out-of-pocket costs each time you receive covered services. How you’ll save Tier 1 – Preferred Like a typical HMO, you select a primary care physician who can refer you to specialists. You can visit any doctor or hospital in the Keystone Health Plan East network. We grouped our network into three tiers based on cost and, in many cases, quality measures. While all of the doctors and hospitals in our network must meet high quality standards, many offer services at a lower cost. You’ll pay the lowest out-of-pocket costs when you visit doctors Tier 2 – Enhanced Tier 3 – Standard and hospitals in Tier 1 – Preferred, which includes more than 50 percent of doctors and hospitals in the Keystone Health Plan East network. But the choice is always yours, and you can choose Tier 1 – Preferred for some services, and Tiers 2 or 3 for others. Also keep in mind: 50% of doctors and hospitals are • For some services, your out-of-pocket costs are the same in Tier 1 – Preferred. no matter what doctor or hospital you use, including preventive care, emergency room visits, and urgent care. Visit ibx.com/providerfinder, and select • For some services, like surgery, you pay out-of-pocket Keystone HMO Proactive under Your costs for both the facility and the performing doctor. To save the most money, you’ll want to make sure both Plan to find Tier 1 providers and save. -

Press Release
PRESS RELEASE GPBCH Leapfrog Efforts Significantly Increase Transparency on Hospital Safety Hospital Reporting Has Increased Eight-fold Since 2012 PHILADELPHIA, PA—(October 12, 2015)— The Greater Philadelphia Business Coalition on Health (GPBCH) is signiFicantly improving transparency of hospital safety inFormation by serving as the “regional roll-out” For the LeapFrog Group’s hospital survey – a national initiative that encourages hospitals to voluntarily disclose data on safety practices and outcomes. Since GPBCH began its LeapFrog initiative in 2012 For southeastern Pennsylvania and Delaware, the number oF hospitals in the region that report their data has increased eight-Fold From 3 to 24 (out oF 55). (New Jersey’s LeapFrog eFForts are coordinated by the New Jersey Health Care Quality Institute). This national survey collects and publicly reports inFormation on hospital safety, quality, and value in a standardized manner, so that purchasers and consumers can make valid comparisons and use inFormation to select a provider. Research also has shown that hospitals that publicly report their data are more likely to improve on the reported measures. According to Neil GoldFarb, President and CEO oF GPBCH, “While we continue to recognize the hospitals that report LeapFrog data, we now are getting valuable insights into care processes and outcomes through the data that have been reported. For example, the 2015 LeapFrog data reported to date for our region show that 71% oF the reporting hospitals Fully meet the LeapFrog standards For computerized -
100% Smokefree U.S. Hospital Campuses and Psychiatric Facilities
100% Smokefree U.S. Hospital Campuses and Psychiatric Facilities “A tobacco free campus fits with our mission as advocates for the health of our patients, their families and our employees. The expansion of our tobacco-free policy is another way our hospital is demonstrating its commitment to making our community healthier. Our hope is that this policy will help safeguard the health of our patients, employees and visitors.” — David Castleberry, CEO Upson Regional Medical Center 100% Smokefree U.S. Hospital Campuses and Psychiatric Facilities July 1, 2021 HOSPITAL CAMPUSES – REPRESENTATIVE STATE LAWS (UPDATED APRIL 3, 2017) In July 2013, New York State enacted a law requiring 100% smokefree grounds of general hospitals. In April, 2016, Hawaii enacted a law requiring 100% tobacco- and e-cigarette-free grounds of Hawaii Health Systems Corporation state health facility properties. HOSPITAL CAMPUSES – REPRESENTATIVE MUNICIPAL LAWS (UPDATED APRIL 3, 2017) In addition, below is a sampling of 44 municipalities found to have enacted laws as of April 2017 specifically requiring 100% smokefree hospital campuses. Municipality State Description 1. Juneau AK 4/07: Tobacco use prohibited on hospital grounds, including parking areas and adjacent streets and sidewalks. 2. Fort Payne AL 2/09: Smoking prohibited on hospital grounds. 3. Belmont CA 10/07: Smoking prohibited in indoor and outdoor public places generally. 4. Calabasas CA 2/06: Smoking prohibited in indoor and outdoor public places generally. 5. Carpinteria CA 2/11: Smoking prohibited in indoor and outdoor public places generally. 6. Contra Costa CA 10/06: Smoking prohibited on grounds of County hospitals and health clinics.