Case 2:20-Cv-01113-GJP Document 277 Filed 12/08/20 Page 1 of 62
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PPC-Infographic.Pdf
Celebrating our 15th anniversary, Partnership for Patient Care (PPC) is the region’s premier patient safety and quality program driving health equity and high quality outcomes. 115th5th Anniversary 2006 – 2021 WHAT IS PARTNERSHIP FOR PATIENT CARE? Partnership for Patient Care (PPC) is a collaboration between Independence Blue Cross, Health Care Improvement Foundation and the region’s leading healthcare organizations and stakeholders to accelerate the adoption of evidence-based clinical best practices. PPC’s improvement efforts have enabled the region to foster partnerships among organizations that share a common desire for providing the safest and highest quality care to patients. PPC serves as an umbrella, under which several programs have been established during the past 15 years to support ongoing regional improvement. PPC PROGRAMS Health Equity Data Strategy (HEDS) NEW New in 2021, HEDS is a regional collaborative aimed at decreasing disparities in health outcomes with a focus on establishing recommendations for the implementation of a health equity data strategy. This program will support organizations in the accurate and reliable collection of REaL (ethnicity, and language) data, utilization of the data to evaluate health outcomes, identification of disparities across populations and health conditions; and implementation of targeted quality improvement strategies that promote health equity. Safety Forum 100% A forum of front-line patient safety leaders from hospitals across Southeastern PA that of participants rated promotes interactive discussions about safety hazards and vulnerabilities and a peer- the program as very good or excellent to-peer exchange of patient safety approaches, processes, and best practices. Pennsylvania Urologic Regional Collaborative (PURC) 142 PURC is a quality improvement initiative that brings urology practices together in a physician- participating physicians led, data-sharing and improvement collaborative aimed at advancing the quality of diagnosis 17,000+ and care for men with prostate cancer. -

PEAES Guide: Philadelphia Contributionship
PEAES Guide: Philadelphia Contributionship http://www.librarycompany.org/Economics/PEAESguide/contribution.htm Keyword Search Entire Guide View Resources by Institution Search Guide Institutions Surveyed - Select One Philadelphia Contributionship 212 South Fourth Street Philadelphia, PA 19106 (215) 627-1752 Contact Person: Carol Wojtowicz Smith, Curator/Archivist, [email protected] Overview: In 1752, Benjamin Franklin brought together a group of Philadelphians to create the first North American property insurance company. They met at the Widow Pratt's (The Royal Standard Tavern on Market Street), selected two surveyors, and laid down rules stipulating that at least one of them survey each house and write up reports that would be discussed by the entire Board, which would make decisions about the extent and rate of insurance. Franklin named the company The Philadelphia Contributionship for the Insurance of Houses from Loss by Fire. Already in 1736 he had helped to found Philadelphia's first fire brigade, the Union Fire Company. The Contributinship was a mutual insurance company that pooled risks. They based its method of operation (and name) on that of the Amicable Contributionship of London, founded in 1696. The new company was conservative in its underwriting, sending surveyors to inspect each building before insuring it. Accepted properties sported fire marks: four clasped gilded hands mounted on wood plaques. The actual cost of the survey was presumably deducted from the 10 shillings earnest money paid by every person insuring in the society. This also covered the costs of the policy and the "badge" or fire mark. Insurance at this time was limited to properties in Pennsylvania located within a ten mile radius from the center of Philadelphia. -

Pennsylvania Hospital Campus
Diabetes Education Main Entrance 2nd Floor McClelland Conference Center South Gatehouse 1st Floor Great Court Administration Bargain Shop AYER 2nd Floor Historic Library North Gatehouse 3rd Floor Surgical Amphitheatre Medical Volunteer Services PINE BUILDING Library Emergency Department Entrance 9 TH STREET WIDENER Physician Oces Admissions Outpatient Laboratories 8 TH STREET CATHCART Emergency Department Outpatient Registration SPRUCE STREET Radiology Gift Shop Pennsylvania Hospital SCHIEDT Women’s Imaging Center Chapel 800 Spruce Street PRESTON Cafeteria Welcome Center Patient and Guest Services Zubrow Auditorium Philadelphia, PA 19107 Women’s Imaging Center ATM Building Location Map MAIN CAMPUS/FLOOR PLAN on reverse side. EMERGENCY FLOOR/ FLOOR/ 9th Street ENTRANCE DESTINATION BUILDING DESTINATION BUILDING (AMBULANCES) Medical Records/ Cardiac Radiology Film Library 1/Preston Catheterization B/Schiedt Widener Schiedt Outpatient Pharmacy 1/Preston Emergency Cheston Department 1/Schiedt EMERGENCY Conference Room 2/Preston Heart Station 3/Schiedt DEPARTMENT Intensive Care Nursery 2/Preston Critical Care 3/Schiedt EMERGENCY 2nd Floor ENTRANCE Labor and Delivery 3/Preston Observation Unit 4/Schiedt McClelland Conference Center Scheidt Elevators Rooms 450–467 4/Preston Dialysis 4/Schiedt Widener Elevators Rooms 550–567 5/Preston Rooms 500–516 5/Schiedt Pine Rooms 650–668 6/Preston Rooms 600–617 6/Schiedt X-Ray Rooms 750–767 7/Preston Rooms 700–717 7/Schiedt Building Pre-Admission Testing Cashier 1/Cathcart Discharge Unit 9/Schiedt 1st Floor -

2020 List of Hospital Electronic Medical Records (EMR) Connected to Outpatient Dialysis Clinics in the Network 4 Service Area
2020 List of Hospital Electronic Medical Records (EMR) Connected to Outpatient Dialysis Clinics in the Network 4 Service Area A Abington Jefferson Health: Abington-Lansdale and Abington Hospitals. Other network hospitals may be connected. Albert Einstein Medical Center Alleghany Health Network: Alleghany General, Jefferson, St. Vincent and West Penn Hospitals. Other network hospitals may be connected Aria-Jefferson Health: Jefferson Torresdale Hospital Armstrong County Memorial Hospital B Bayhealth: Kent General Hospital (Delaware) Butler Health System: Butler Memorial Hospital C Chestnut Hill Hospital Children's Hospital of Philadelphia Christiana Hospital (Delaware) Commonwealth Health System: Wilkes Barre General Conemaugh Health System: Conemaugh Memorial Medical Center Crozer Chester Medical Center D -E-F-G Doylestown Health: Doylestown Hospital Ephrata Excela Health: Latrobe and Westmoreland Hospitals. Other network hospitals may be connected. Geisinger: Danville, Geisinger Community Medical Center, Holy Spirit, Lewistown and Wyoming Valley Hospitals Grandview Hospital Guthrie Towanda Memorial Hospital H-I-J Heritage Valley Health System: Beaver and Sewickley Hospitals Holy Redeemer Hospital Indiana Regional Medical Center Jennersville Regional Hospital L-M-N-O Lancaster General Health: Lancaster General Hospital Lankenau Medical Center Revised 3/11/20 Page 1 2020 List of Hospital Electronic Medical Records (EMR) Connected to Outpatient Dialysis Clinics in the Network 4 Service Area Lehigh Valley Health Network: Bethlehem, Hazleton, Lehigh Valley and Pocono Hospitals. Other network hospitals may be connected. Main Line Health: Riddle Memorial Hospital Memorial Medical Center Mercy Catholic Medical Center: Mercy Fitzgerald Hospital P Penn Highlands Healthcare: Brookville, Clearfield and Dubois Penn Medicine: Pennsylvania Hospital Penn State Health: St. Joseph's Medical Center Phoenixville Hospital Pottstown Hospital Punxsutawney Area Hospital Q-R-S Reading Hospital Sharon Regional Medical Center St. -
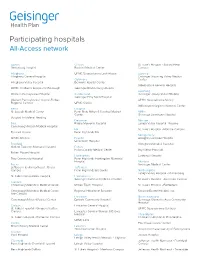
Participating Hospitals All-Access Network
Participating hospitals All-Access network Adams Clinton St. Luke’s Hospital - Sacred Heart Gettysburg Hospital Bucktail Medical Center Campus Allegheny UPMC Susquehanna Lock Haven Luzerne Allegheny General Hospital Geisinger Wyoming Valley Medical Columbia Center Allegheny Valley Hospital Berwick Hospital Center Wilkes-Barre General Hospital UPMC Children’s Hospital of Pittsburgh Geisinger Bloomsburg Hospital Lycoming Western Pennsylvania Hospital Cumberland Geisinger Jersey Shore Hospital Geisinger Holy Spirit Hospital Western Pennsylvania Hospital-Forbes UPMC Susquehanna Muncy Regional Campus UPMC Carlisle Williamsport Regional Medical Center Berks Dauphin St. Joseph Medical Center Penn State Milton S Hershey Medical Mifflin Center Geisinger Lewistown Hospital Surgical Institute of Reading Delaware Monroe Blair Riddle Memorial Hospital Lehigh Valley Hospital - Pocono Conemaugh Nason Medical Hospital Elk St. Luke’s Hospital - Monroe Campus Tyrone Hospital Penn Highlands Elk Montgomery UPMC Altoona Fayette Abington Lansdale Hospital Uniontown Hospital Bradford Abington Memorial Hospital Guthrie Towanda Memorial Hospital Fulton Fulton County Medical Center Bryn Mawr Hospital Robert Packer Hospital Huntingdon Lankenau Hospital Troy Community Hospital Penn Highlands Huntingdon Memorial Hospital Montour Bucks Geisinger Medical Center Jefferson Health Northeast - Bucks Jefferson Campus Penn Highlands Brookville Northampton Lehigh Valley Hospital - Muhlenberg St. Luke's Quakertown Hospital Lackawanna Geisinger Community Medical Center St. Luke’s Hospital - Anderson Campus Cambria Conemaugh Memorial Medical Center Moses Taylor Hospital St. Luke’s Hospital - Bethlehem Conemaugh Memorial Medical Center - Regional Hospital of Scranton Steward Easton Hospital, Inc. Lee Campus Lancaster Northumberland Conemaugh Miners Medical Center Ephrata Community Hospital Geisinger Shamokin Area Community Hospital Carbon Lancaster General Hospital St. Luke’s Hospital - Gnaden Huetten UPMC Susquehanna Sunbury Campus Lancaster General Women & Babies Hospital Philadelphia St. -

Employee Handbook
Employee Handbook You and Jefferson Thomas Jefferson University & Hospitals Stephen K. Klasko, MD, MBA President and CEO Thomas Jefferson University and Jefferson Health System Dear Colleague, Welcome to Thomas Jefferson University and Hospitals! In accepting your new position, you have joined a team committed to redefining healthcare. With a robust history and community roots dating back to 1824, Jefferson is a nationally influential and widely respected academic medical center. We deliver high quality, personalized and compassionate care, and you are now a vital part of our tradition of excellence. By selecting Jefferson, you will enjoy competitive pay, a broad selection of employee benefits from which to choose, opportunity for educational and developmental growth, and a challenging and interactive work environment. Congratulations and my best wishes as you assume your new responsibilities at Jefferson. Sincerely, Stephen K. Klasko, MD, MBA President and CEO Thomas Jefferson University and Jefferson Health System About This Handbook This employee handbook has been designed to provide you with general information about various policies, benefits, services and facilities of Jefferson which may be of interest to you in the course of your employment. Please understand that it only highlights these topics. More specific information may be obtained from your supervisor, the hospital intranet, where any specific policies cited here may be found or the Department of Human Resources at Suite 2150 Gibbon Building or Methodist Administration Suite. You are strongly encouraged to become acquainted with all Jefferson policies and procedures to make your employment as satisfying and productive as possible. The policies, procedures and benefits described in this handbook are not all-inclusive and may be amended or rescinded from time to time at the discretion of Jefferson, with or without notice. -

Temple Health Magazine
LEWIS KATZ SCHOOL OF MEDICINE AT TEMPLE UNIVERSITY | TEMPLE UNIVERSITY HEALTH SYSTEM WINTER 2021 CONQUERING THE CLOT Tackling Thrombosis with Technology and Tenacity COVID-19 AT TEMPLE: STORIES UNMASKED SEPSIS: INSIGHTS, INNOVATIONS AGENDA Temple Health Magazine EDITOR Giselle Zayon [email protected] Health Magazine DESIGN & ART DIRECTION B&G Design Studios WRITERS & CONTRIBUTORS TKarenemple Brooks HealthMagazine Christopher Guadagnino Meredith Mann Jennifer Reardon Andrew Smith Jeremy Walter BUSINESS MANAGER Younndia Rush ADMINISTRATION Christopher Guadagnino, PhD Director, Communications Anne Carlin Practical Wisdom Director, Alumni Relations CONTACT US n the spring of 2020, when the City of Philadelphia needed a large indoor Office of Communications space to convert to a field hospital during the COVID-19 pandemic, any 3509 N. Broad Street Philadelphia, PA 19140 number of complexes in town could have sufficed — but Temple was the 215-707-4839 only organization to answer that call, lending the City its 340,000- square-foot Liacouras Center (page 18). TempleHealth.org IIn 2017, a Temple physician named Riyaz Bashir, MD, was frustrated. Not a 1-800-TEMPLEMED single catheter on the market could do what he needed a catheter to do, so he Lewis Katz School of Medicine Temple University Hospital designed one himself. Now the unique tool — designed to instantly restore blood Temple University Hospital flow through blood clots — is poised for worldwide use (pages 12 and 44). There’s Episcopal Campus Temple University Hospital been lots of practical Temple thinking about blood clots: the namesake of the Jeanes Campus Temple University Hospital university’s Thrombosis Research Center — Sol Sherry, MD (1916-1993) — Northeastern Campus basically invented the field of using enzymes to melt clots (pages 12 and 46). -

Temple University Health System Table of Contents
Temple University Health System Table of Contents 1. Temple University Hospital Community Commitment 2. Programs to Promote Access to Care and Improve Community Health 3. Community Health Needs Assessment Summary 4. Plan to Improve Health of Moms and Newborns 5. Plan to Address Obesity and Overweight BMI 6. Plan to Improve Heart and Vascular Health 7. Plan to improve Access to Mental Health Resources 8. Plan to Strengthen Awareness of Gun Violence 9. Plan to Strengthen Practices for Culturally Competent Care 10.Approach to Unmet Needs 11.Looking Forward to a Healthier Population Temple University Hospital Community Commitment Temple University Hospital was founded in 1892 as “Samaritan Hospital,” with the mission of caring for patients with limited incomes and ensuring access to medical care in its surrounding neighborhoods. Today, Temple University Hospital is a 714-bed non-profit acute care hospital that provides a comprehensive range of medical services to its North Philadelphia neighborhoods, as well as a broad spectrum of secondary, tertiary, and quaternary care to patients throughout Southeastern Pennsylvania. Temple University Hospital serves one of our nation’s most economically challenged and diverse urban populations. About 84% of the patients served by Temple University Hospital are covered by government programs, including 31% by Medicare and 53% by Medicaid. We are an indispensable provider of health care in the largest city in America without a public hospital. Among Pennsylvania’s full-service safety-net providers, Temple University Hospital serves the greatest volume and highest percentage of patients covered by Medicaid. Temple University Hospital also serves as a critical access point for vital public health services. -

2022 CASPR Program Summary Chart
AACPM, Office of Graduate Services 9/28/2021 2022 CASPR Program Summary Chart CPME APPROVAL STIPEND PROGRAM NAME PROGRAM FEE Type # Approved # Funded Year One Year Two Year Three Year Four 0514 AdventHealth East Orlando $0.00 PMSR/RRA: 3 3 $55,162 $57,262 $59,342 CRIP: Section 1 0146 Adventist Health White Memorial $0.00 PMSR/RRA: 2 2 $62,487 $63,885 $66,631 CRIP: Section 2 0371 Advocate Christ Medical Center PMSR/RRA: 3 3 $62,000 $63,000 $65,000 CRIP: Unsure 0337 Advocate Illinois Masonic Medical Center and $0.00 PMSR/RRA: 3 3 $53,665 $63,000 $65,000 CRIP: Unsure 0701 Albert Einstein Medical Center PMSR/RRA: 1 1 $59,635 $61,311 $62,723 CRIP: Section 1 0348 AMITA Health Saint Joseph Hospital Chicago $0.00 PMSR/RRA: 5 5 $58,269 $60,485 $62,597 CRIP: Section 2 0349 AMITA Health Saints Mary and Elizabeth Medi $0.00 PMSR/RRA: 1 1 $59,434 $61,695 $63,849 CRIP: Section 2 0445 Ascension Genesys Hospital $0.00 PMSR/RRA: 2 2 $53,974 $56,431 $58,205 CRIP: Section 2 0453 Ascension Macomb Oakland Hospital $0.00 PMSR/RRA: 3 3 $54,619 $55,192 $55,746 CRIP: Section 2 0450 Ascension Providence Hospital Southfield Ca $0.00 PMSR/RRA: 3 3 $53,532 $54,084 $54,636 CRIP: Section 2 0452 Ascension St. John Hospital $0.00 PMSR/RRA: 4 4 $53,532 $54,084 $53,581 CRIP: Section 2 0354 Ascension St. Vincent Hospital Indianapolis $0.00 PMSR/RRA: 4 4 $57,288 $57,769 $58,906 CRIP: Section 2 0361 Ascension Wisconsin Hospital $0.00 PMSR/RRA: 3 3 $62,740 $63,850 $64,970 CRIP: Section 2 0456 Aultman Alliance Community Hospital $0.00 PMSR/RRA: 3 3 $53,350 $54,120 $55,000 CRIP: -

Designated Acute Care Hospital Stroke Centers 180424
Acute Stroke -ready; Comprehensive stroke COUNTY FACILITY NAME CITY ZIP Center or Primary Stroke Center? MONTGOMERY Abington Memorial Hospital Comprehensive stroke Center Abington 19001 ALLEGHENY Allegheny General Hospital Comprehensive Stroke Center Pittsburgh 15212 CUMBERLAND Carlisle Regional Medical Center Primary Stroke Center Carlisle 17015 FRANKLIN Chambersburg Hospital Primary Stroke Center Chambersburg 17201 CHESTER Chester County Hospital – Chester County Primary Stroke Center West Chester 19380 CAMBRIA Conemaugh Memorial Medical Center Primary Stroke Center Johnstown 15905 BLAIR Conemaugh Nason Medical Center Acute Stroke -ready Roaring Spring 16673 BUCKS Doylestown Hospital Primary Stroke Center Doylestown 18901 MONTGOMERY Einstein Medical Center Montgomery Primary Stroke Center East Norriton 19403 LANCASTER Ephrata Community Hospital Primary Stroke Center Ephrata 17522 WESTMORELAND Excela Health Frick Hospital Primary Stroke Center Westmoreland 15666 WESTMORELAND Excela Health Latrobe Hospital Primary Stroke Center Latrobe 15650 WESTMORELAND Excela Health Westmoreland Hospital Primary Stroke Center Greensburg 15601 LACKAWANNA Geisinger Community Medical Center – Scranton - Lackawanna County Primary Stroke Center Scranton 18510 MONTOUR Geisinger Medical Center – Montour County Primary Stroke Center Danville 17822 LUZERNE Geisinger Wyoming Valley Medical Center, Wilkes-Barre – Luzerne County Primary Stroke Center Wilkes Barre 18711 ADAMS Gettysburg Hospital Primary Stroke Center Gettysburg 17325 CARBON Gnadden Huetten Memorial -

Student Scholarship Abel, Timothy S. Temple Scholar Award Temple University Grant University of Delaware Scholar University of Maryland President's Scholarship A.J
Student Scholarship Abel, Timothy S. Temple Scholar Award Temple University Grant University of Delaware Scholar University of Maryland President's Scholarship A.J. Drexel Scholarship Amoruso, Donald Joseph Drexel University Endowed Grant Duquesne University Grant Duquesne University Academic Scholarship Arnone, Mario Drexel University Endowed Grant Becker, Colin Duquesne University Academic Scholarship St. Joseph's University Regis Grant St. Joseph's University Achievement Scholarship St. Joseph's University Mission Scholarship St. Joseph's University Legacy Scholarship Temple Scholar Award Begley, William Francis American University Frederick Douglas Scholarship Northeastern University Dean's Scholarship Christian Bernlohr Drexel University Dean Scholar Bondiskey, Patrick Michael Drexel University Endowed Grant Temple Scholar Award Bowman, David Edward Alvernia University Achievement Award Alvernia University PACE Award Duquesne University Academic Scholarship Briggs, Shawn Michael Albright College Trustee Grant Lebanon Valley College Grant Lebanon Valley College Grant-In-Aid Lebanon Valley Leadership Award Misericordia Mission Award Misericordia University Dean's Award Misericordia University Presidential Scholarship Buonomo, Andrew Joseph Catholic University Scholarship Duquesne University Academic Scholarship LaSalle University Founders Scholarship St. Joseph's University Achievement Scholarship St. Joseph's University Legacy Scholarship St. Joseph's University Regis Grant Burke, Daniel Richard Duquesne University Academic Scholarship -

Course Catalog 2019 - 2020
COURSE CATALOG 2019 - 2020 mc3.edu TABLE OF CONTENTS COLLEGE FACULTY AND STAFF.................................................................................................2 1 COLLEGE FACULTY AND STAFF Cheryl L. Dilanzo, R.T. (R), Director of Radiography B.S. Thomas Jefferson University M.S. University of Pennsylvania Therol Dix, Dean of Arts and Humanities COLLEGE FACULTY B.A. University of California, Los AngelesM.A. University of Pennsylvania J.D. Georgetown University AND STAFF Bethany Eisenhart, Part-Time Career Coach ADMINISTRATION B.S. DeSales University Kimberly Erdman, Director of Dental Hygiene A.A.S., B.S. Pennsylvania College of Technology Office of the President M.S. University of Bridgeport Victoria L. Bastecki-Perez, President Katina Faulk, Administrative Director for Academic Initiatives D.H. University of Pittsburgh A.S., B.S. Pennsylvania College of Technology B.S. Edinboro University of Pennsylvania M.B.A. Excelsior College M.Ed, Ed.D. University of Pittsburgh Gaetan Giannini, Dean of Business and Entrepreneurial Initiatives Candy K. Basile, Administrative Support Secretary B.S. Temple University A.A.S. Montgomery County Community College M.B.A. Seton Hall University Deborah Rogers, Executive Assistant to the College’s Board of Trustees Ed.D. Gwynedd Mercy University A.A.S. Montgomery County Community College Suzanne Vargus Holloman, WIF Grant Project Director B.S. Syracuse University Academic Affairs M.B.A. Drexel University Gloria Oikelome, Interim Vice President of Academic Affairs and Dean of Sean Hutchinson, Coordinator of Integrated Learning Health Sciences B.A., M.A. La Salle University B.S. Bethel University Alfonzo Jordan, Science, Technology, Engineering and Mathematics Lab M.S. Long Island University Manager Ed.D.