Safety of Vaginal Estrogens: a Systematic Review Supplemental
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Androgen Excess in Breast Cancer Development: Implications for Prevention and Treatment
26 2 Endocrine-Related G Secreto et al. Androgen excess in breast 26:2 R81–R94 Cancer cancer development REVIEW Androgen excess in breast cancer development: implications for prevention and treatment Giorgio Secreto1, Alessandro Girombelli2 and Vittorio Krogh1 1Epidemiology and Prevention Unit, Fondazione IRCCS – Istituto Nazionale dei Tumori, Milano, Italy 2Anesthesia and Critical Care Medicine, ASST – Grande Ospedale Metropolitano Niguarda, Milano, Italy Correspondence should be addressed to G Secreto: [email protected] Abstract The aim of this review is to highlight the pivotal role of androgen excess in the Key Words development of breast cancer. Available evidence suggests that testosterone f breast cancer controls breast epithelial growth through a balanced interaction between its two f ER-positive active metabolites: cell proliferation is promoted by estradiol while it is inhibited by f ER-negative dihydrotestosterone. A chronic overproduction of testosterone (e.g. ovarian stromal f androgen/estrogen balance hyperplasia) results in an increased estrogen production and cell proliferation that f androgen excess are no longer counterbalanced by dihydrotestosterone. This shift in the androgen/ f testosterone estrogen balance partakes in the genesis of ER-positive tumors. The mammary gland f estradiol is a modified apocrine gland, a fact rarely considered in breast carcinogenesis. When f dihydrotestosterone stimulated by androgens, apocrine cells synthesize epidermal growth factor (EGF) that triggers the ErbB family receptors. These include the EGF receptor and the human epithelial growth factor 2, both well known for stimulating cellular proliferation. As a result, an excessive production of androgens is capable of directly stimulating growth in apocrine and apocrine-like tumors, a subset of ER-negative/AR-positive tumors. -
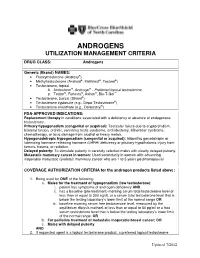
Androgens Utilization Management Criteria
ANDROGENS UTILIZATION MANAGEMENT CRITERIA DRUG CLASS: Androgens Generic (Brand) NAMES: • Fluoxymesterone (Androxy®) • Methyltestosterone (Android®, Methitest®, Testred®) • Testosterone, topical A. Androderm®, Androgel® - Preferred topical testosterone ® ® ® ™ B. Testim , Fortesta , Axiron , Bio-T-Gel • Testosterone, buccal (Striant®) • Testosterone cypionate (e.g., Depo-Testosterone®) • Testosterone enanthate (e.g., Delatestryl®) FDA-APPROVED INDICATIONS: Replacement therapy in conditions associated with a deficiency or absence of endogenous testosterone. Primary hypogonadism (congenital or acquired): Testicular failure due to cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchidectomy, Klinefelter syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. Hypogonadotropic hypogonadism (congenital or acquired): Idiopathic gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. Delayed puberty: To stimulate puberty in carefully selected males with clearly delayed puberty. Metastatic mammary cancer in women: Used secondarily in women with advancing inoperable metastatic (skeletal) mammary cancer who are 1 to 5 years postmenopausal COVERAGE AUTHORIZATION CRITERIA for the androgen products listed above: 1. Being used for ONE of the following: a. Males for the treatment of hypogonadism (low testosterone): i. patient has symptoms of androgen deficiency AND ii. has a baseline (pre-treatment) morning serum total testosterone level of less than or equal to 300 ng/dL or a serum total testosterone level that is below the testing laboratory’s lower limit of the normal range OR iii. baseline morning serum free testosterone level, measured by the equilibrium dialysis method, of less than or equal to 50 pg/ml or a free serum testosterone level that is below the testing laboratory’s lower limit of the normal range, OR b. -

Phase II Study of Hormone Therapy with Tamoxifen in Patients with Well Differentiated Neuroendocrine Tumors and Hormone Receptor Positive Expression (HORMONET)
Phase II study of hormone therapy with tamoxifen in patients with well differentiated neuroendocrine tumors and hormone receptor positive expression (HORMONET) Time of researchers and respective Departments: Rachel Riechelmann (Main Investigador)1, Milton Barros 1, Marcos Camandaroba1,2, Virgilio Souza1,2, Celso Abdon Mello1, Paula Nicole3, Eduardo Nóbrega4, Ludmilla Chinen5, Marina De Brot6, Héber Salvador7. Departaments: 1- Clinical Oncology; 2- postgraduate student; 3- Radiology; 4- Nuclear Medicine; 5-International Research Center (CIPE); 6-Pathologic anatomy; 7- Abdomen Surgery AC Camargo Cancer Center - Brazil Registration Number on Institutional Research Ethics Committee: 2626/18 March,06,2019 Introduction Neuroendocrine tumors (NET) are rare neoplasms, but with increasing incidence and prevalence in the last decades. Although they may manifest in the most diverse tissues, the vast majority of cases will affect organs of the digestive tract and lung. At diagnosis, more than half of the cases present metastatic disease, and among patients with localized disease, up to one-third will have recurrence of the disease. Unfortunately, the minority of patients with metastatic disease are eligible for curative intent.1 Although there are many types of NET, they are often studied together as a group because their cells share common histological findings, have special secretory granules, and the ability to secrete bioactive amines and polypeptide hormones. Approximately 25 percent of the tumors present functional hormonal syndromes (situation of great morbidity for these patients), being the carcinoid syndrome, the most common one. From the molecular point of view, these neoplasias are largely dependent on the activation of the mTOR pathway and neoangiogenesis.2 Another striking feature of neuroendocrine cells is the expression of cell surface hormone receptors whose activation or blockade may exert an important regulatory function. -

CASODEX (Bicalutamide)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Gynecomastia and breast pain have been reported during treatment with These highlights do not include all the information needed to use CASODEX 150 mg when used as a single agent. (5.3) CASODEX® safely and effectively. See full prescribing information for • CASODEX is used in combination with an LHRH agonist. LHRH CASODEX. agonists have been shown to cause a reduction in glucose tolerance in CASODEX® (bicalutamide) tablet, for oral use males. Consideration should be given to monitoring blood glucose in Initial U.S. Approval: 1995 patients receiving CASODEX in combination with LHRH agonists. (5.4) -------------------------- RECENT MAJOR CHANGES -------------------------- • Monitoring Prostate Specific Antigen (PSA) is recommended. Evaluate Warnings and Precautions (5.2) 10/2017 for clinical progression if PSA increases. (5.5) --------------------------- INDICATIONS AND USAGE -------------------------- ------------------------------ ADVERSE REACTIONS ----------------------------- • CASODEX 50 mg is an androgen receptor inhibitor indicated for use in Adverse reactions that occurred in more than 10% of patients receiving combination therapy with a luteinizing hormone-releasing hormone CASODEX plus an LHRH-A were: hot flashes, pain (including general, back, (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of pelvic and abdominal), asthenia, constipation, infection, nausea, peripheral the prostate. (1) edema, dyspnea, diarrhea, hematuria, nocturia, and anemia. (6.1) • CASODEX 150 mg daily is not approved for use alone or with other treatments. (1) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca Pharmaceuticals LP at 1-800-236-9933 or FDA at 1-800-FDA-1088 or ---------------------- DOSAGE AND ADMINISTRATION ---------------------- www.fda.gov/medwatch The recommended dose for CASODEX therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening). -

Study Protocol and Statistical Analysis Plan
Confidential Clinical study protocol number: J1228 Page 1 Version Date: May 7, 2018 IRB study Number: NA_00067315 A Trial of maintenance Rituximab with mTor inhibition after High-dose Consolidative Therapy in CD20+, B-cell Lymphomas, Gray Zone Lymphoma, and Hodgkin’s Lymphoma Principal Investigator: Douglas E. Gladstone, MD The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins 1650 Orleans Street, CRBI-287 Baltimore, MD 21287 Phone: 410-955-8781 Fax: 410-614-1005 Email: [email protected] IRB Protocol Number: NA_00067315 Study Number: J1228 IND Number: EXEMPT Novartis Protocol Number: CRAD001NUS157T Version: May 7, 2018 Co-Investigators: Jonathan Powell 1650 Orleans Street, CRBI-443 Phone: 410-502-7887 Fax: 443-287-4653 Email: [email protected] Richard Jones 1650 Orleans Street, CRBI-244 Phone: 410-955-2006 Fax: 410-614-7279 Email: [email protected] Confidential Clinical study protocol number: J1228 Page 2 Version Date: May 7, 2018 IRB study Number: NA_00067315 Satish Shanbhag Johns Hopkins Bayview Medical Center 301 Building, Suite 4500 4940 Eastern Ave Phone: 410-550-4061 Fax: 410-550-5445 Email: [email protected] Statisticians: Gary Rosner Phone: 410-955-4884 Email: [email protected] Marianna Zahurak Phone: 410-955-4219 Email: [email protected] Confidential Clinical study protocol number: J1228 Page 3 Version Date: May 7, 2018 IRB study Number: NA_00067315 Table of contents Table of contents ......................................................................................................................... 3 List of abbreviations -

Effect of Dehydroepiandrosterone and Testosterone Supplementation on Systemic Lipolysis
ORIGINAL ARTICLE Effect of Dehydroepiandrosterone and Testosterone Supplementation on Systemic Lipolysis Ana E. Espinosa De Ycaza, Robert A. Rizza, K. Sreekumaran Nair, and Michael D. Jensen Division of Endocrinology, Endocrine Research Unit, Mayo Clinic, Rochester, Minnesota 55905 Downloaded from https://academic.oup.com/jcem/article/101/4/1719/2804555 by guest on 24 September 2021 Context: Dehydroepiandrosterone (DHEA) and T hormones are advertised as antiaging, antiobe- sity products. However, the evidence that these hormones have beneficial effects on adipose tissue metabolism is limited. Objective: The objective of the study was to determine the effect of DHEA and T supplementation on systemic lipolysis during a mixed-meal tolerance test (MMTT) and an iv glucose tolerance test (IVGTT). Design: This was a 2-year randomized, double-blind, placebo-controlled trial. Setting: The study was conducted at a general clinical research center. Participants: Sixty elderly women with low DHEA concentrations and 92 elderly men with low DHEA and bioavailable T concentrations participated in the study. Interventions: Elderly women received 50 mg DHEA (n ϭ 30) or placebo (n ϭ 30). Elderly men received 75 mg DHEA (n ϭ 30),5mgT(nϭ 30), or placebo (n ϭ 32). Main Outcome Measures: In vivo measures of systemic lipolysis (palmitate rate of appearance) during a MMTT or IVGTT. Results: At baseline there was no difference in insulin suppression of lipolysis measured during MMTT and IVGTT between the treatment groups and placebo. For both sexes, a univariate analysis showed no difference in changes in systemic lipolysis during the MMTT or IVGTT in the DHEA group and T group when compared with placebo. -

Estradiol Acetate Vaginal Ring) Rx Only
NDA 21-367/S-002 Page 3 PRESCRIBING INFORMATION Femring® (estradiol acetate vaginal ring) Rx Only ESTROGENS INCREASE THE RISK OF ENDOMETRIAL CANCER Close clinical surveillance of all women taking estrogens is important. Adequate diagnostic measures, including endometrial sampling when indicated, should be undertaken to rule out malignancy in all cases of undiagnosed persistent or recurring abnormal vaginal bleeding. There is no evidence that the use of “natural” estrogens results in a different endometrial risk profile than synthetic estrogens at equivalent estrogen doses. (See WARNINGS, Malignant neoplasms, Endometrial cancer.) CARDIOVASCULAR AND OTHER RISKS Estrogens with or without progestins should not be used for the prevention of cardiovascular disease or dementia. (See WARNINGS, Cardiovascular disorders and Dementia.) The Women’s Health Initiative (WHI) study reported increased risks of myocardial infarction, stroke, invasive breast cancer, pulmonary emboli, and deep vein thrombosis in postmenopausal women (50 to 79 years of age) during 5 years of treatment with oral conjugated estrogens (CE 0.625 mg) combined with medroxyprogesterone acetate (MPA 2.5 mg) relative to placebo. (See CLINICAL PHARMACOLOGY, Clinical Studies and WARNINGS, Cardiovascular disorders and Malignant neoplasms, Breast cancer.) The Women’s Health Initiative Memory Study (WHIMS), a substudy of WHI, reported increased risk of developing probable dementia in postmenopausal women 65 years of age or older during 4 years of treatment with oral conjugated estrogens -

Reproductive DHEA-S
Reproductive DHEA-S Analyte Information - 1 - DHEA-S Introduction DHEA-S, DHEA sulfate or dehydroepiandrosterone sulfate, it is a metabolite of dehydroepiandrosterone (DHEA) resulting from the addition of a sulfate group. It is the sulfate form of aromatic C19 steroid with 10,13-dimethyl, 3-hydroxy group and 17-ketone. Its chemical name is 3β-hydroxy-5-androsten-17-one sulfate, its summary formula is C19H28O5S and its molecular weight (Mr) is 368.5 Da. The structural formula of DHEA-S is shown in (Fig.1). Fig.1: Structural formula of DHEA-S Other names used for DHEA-S include: Dehydroisoandrosterone sulfate, (3beta)-3- (sulfooxy), androst-5-en-17-one, 3beta-hydroxy-androst-5-en-17-one hydrogen sulfate, Prasterone sulfate and so on. As DHEA-S is very closely connected with DHEA, both hormones are mentioned together in the following text. Biosynthesis DHEA-S is the major C19 steroid and is a precursor in testosterone and estrogen biosynthesis. DHEA-S originates almost exclusively in the zona reticularis of the adrenal cortex (Fig.2). Some may be produced by the testes, none is produced by the ovaries. The adrenal gland is the sole source of this steroid in women, whereas in men the testes secrete 5% of DHEA-S and 10 – 20% of DHEA. The production of DHEA-S and DHEA is regulated by adrenocorticotropin (ACTH). Corticotropin-releasing hormone (CRH) and, to a lesser extent, arginine vasopressin (AVP) stimulate the release of adrenocorticotropin (ACTH) from the anterior pituitary gland (Fig.3). In turn, ACTH stimulates the adrenal cortex to secrete DHEA and DHEA-S, in addition to cortisol. -

Targeting Glycine Reuptake in Alcohol Seeking and Relapse
JPET Fast Forward. Published on January 24, 2018 as DOI: 10.1124/jpet.117.244822 This article has not been copyedited and formatted. The final version may differ from this version. TITLE PAGE Targeting Glycine Reuptake in Alcohol Seeking and Relapse Valentina Vengeliene, Martin Roßmanith, Tatiane T. Takahashi, Daniela Alberati, Berthold Behl, Anton Bespalov, Rainer Spanagel Downloaded from The primary laboratory of origin: Institute of Psychopharmacology, Central Institute of jpet.aspetjournals.org Mental Health, Faculty of Medicine Mannheim, Heidelberg University, Germany; at ASPET Journals on September 30, 2021 VV, MR, TTT, RS: Institute of Psychopharmacology, Central Institute of Mental Health, Faculty of Medicine Mannheim, Heidelberg University, Germany; DA: Roche Pharma Research and Early Development, Neuroscience, Ophthalmology and Rare Diseases, Roche Innovation Center Basel, CH-4070 Basel, Switzerland; BB, AB: Department of Neuroscience Research, AbbVie Deutschland GmbH & Co. KG, Ludwigshafen, Germany; AB: Department of Psychopharmacology, Pavlov Medical University, St Petersburg, Russia JPET #244822 JPET Fast Forward. Published on January 24, 2018 as DOI: 10.1124/jpet.117.244822 This article has not been copyedited and formatted. The final version may differ from this version. RUNNING TITLE GlyT1 in Alcohol Seeking and Relapse Corresponding author with complete address: Valentina Vengeliene, Institute of Psychopharmacology, Central Institute of Mental Health (CIMH), J5, 68159 Mannheim, Germany Email: [email protected], phone: +49-621-17036261; fax: +49-621- Downloaded from 17036255 jpet.aspetjournals.org The number of text pages: 33 Number of tables: 0 Number of figures: 6 Number of references: 44 at ASPET Journals on September 30, 2021 Number of words in the Abstract: 153 Number of words in the Introduction: 729 Number of words in the Discussion: 999 A recommended section assignment to guide the listing in the table of content: Drug Discovery and Translational Medicine 2 JPET #244822 JPET Fast Forward. -

Estradiol (E2), Estriol (E3), Ethinylestradiol (EE2), Testosterone (TEST), Androstenedione (AND), and Progesterone
UNIVERSITY OF CINCINNATI Date: 13-Aug-2010 I, Ruth Marfil Vega , hereby submit this original work as part of the requirements for the degree of: Doctor of Philosophy in Environmental Science It is entitled: Abiotic Transformation of Estrogens in Wastewater Student Signature: Ruth Marfil Vega This work and its defense approved by: Committee Chair: Makram Suidan, PhD Makram Suidan, PhD George Sorial, PhD George Sorial, PhD Margaret Kupferle, PhD, PE Margaret Kupferle, PhD, PE Marc Mills, PhD Marc Mills, PhD 11/8/2010 1,041 Abiotic Transformation of Estrogens in Wastewater A Dissertation submitted to the Graduate School of the University of Cincinnati in partial fulfillment of the requirements for the degree of Doctor of Philosophy In the School of Energy, Environmental, Biological and Medical Engineering By Ruth Marfil-Vega B.S. Chemistry, University of Valladolid, Spain, 2001 Committee Chair: Makram T. Suidan, Ph.D. ABSTRACT The fate of seven steroids: estrone (E1), estradiol (E2), estriol (E3), ethinylestradiol (EE2), testosterone (TEST), androstenedione (AND), and progesterone (PROG), in the presence of synthetic wastewater was studied in order to establish the role abiotic processes play in the elimination of these chemicals from the environment. Comprehension of these mechanisms will foster the optimization of the existing wastewater treatment technologies and the development of sustainable alternatives. Distinctive behavior was encountered for the target compounds in accordance with their chemical structure, hence, different physico-chemical properties and reactivity. Estrogenic compounds, comprising E1, E2, E3 and EE2, were found to undergo a catalytic transformation when contacted with a model vegetable material present in the synthetic wastewater. -

The Mechanisms and Managements of Hormone-Therapy Resistance in Breast and Prostate Cancers
Endocrine-Related Cancer (2005) 12 511–532 REVIEW The mechanisms and managements of hormone-therapy resistance in breast and prostate cancers K-M Rau1,2*, H-Y Kang3,4*, T-L Cha1,5,6, S A Miller1 and M-C Hung1 1Department of Molecular and Cellular Oncology, The University of Texas M.D. Anderson Cancer Center, Houston, TX 77030, USA 2Department of Hematology-Oncology, Chang Gung Memorial Hospital, Kaohsiung Medical Center, Kaohsiung, Taiwan 3Graduate Institute of Clinical Medical Sciences, Chang Gung University, Kaohsiung, Taiwan 4The Center for Menopause and Reproductive Medicine Research, Chang Gung Memorial Hospital, Kaohsiung Medical Center, Kaohsiung, Taiwan 5Graduate School of Biomedical Sciences, The University of Texas Health Science Center at Houston, Houston, TX 77030, USA 6Division of Urology, Department of Surgery, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan (Requests for offprints should be addressed to M-C Hung; Email: [email protected]) *(K-M Rau and H-Y Kang contributed equally to this work) Abstract Breast and prostate cancer are the most well-characterized cancers of the type that have their development and growth controlled by the endocrine system. These cancers are the leading causes of cancer death in women and men, respectively, in the United States. Being hormone-dependent tumors, antihormone therapies usually are effective in prevention and treatment. However, the emergence of resistance is common, especially for locally advanced tumors and metastatic tumors, in which case resistance is predictable. The phenotypes of these resistant tumors include receptor- positive, ligand-dependent; receptor-positive, ligand-independent; and receptor-negative, ligand- independent. The underlying mechanisms of these phenotypes are complicated, involving not only sex hormones and sex hormone receptors, but also several growth factors and growth factor re- ceptors, with different signaling pathways existing alone or together, and with each pathway possibly linking to one another. -

A Simple Method to Measure Sulfonation in Man Using Paracetamol As Probe Drug Natália Marto 1,2*, Judit Morello1,3, Alexandra M
www.nature.com/scientificreports OPEN A simple method to measure sulfonation in man using paracetamol as probe drug Natália Marto 1,2*, Judit Morello1,3, Alexandra M. M. Antunes3, Sofa Azeredo4, Emília C. Monteiro1,5 & Sofa A. Pereira1,5 Sulfotransferase enzymes (SULT) catalyse sulfoconjugation of drugs, as well as endogenous mediators, gut microbiota metabolites and environmental xenobiotics. To address the limited evidence on sulfonation activity from clinical research, we developed a clinical metabolic phenotyping method using paracetamol as a probe substrate. Our aim was to estimate sulfonation capability of phenolic compounds and study its intraindividual variability in man. A total of 36 healthy adult volunteers (12 men, 12 women and 12 women on oral contraceptives) received paracetamol in a 1 g-tablet formulation on three separate occasions. Paracetamol and its metabolites were measured in plasma and spot urine samples using liquid chromatography-high resolution mass spectrometry. A metabolic ratio (Paracetamol Sulfonation Index—PSI) was used to estimate phenol SULT activity. PSI showed low intraindividual variability, with a good correlation between values in plasma and spot urine samples. Urinary PSI was independent of factors not related to SULT activity, such as urine pH or eGFR. Gender and oral contraceptive intake had no impact on PSI. Our SULT phenotyping method is a simple non-invasive procedure requiring urine spot samples, using the safe and convenient drug paracetamol as a probe substrate, and with low intraindividual coefcient of variation. Although it will not give us mechanistic information, it will provide us an empirical measure of an individual’s sulfonator status. To the best of our knowledge, our method provides the frst standardised in vivo empirical measure of an individual’s phenol sulfonation capability and of its intraindividual variability.