Alcohol and Diabetes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mixing Alcohol with Your Diabetes You Can Drink If Your Blood Sugar Is Well Controlled – and You Take the Right Steps to Be Safe
Diabetes Education – #16 Mixing Alcohol with Your Diabetes You can drink if your blood sugar is well controlled – and you take the right steps to be safe. If you have diabetes, you may think that drinking is off limits. Not so! Keeping an eye on how much and what you drink can help you drink more safely. You can avoid the alcohol-related pitfalls: • low blood sugar • weight gain • high blood pressure. Before you have a drink, ask yourself the 3 questions below. The ADA (American Diabetes Association) suggests these: • Is my diabetes in good control? • Does my health care team agree that I can have alcohol? • Do I know how alcohol can affect me and my blood sugar? If you can answer "yes" to all 3 questions, it is likely OK to have a drink. But make sure you know the potential effects of drinking. And, make sure you know your personal limits. What happens when you drink? Between meals and while you sleep, the liver makes new glucose (sugar). The liver then sends this sugar into the bloodstream. Here, it helps to prevent or slow down a low blood sugar reaction. When you drink, it disrupts the process. Substances form when alcohol breaks down in the liver. These substances block the liver from making new glucose. Blood sugars fall and you can quickly become too low. Diabetes Education – #16 Treat hypoglycemia quickly Drinking can affect your blood sugar for up to 12 hours. So test your blood sugar before going to bed. If it is in the 100 – 140 mg/dL range, you may be fine. -

Managing a High Output Ostomy: for Patients with an Ileostomy Or Jejunostomy
Form: D-8844 Managing a High Output Ostomy: For patients with an ileostomy or jejunostomy Read this brochure to learn: • what is a high output ostomy • why is a high output ostomy a problem • what foods and drinks can help you manage it What is a high output ostomy? A high output ostomy is when your ostomy output (the amount of waste coming out of your stoma) is more than 1.2 litres (about 5 cups) in a day. Signs of a high output ostomy include: • having to empty your stoma bag more than 8 times a day • having watery output Why is it a problem? You may become dehydrated (your body does not get enough water) if you have too much output. Your body may not absorb fluids well when you have a high output ostomy. Signs of dehydration are: • feeling thirsty • peeing less than usual • having dark yellow pee • losing weight • having dry lips and mouth • having a headache, dizziness or fatigue 2 How can I manage a high output ostomy? Making some changes to how you eat and drink can help manage a high output ostomy. Your health care team may also give you medicine to help manage a high output ostomy. 9 Have a small meal every 2 to 3 hours. This helps your body absorb food better and meet your nutrition needs. 9 Chew your food very well. This makes it easier for your body to break down and use the food you eat. 9 Do not drink fluids while you eat. Wait 30 minutes before and after a meal before drinking fluids. -

Medicines That Affect Fluid Balance in the Body
the bulk of stools by getting them to retain liquid, which encourages the Medicines that affect fluid bowels to push them out. balance in the body Osmotic laxatives e.g. Lactulose, Macrogol - these soften stools by increasing the amount of water released into the bowels, making them easier to pass. Older people are at higher risk of dehydration due to body changes in the ageing process. The risk of dehydration can be increased further when Stimulant laxatives e.g. Senna, Bisacodyl - these stimulate the bowels elderly patients are prescribed medicines for chronic conditions due to old speeding up bowel movements and so less water is absorbed from the age. stool as it passes through the bowels. Some medicines can affect fluid balance in the body and this may result in more water being lost through the kidneys as urine. Stool softener laxatives e.g. Docusate - These can cause more water to The medicines that can increase risk of dehydration are be reabsorbed from the bowel, making the stools softer. listed below. ANTACIDS Antacids are also known to cause dehydration because of the moisture DIURETICS they require when being absorbed by your body. Drinking plenty of water Diuretics are sometimes called 'water tablets' because they can cause you can reduce the dry mouth, stomach cramps and dry skin that is sometimes to pass more urine than usual. They work on the kidneys by increasing the associated with antacids. amount of salt and water that comes out through the urine. Diuretics are often prescribed for heart failure patients and sometimes for patients with The major side effect of antacids containing magnesium is diarrhoea and high blood pressure. -

Water Requirements, Impinging Factors, and Recommended Intakes
Rolling Revision of the WHO Guidelines for Drinking-Water Quality Draft for review and comments (Not for citation) Water Requirements, Impinging Factors, and Recommended Intakes By A. Grandjean World Health Organization August 2004 2 Introduction Water is an essential nutrient for all known forms of life and the mechanisms by which fluid and electrolyte homeostasis is maintained in humans are well understood. Until recently, our exploration of water requirements has been guided by the need to avoid adverse events such as dehydration. Our increasing appreciation for the impinging factors that must be considered when attempting to establish recommendations of water intake presents us with new and challenging questions. This paper, for the most part, will concentrate on water requirements, adverse consequences of inadequate intakes, and factors that affect fluid requirements. Other pertinent issues will also be mentioned. For example, what are the common sources of dietary water and how do they vary by culture, geography, personal preference, and availability, and is there an optimal fluid intake beyond that needed for water balance? Adverse consequences of inadequate water intake, requirements for water, and factors that affect requirements Adverse Consequences Dehydration is the adverse consequence of inadequate water intake. The symptoms of acute dehydration vary with the degree of water deficit (1). For example, fluid loss at 1% of body weight impairs thermoregulation and, thirst occurs at this level of dehydration. Thirst increases at 2%, with dry mouth appearing at approximately 3%. Vague discomfort and loss of appetite appear at 2%. The threshold for impaired exercise thermoregulation is 1% dehydration, and at 4% decrements of 20-30% is seen in work capacity. -

How Do You Look After a Vomiting Drunk Friend?
Alcohol and Young People How do you look after a vomiting drunk friend? Vomiting can be life-threatening even when The police do not routinely attend an ambulance alcohol is not involved. If a vomiting person call, even if there are illegal drugs involved. The has been drinking alcohol, it can cause them to only reason the police will usually attend is if the lose a natural response called the ‘gag reflex’. paramedics ask them to be there. This is usually With no gag reflex, a person is in danger of due to another crime taking place or the threat of choking on their own vomit, particularly if they violence. lose consciousness. Helping a drunk friend can be difficult and potentially Whether you are drinking alcohol or not, there dangerous. Often, the person may be aggressive are some simple things you can do to look after a and uncooperative. While it is important to try to vomiting, drunk friend: keep your friend safe, the first priority must always stay with them and monitor them closely be your personal safety. Never be afraid to pass the problem over to someone else, particularly if they keep them as upright as possible and never become violent. If in doubt, call 000. lay them down give them a plastic bucket or bowl and make ALWAYS REMEMBER, YOU ARE A FRIEND, sure they are somewhere safe where they NOT A DOCTOR can be watched get them to rinse their mouth out regularly keep them warm reassure them if in doubt, call 000 immediately What causes vomiting? sheet ‘Alcohol Poisoning’). -
Guidelines for Drinking-Water Quality FIRST ADDENDUM to THIRD EDITION Volume 1 Recommendations WHO Library Cataloguing-In-Publication Data World Health Organization
Guidelines for Drinking-water Quality FIRST ADDENDUM TO THIRD EDITION Volume 1 Recommendations WHO Library Cataloguing-in-Publication Data World Health Organization. Guidelines for drinking-water quality [electronic resource] : incorporating first addendum. Vol. 1, Recommendations. – 3rd ed. Electronic version for the Web. 1.Potable water – standards. 2.Water – standards. 3.Water quality – standards. 4.Guidelines. I. Title. ISBN 92 4 154696 4 (NLM classification: WA 675) © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel: +41 22 791 3264; fax: +41 22 791 4857; email: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; email: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expres- sion of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -

Fluids in Sport Why Fluid Is Important Dehydration and Performance Can
Fluids in Sport Why fluid is important Water is essential to maintain blood volume, regulate Can you drink too much? body temperature and allow muscle contractions to take place. During exercise, the main way the body Drinking more fluid than is comfortable, in any conditions, has the potential to interfere with your maintains optimal body temperature is by sweating. performance. In cool weather or when the exercise Heat is removed from the body when beads of sweat on pace is gentle, the rate of sweat loss may be quite low. the skin evaporate, resulting in a loss of body fluid. It is unnecessary and potentially dangerous to drink at Sweat production, and therefore fluid loss, increases with a rise in ambient temperature and humidity, as well rates that are far greater than sweat losses. Such as with an increase in exercise intensity. over-hydration during exercise can cause a dilution of blood sodium levels (hyponatraemia). Symptoms include headaches, disorientation, coma, and in Drinking fluid during exercise is necessary to replace severe cases, death. It is important to note though fluids lost in sweat. This action will reduce the risk of heat stress, maintain normal muscle function, and that this is relatively rare and dehydration is a much prevent performance decreases due to dehydration. more common issue. In most cases during exercise, the rates of sweat loss are higher than the rate you can drink, so most athletes get into fluid deficit. Therefore, fluid guidelines promote Estimating your fluid losses drinking more fluid to reduce the deficit and potential Knowing your sweat rate can give you an indication of performance detriments associated with dehydration. -
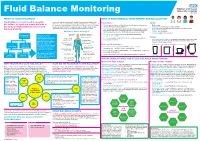
Fluid Balance Monitoring
Fluid Balance Monitoring WHAT IS FLUID BALANCE? WHO IS RESPONSIBLE: MONITORING AND ESCALATION Fluid balance is a term used to describe In order to maintain homeostasis, the adult human body needs a fluid Trained Nurses Doctors intake of 2-3 litres (25-30ml / kg per day), allowing it to keep a balance of the balance of input and output of fluids in the nutrients, oxygen and water, which are necessary to preserve a stable • Identify patients who need fluid balance monitoring and communicate • Daily review: the body, to allow metabolic processes to healthy internal environment. Output should be roughly equal, though via whiteboard behind bed, handover Indication for monitoring, is it still necessary? – document with special instructions such as restrictions or function properly. ‘insensible losses’ may give a slightly positive balance on charts. • Clarify up-to-date plan with medical team and communicate to patient Goal and visitors, wider MDT including HCAs: SALT, housekeeping, physio frequency of monitoring What does water do for you? and any colleague who may assist with, provide or remove fluids Charts – current balance Escalation plan or the need for it Forms saliva Needed by the brain to • Ensure accuracy using charts and calculating cumulative Human body is Although these fluid (digestion) manufacture hormones measurements 6 hourly 55-60% fluid compartments are classed as and neurotransmitters Patients separate, water and fluids are Keeps mucosal • Escalate promptly to medical team in case of developing imbalance, constantly moving between deterioration or concern • Must demonstrate capacity (understand information, retain and recall membranes moist Regulates body when asked) concerning their fluid balance monitoring if they are to them all, powered by different temperature (sweating processes such as diffusion complete charts independently. -

Oral Rehydraton Salt
ORAL REHYDRATON SALT Dehydration Dehydration occurs when water intake is not enough to replace free water lost due to normal physiologic processes, including breathing, urination, and perspiration, or other causes, including diarrhea and vomiting. Dehydration can be life-threatening when severe and lead to seizures or respiratory arrest, and also carries the risk of osmotic cerebral edema if rehydration is overly rapid. Treatment Correction of a dehydrated state is accomplished by the replenishment of necessary water and electrolytes (through oral rehydration therapy or fluid replacement by intravenous therapy. As oral rehydration is less painful, less invasive, less expensive, and easier to provide, it is the treatment of choice for mild dehydration. Solutions used for intravenous rehydration must be isotonic or hypertonic. Pure water injected into the veins will cause the breakdown (lysis) of red blood cells (erythrocytes). ORS section in National Institute of Health, Islamabad manufacture Oral Rehydration Salt new formula of WHO (World Health Organization). Composition Sodium Chloride 2.60g Potassium Chloride 1.50g Tri-sodium Citrate Di-hydrate 2.90g Glucose Anhydrous 13.50g Directions Dissolve one sachet of ORS in one-liter clean water. Do not boil the solution or mix anything. Use the solution within 24 hours. Dosage and Administration Infants: One liter over 24 hours’ period Children: One liter over 8 to 24 hours’ period. Adults: Drink freely as required (Two to four liters during 24 hours). Contraindications ORT should be discontinued and fluids replaced intravenously when vomiting is protracted despite proper administration of ORT, signs of dehydration worsen despite giving ORT, the person is unable to drink due to a decreased level of consciousness, or there is evidence of intestinal blockage or ileus. -

Oral Rehydration Therapy: the Behavioral Issues
ORAL REHYDRATION THERAPY: THE BEHAVIORAL ISSUES BEHAVIORAL ISSUES IN CHILD SURVIVAL PROGRAMS: Monograph NUlnber One Prepared for THE OFFICE OF HEALTH U.S. AGENCY FOR INTERNATIONAL DEVELOPMENT By Soheir Sukkary-Stolba, Ph.D. p~ -1\P.JG-l~'7 BEHAVIORAL ISSUES IN CHILD SURVIVAL PROGRAMS: A Synthesis of the Literature with Recommendations for Project Design & Implementation Monograph Number One ORAL REHYDRATION THERAPY: THE BEHAVIORAL ISSUES By Soheir Sukkary-Stolba, Ph.D. Prepared for THE OFFICE OF HEALTH U. S. AGENCY FOR INTERNATIONAL DEVELOPMENT Washington D.C. INTERNATIONAL HEALTH & DEVELOPMENT ASSOCIATES July 1990 Oral Rehydration Therapy: The Behavioral Issues Monograph Number One Sukkary-Stolba, Soheir (author) u.s. ~gency For International Development, Bureau for Science and Technology. Office of Health. (sponsor) International Health and Development Associates. 18133 Coastline Drive, suite 4A, Malibu, CA 90265 (sponsor) Behavioral Issues in Child survival Programs; A synthesis of the Literature with Recommendations for project Design & Implementation (six monograph series) *also available from: International Health and Development Associates. 18133 Coastline Drive, suite 4A, Malibu, CA 90265 Diarrhea remains the numbe.r one threat to the health and well-being of children in developing countries. Each year the dehydration that often results from diarrhea exacts a tremendous toll: the lives of more than five million infants and children. The simple and effective technology known as ORT (for oral rehydration therapy) provides a means to cut dramatically the number of diarrhea-related deaths. Although it is easy to use, teaching mothers and other child caretakers to prepare and administer ORT correctly has not been easy, however, many cultural, environ~ental and socio-economic factors influence local perceptions of diarrhea and the use of ORT. -

Diabetes Insipidus
www.healthinfo.org.nz Diabetes insipidus If you have cranial diabetes insipidus, it means you don't have enough anti-diuretic hormone (ADH). This hormone is also called arginine vasopressin (AVP). You make ADH in an area of your brain called the hypothalamus, which is just above your pituitary gland. Your pituitary gland releases the ADH into your blood. ADH acts on your kidneys, allowing you to make concentrated urine. If your body doesn't make enough ADH then your kidneys make a lot of dilute urine. As a result, you'll feel thirsty and have to urinate (wee) a lot. These symptoms are similar to those that people have with sugar diabetes (diabetes mellitus). However, people with diabetes insipidus have normal blood sugar levels. Their symptoms are caused by lack of ADH. What causes diabetes insipidus? Almost any disease that affects the pituitary region of the brain can cause diabetes insipidus. Causes include pituitary tumours, and damage caused by surgery or trauma. Sometimes there might be a genetic cause. Sometimes people's kidneys can't respond to ADH. This is called nephrogenic diabetes insipidus (NDI). NDI can be caused by some medications, in particular lithium. If you're taking lithium, it's important that you tell your doctor about any symptoms such as feeling very thirsty and passing lots of urine. You should also have regular blood tests to check your lithium level. Symptoms and diagnosis Feeling very thirsty, drinking lots of fluid (often preferring cold water) and passing lots of urine are the symptoms of diabetes insipidus. We diagnose diabetes insipidus with blood and urine tests. -
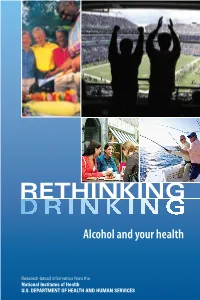
Rethinking Drinking in Focus Testing
Alcohol and your health Research-based information from the National Institutes of Health U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES “Sometimes we do things out of habit and we don’t really stop to think about it. This made me think about my choices.” “It emphasized that drinking is not bad in and of itself—it’s how much you’re doing it and how it’s affecting your life.” “I thought the strategies for cutting down were really good. It gives you tools to help yourself.” These are comments from social drinkers who reviewed Rethinking Drinking in focus testing. We welcome your comments as well. Send an email to [email protected] or call 301–443–3860. For an online version of this booklet with interactive features and additional resources, visit RethinkingDrinking.niaaa.nih.gov RETHINKING DRINKING Do you enjoy a drink now and then? Many of us do, often when socializing with friends and family. Drinking can be beneficial or harmful, depending on your age and health status, the situation, and, of course, how much you drink. much is t How Do you think you may drink too much at times? Do you think “everyone” drinks a lot? See below for results from a nationwide survey of 43,000 adults by the National Institutes of Health on alcohol use and its consequences. oo much? Alcohol use by adults in the United States* 37% 7 in 10 adults 3 in 10 adults always drink always drink at drink at levels at low-risk 28% low-risk levels levels that put them drink at or at risk for heavy or alcoholism, at-risk do not drink 35% liver disease, and at all don’t drink levels other problems about a change? Thinking at all *Although the minimum legal drinking age in the U.S.