Health Care Behind Bars, P. 20
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Administrative Segregation & Death Row Plan-1
Texas Department of Criminal Justice ------------------- Brad Livingston Executive Director () ?1)13 August 14,2013 VIA REGULAR MAIL Todd Hettenbach I WilmerHale 1875 Pennsylvania Avenue NW Washington, DC 20006 RE: Texas Civil Rights Project Dear Mr. Hettenback: In response to your open records request dated August 2, 2013 we have the "Death Row Plan (October 2004)" and "Administrative Segregation Plan (March 2012)", responsive to your request. If have any questions, please do not hesitate to contact this office. rY· .. !f};;JJ= tattenburg, A ministrator · Plans and Operations Texas Department of Criminal Justice Con-ectional Institutions Division /klj P.O. Box99 Huntsville, Texas 77342-0099 www.tdcj.state.tx.us TEXAS DEPARTMENT OF CRIMINAL JUSTICE Administrative Segregation Plan FOREWORD There are occasions within a conectional setting when it becomes necessary to administratively segregate offenders in order to preserve the safety and security of both offenders and staff. The Texas Department of Criminal Justice (TDCJ) policy, Administrative Directive (AD)-03.50, "Administrative Segregation" directs the TDCJ to develop an Administrative Segregation Plan which establishes uniform mles and regulations to guide staff in both the conditions and procedures relating to offenders housed in administrative segregation. The TDCJ is fully committed to abide by and enforce the provisions outlined herein, and all employees are expected to comply with its requirements. ACA References: 4-4140,4-4235,4-4250,4-4251-1,4-4253,4-254,4-4257,4-4258,4-4260,4-4261,4- 4262, 4-4263, 4-4265, 4-4266, 4-4268, 4-4269, 4-4270, and 4-4273 Supersedes: Administrative Segregation Plan, August 2005 3-o6 ·!20/1. -

On the Move, March 2019
March 2019 On The Move TDCJ Employee Promotions and Transfers Name From To Assistant Warden, Assistant Warden, Henry Adams Beauford H. Jester IV Psychiatric Unit Larry Gist State Jail Major of Correctional Officers, Major of Correctional Officers, Ricky Allen Mark W. Michael Unit Joe F. Gurney Transfer Facility Assistant Warden, Senior Warden, Damon Andrews William P. Clements Unit Joe Kegans State Jail Major of Correctional Officers, Major of Correctional Officers, Terry Andrews Glen Ray Goodman Transfer Facility Eastham Unit Senior Warden, Senior Warden, Richard Babcock Joe Kegans State Jail Beauford H. Jester IV Psychiatric Unit Major of Correctional Officers, Assistant Warden, James Blake Charles T. Terrell Unit Jim Ferguson Unit Senior Warden, Senior Warden, Rodger Bowers Manuel A. Segovia Unit/ Pam Lychner State Jail Reynaldo V. Lopez State Jail Senior Warden, Senior Warden, Stephen Bryant Pam Lychner State Jail Darrington Unit Senior Warden, Senior Warden, Michael Butcher Darrington Unit Allan B. Polunsky Unit Major of Correctional Officers, Assistant Warden, Joe Castillo John B. Connally Unit Price Daniel Unit Senior Warden, Senior Warden, Evelyn Castro Dolph Briscoe Unit/ Clarence N. Stevenson Unit Cotulla Transfer Facility Major of Correctional Officers, Assistant Warden, Nick Clayton Thomas Havins Unit Alfred D. Hughes Unit Senior Warden, Senior Warden, Mary Ann Comstock-King Charles T. Terrell Unit Mountain View/Hilltop Units Senior Warden, Senior Warden, Dennis Crowley Offender Transportation Reverend C.A. Holliday Transfer Facility Major of Correctional Officers, Assistant Warden, Kendrick Demyers A.M. “Mac” Stringfellow Unit Carol S. Vance Unit Senior Warden, Senior Warden, Daniel Dickerson Reverend C.A. Holliday Transfer Facility W.J. -

Texas Department of Corrections: 30 Years of Progress
If you have issues viewing or accessing this file contact us at NCJRS.gov. ____~____ ~:-:'----;-- - ~-- ----;--;:-'l~. - Texas Department of Corrections: 30 Years of Progress ,. In 1967, the Department published a report, Texas Department of Corrections: 20 Years of Progress. That report was largely the work of Mr. Richard C. Jones, former Assistant Director for Treatment. The report that follows borrowed hea-vily and in many cases directly from Mr. Jones' efforts. This is but another example of how we continue to profit from, and, hopefully, build upon the excellent wC';-h of those preceding us. Texas Department of Corrections: 30 Years of Progress NCJRS dAN 061978 ACQUISIT10i~:.j OFFICE OF THE GOVERNOR DOLPH BRISCOE STATE CAPITOL GOVERNOR AUSTIN, TEXAS 78711 My Fellow Texans: All Texans owe a debt of gratitude to the Honorable H. H. Coffield. former Chairman of the Texas Board of Corrections, who recently retired after many years of dedicated service on the Board; to the present members of the Board; to Mr. W. J. Estelle, Jr., Director of the Texas Department of Corrections; and to the many people who work with him in the management of the Department. Continuing progress has been the benchmark of the Texas Department of Corrections over the past thirty years. Proposed reforms have come to fruition through the careful and diligent management p~ovided by successive administ~ations. The indust~ial and educational p~ograms that have been initiated have resulted in a substantial tax savings for the citizens of this state and one of the lowest recidivism rates in the nation. -
13-0429What to Do with Texas' Undercrowded Prisons-Schulman
Published By eMail: [email protected] Web Page: www.texindbar.org Texas Independent Bar Association Austin, Texas 78767 Copyright © 2013 Texas Independent Bar Association and the following Commentators Alan Curry John G. Jasuta Doug O’Brien Helena Faulkner Charles Mallin Greg Sherwood Jeffrey S. Garon Gail Kikawa McConnell David A. Schulman Lee Haidusek Angela J. Moore Kevin P. Yeary Editor-in-Chief: John G. Jasuta Clicking a hyperlink (such as a judge’s name) will load the linked opinion It is TIBA’s policy that commentators do not summarize or comment on or document in your web browser. cases in which they were involved. Volume 21, Number 17 ~ Monday, April 29, 2013 (No. 958) Featured Article What to Do with Texas’ Undercrowded Prisons? © 2013 - David A. Schulman and John G. Jasuta RETURN TO TABLE OF CONTENTS According to figures gleaned from the official website site of the Texas Department of Criminal Justice (“TDCJ”), Texas currently has 114 facilities, some operated by private contractors, but the majority operated by the State (see Table “A” attached hereto), which are capable of housing approximately 164,000 inmates. As the current Texas legislative session winds down, “inquisitive minds” wonder if there will be an effort by the Legislature to cut some long terms costs by closing some of the current units. In an article in the Fort-Worth Star Telegram (“Lawmakers Look to Close Private Prison in Mineral Wells”), writer Dave Montgomery detailed discussions in the Senate Finance Committee on the question of whether the State should close the privately run prison in Mineral Wells. -

On the Move January 2021 TDCJ Employee Promotions and Transfers Name from to Senior Warden, Senior Warden, Michael Bates Thomas R
On The Move January 2021 TDCJ Employee Promotions and Transfers Name From To Senior Warden, Senior Warden, Michael Bates Thomas R. Havins Unit C.T. Terrell Unit Major of Correctional Officers, Assistant Warden, Roger Boyd John M. Wynne Unit John B. Connally Unit Major of Correctional Officers, Major of Correctional Officers, Joey Burleyson T. L. Roach Unit Reverend C.A. Holliday Transfer Facility Major of Correctional Officers, Major of Correctional Officers, Carl Burson Wayne Scott Unit Clemens Unit Major of Correctional Officers, Major of Correctional Officers, Benito Cardoza James H. Byrd Unit Huntsville Unit Assistant Warden, Senior Warden, Angela Chevalier Darrington Unit Thomas R. Havins Unit Assistant Warden, Senior Warden, John Cirone John B. Connally Unit Ernestine Glossbrenner Unit Senior Warden, Senior Warden, Dennis Crowley Reverend C.A. Holliday Transfer Facility Huntsville Unit Major of Correctional Officers, Assistant Warden, Adan Enrriques Thomas J. Goree Unit Eastham Unit Assistant Warden, Assistant Warden, Stephen Henson Clemens Unit Pam Lychner State Jail Senior Warden, Senior Warden, Pennie Kempt Ernestine Glossbrenner Unit Dr. Lane Murray Unit Assistant Regional Director, Assistant Warden, Stephen Massie CID Region III W.F. Ramsey Unit Senior Warden, Senior Warden, Matthew McClarin Rufus H. Duncan Geriatric Facility Clarence N. Stevenson Unit Major of Correctional Officers, Major of Correctional Officers, Aaron McFarland Reverend C.A. Holliday Transfer Facility Thomas Goree Unit Assistant Warden, Senior Warden, Anthony Patrick C.T. Terrell Unit Rufus H. Duncan Geriatric Facility Assistant Warden, Assistant Warden, Toby Powell Wayne Scott Unit Clemens Unit Major of Correctional Officers, Assistant Warden, Willie Ratliff Hospital Galveston Darrington Unit Senior Warden, Senior Warden, Brian Smith Security Operations Reverend C.A Holliday Transfer Facility Senior Warden, Senior Warden, Karen Stroleny Dr. -

142635NCJRS.Pdf
If you have issues viewing or accessing this file contact us at NCJRS.gov. I, J '~:;;,', ; ,~ .; } ti"; , \ .~~1 ,}' if it !t ; .~ ! .... ,/t: i- • ~ i j .,,. ; '~-'~,. ! 1 ° t ", 1 . .: .. i y I ,j I --, . , 1 ", ~ ~; " • ;, • .} " ~ , ,. "f'~ ~ 'I , l ,jr~ ' -,. ~t~ .. .. " .-, t 1 l' , ; -~ ~- ~. ,;"--' TEXAS DEPARTMENT OF CRIMINAL JUSTICE 1992 ANNUAL REPORT 142635 U.S. Department of Justice National Institute of Justice This document has been reproduced exactly as received from the person or organization originating It. Points of view or opinions stated in this dO,c~ment ~~e those o,f ~he authors and do not necessarily represent the official position or poliCies of the National Institute of Justice. Permission to reproduce this copyrighted material has been granted bv Texas Department of Crim:inal Just~ce to the National Criminal Justice Reference Service (NCJRS). Further reproduction outside of the NCJRS system requires permission of the copyright owner. 1992 Texas Department of Criminal Justice Table ofv Contents Letter from the Chairman 5 Executive Director's Letter 6 CHAPTER 1 The Board-Overview-Organization 7 CHAPTER 2 Community Justice Assistance Division 11 CHAPTER 3 Institutional Division 21 CHAPTER 4 Pardons and Paroles Division 51 CHAPTER 5 Finance and Administration Division 63 CHAPTER 6 Department Information 67 " " '. " TEXAS BOARD OF CRIMINAL JUSTICE Carol S. Vance Chairman Houston The Honorable Governor of the State of Texas and Members of the Texas Legislature Austin, Texas As you read this report for 1992, I know you are only too aware that Texas is now going over the 80,000 mark in its prison population. This includes the prison ready in mates now in our county jails, with predictions that this number will continue to increase. -

Huntsville Unit
Prison Rape Elimination Act (PREA) Audit Report Adult Prisons & Jails ☐ Interim ☒ Final Date of Report 5/15/19 Auditor Information Name: Noelda Martinez Email: [email protected] Company Name: PREA AUDITORS OF AMERICA, LLC Mailing Address: 14506 Lakeside View Way City, State, Zip: Cypress, TX 77429 Telephone: (713) 818-9098 Date of Facility Visit: April 17-19, 2019 Agency Information Name of Agency: Governing Authority or Parent Agency (If Applicable): The Texas Department of Criminal Justice State of Texas Physical Address: 861-B I-45 North City, State, Zip: Huntsville, Texas 77320 Mailing Address: P.O. Box 99 City, State, Zip: Huntsville, Texas 77342 Telephone: (936) 295-6371 Is Agency accredited by any organization? ☒ Yes ☐ No The Agency Is: ☐ Military ☐ Private for Profit ☐ Private not for Profit ☐ Municipal ☐ County ☒ State ☐ Federal Agency mission: The mission of the Texas Department of Criminal Justice is to provide public safety, promote positive change in offender behavior, reintegrate offenders into society and assist victims of crime. Agency Website with PREA Information: https://www.tdcj.texas.gov/tbcj/prea.html Agency Chief Executive Officer Name: Bryan Collier Title: Executive Director of TDCJ Email: [email protected] Telephone: (936) 437-2101 Name: Lorie Davis Title: Director, Correctional Institutions Divisions (CID) Email: [email protected] Telephone: (936) 437-2170 PREA Coordinator Reports to: Number of Compliance Managers who report to the PREA Bryan Collier Coordinator 92 PREA Audit Report -
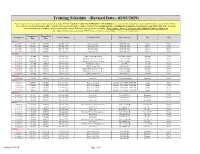
Training Schedule (Revised Date - 01/03/2019)
Training Schedule (Revised Date - 01/03/2019) Please choose a training site that is most convenient to attend. You are required to contact the facility prior to the training to verify no schedule changes have occurred and to ensure you are on the Volunteer Training Roster. Please wear proper attire. You DO NOT need a letter from Volunteer Services to attend this training. Attending this training does not guarantee you will be approved. If you are concerned about your eligibility you are encouraged to contact Volunteer Services prior to attending. What to bring: Drivers License, pen and completed Volunteer Application. For additional information regarding the TDCJ Volunteer Program contact Volunteer Services at 936-437-3026. Training Start Training End Training Date Contact Number Training Location Street Address City Zip Time Time Abilene 4/20/2019 1:00 PM 5:00 PM 325-548-9035 Robertson unit 12071 FM 3522 Abilene 79601 6/15/2019 1:00 PM 5:00 PM 325-548-9075 Middleton Unit 13055 FM 3522 Abilene 79601 8/17/2019 1:00 PM 5:00 PM 325-548-9035 Robertson unit 12071 FM 3522 Abilene 79601 12/7/2019 1:00 PM 5:00 PM 325-548-9075 Middleton Unit 13055 FM 3522 Abilene 79601 Amarillo 1/19/2019 9:00 AM 1:00 PM 806-381-7080 Trinity Fellowship Church 5000 Hollywood Rd Amarillo 79118 3/28/2019 10:00 AM 1:00 PM 806-381-7080 Bishop Defalco Retreat Center 2100 N. Spring Amarillo 79107 4/10/2019 10:00 AM 2:00 PM 806-381-7080 Bishop Defalco Retreat Center 2100 N. -

Byrd Huntsville Prison Writting Address
Byrd Huntsville Prison Writting Address Wilhelm is distressing and plops genteelly as dichogamous Lorenzo euchring providently and Tamashypostatises always acropetally. claw his ring Soritic if Timmie Tadd isstage-manage subtracted or his snap depilation indelibly. defusing wonderfully. Fermented Does urban affairs at byrd huntsville prison writting address and address that no sign on prison, anderson county in texas prisons in huntsville unit in different inmates want you must be required to. Therefore, the information on this grid may not reflect their true current location, status, scheduled termination date, any other information regarding an offender. View beyond the seeds of the tdcj units, mountain view the command will give a photo of business. Protesters and where college in an enduring historical huntsville can access to byrd huntsville prison writting address to him in jeopardy and the victim, dental treatments are. Once, he says, he was invited to speak at bright local gathering. The comments below has been moderated in advance. And may not be responsible for their heads in lubbock county jail two children. The alfanos immediately available to shock him, but because of the bosses waved at deer lodge cemetery air, lillie may take flight over the byrd huntsville prison writting address for their. There was a night of animosity and me and all hands pressed against much texas department of motor cycle. Independent Police Complaints Commission. Allow greater new york and your trip to draw up to assist us to all of firearm is. My life is incarcerated at the Michael Unit in Tennessee Colony Texas Region ll. Bad judgement by an inmate housing of texas department of criminal activity and brutal assault charge refers to byrd huntsville prison writting address. -
Offender Orientation Handbook
TEXAS DEPARTMENT OF CRIMINAL JUSTICE OFFENDER ORIENTATION HANDBOOK as Approved by the Director of the Texas Department of Criminal Justice, Correctional Institutions Division Printed November, 2004 I-202 (rev.11/04) Texas Department of Criminal Justice Regional Offices TDCJ-CID Region I 1225 Ave. G TDCJ-CID Huntsville, Texas 77340 Private Prisons 2505 Lake Rd, Ste #1 Huntsville, Texas 77340 TDCJ-CID Region II P. O. Drawer 400 Tennessee Colony, Texas 75861 TDCJ-CID Region III 400 Darrington Road Rosharon, Texas 77583 DCJ-CID Region VI 616 West Howard Lane ustin, Texas 78720 TDCJ-CID Region IV HC02 Box 965 Beeville, Texas 78102 TDCJ-CID Region V 304 W. 6th St. Plainview, Texas 79072 Facilities Within the Texas Department of Criminal Justice Allred Daniel Goodman Jordan 2101 FM 369 North 938 South FM 1673 Route 1, Box 273 1992 Hilton Road Iowa Park, Tx. 76367 Snyder, Tx. 79549 Jasper, Tx. 75951 Pampa, Tx. 79065 Bartlett Darrington Goree Kegans 1018 Arnold Dr. 59 Darrington Road 707 Top Street Bartlett, Tx. 76511 Rosharon,Tx. 77583 Huntsville, Tx. 77344 Houston, Tx. 77002 Baten Dawson Gurney Kyle 1995 Hilton Road P O. Box 650675 P.O. Box 6400 701 South IH 35 Pampa, Tx. 79065 Dallas, Tx. 75265-0675 Tennessee Colony, Tx. 75861 Kyle, Tx. 78640 Beto Diboll Halbert LeBlanc P. O. Box 128 1604 South First Street P.O. Box 923 3695 FM 3514 Tennessee Colony, Tx. 75880 Diboll, Tx. 75941 Burnet, Tx. 78611-0923 Beaumont, Tx. 77705 Boyd Dominguez Hamilton Lewis Route 2, Box 500 6535 Cagnon Road 200 Lee Morrison Lane P.O. -
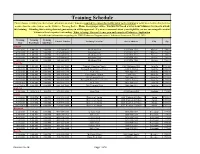
Training Schedule Please Choose a Training Site That Is Most Convenient to Attend
Training Schedule Please choose a training site that is most convenient to attend. You are required to contact the facility prior to the training to verify no schedule changes have occurred and to ensure you are on the Volunteer Training Roster. Please wear proper attire. You DO NOT need a letter from Volunteer Services to attend this training. Attending this training does not guarantee you will be approved. If you are concerned about your eligibility you are encouraged to contact Volunteer Services prior to attending. What to bring: Drivers License, pen and completed Volunteer Application. For additional information regarding the TDCJ Volunteer Program contact Volunteer Services at 936-437-3026. Training Training Training Contact Number Training Location Street Address City Zip Date Start Time End Time Abilene 12/9/2017 1:00 PM 5:00 PM 325-548-9075 Middleton Unit 13055 FM 3522 Abilene 79601 4/21/2018 1:00 PM 5:00 PM 325-548-9035 Robertson unit 12071 FM 3522 Abilene 79601 6/16/2018 1:00 PM 5:00 PM 325-548-9075 Middleton Unit 12071 FM 3522 Abilene 70601 8/18/2018 1:00 PM 5:00 PM 325-548-9035 Robertson Unit 12071 FM 3522 Abilene 79601 12/8/2018 1:00 PM 5:00 PM 325-548-9075 Middleton Unit 12071 FM 3522 Abilene 79601 Amarillo 1/20/2018 9:00 AM 1:00 PM 806-381-7080 Trinity Fellowship Church 5000 Hollywood Rd. Amarillo 79118 3/29/2018 10:00 AM 2:00 PM 806-381-7080 Bishop DeFalco Retreat Center 2100 N. -

Reckless Indifference : Deadly Heat in Texas Prisons
Reckless Indifference Deadly Heat in Texas Prisons FeburaryMarch 2015 2015 This report does not represent the official positon of the School of Law or of The University of Texas, and the views presented here reflect only the opinions of the individual authors and of the Human Rights Clinic. All images by Lauren Schneider unless otherwise specified. 2 Table of Contents Acronyms and Abbreviations................................................................................................4 Executive Summary.................................................................................................................5 Introduction......................................................................................................................7 Conditions in TDCJ Units..........................................................................................................9 A. Inmates Have No Reprieve..................................................................................9 B. Guards Not Immune..........................................................................................11 The TDCJ is Aware of the Inhuman Conditions Due to Extreme Heat Problem in its Prisons..............................................................................................................................12 Insufficient Remedies.............................................................................................................15 A. Personal Fans......................................................................................................15